Introduction
Fibromyalgia (FM) is a disease of unknown origin that affects approximately 5% of the population, mainly young women [1]. To date, the precise cause of FM is unknown [2].
The symptoms associated with FM significantly affect the patient’s quality of life and can result in extensive use of healthcare services [3]. Fibromyalgia does not have a uniform disease course, with many patients describing exacerbations or sudden increases in their symptoms throughout the course of the disease [4, 5]. These exacerbations are commonly referred to by patients and the professionals who treat them as “flares” [4–6]. And although they are commonly discussed in consultations by patients, there are very few studies that have defined their characteristics.
The purpose of this study is to determine how often these outbreaks occur in a large group of patients in our clinics, when these patients are followed up continuously for 6 months. We also aimed to find out what factors these exacerbations were related to, how they occurred, and what measures the patients took to alleviate the flares.
Material and methods
Over a 2-year period, between January 2019 and January 2021, a total of 124 patients were recruited who were willing to record in a diary if over a 6-month period they experienced any obvious worsening in their symptoms, or symptoms other than their usual symptoms appeared. This was a closed, prospective, longitudinal study with no control group. As there is no agreed definition for the term FM flare, we relied on previous studies that had described this condition [4–6]. They were to record the onset of thecondition, possible triggers, clinical presentation, factors that alleviated or improved symptoms, and the end of the flare-up.
The Medline, PubMed and Scopus databases were used for the previous literature review.
Participants
Participants had a diagnosis of FM that was confirmed by medical history review. To be eligible to participate in this study, all participants had to be 18 years of age or older. No quota of women or men was determined a priori, in order to keep the sample as random as possible.
Patients were excluded if they had other illnesses that in the opinion of the researchers could interfere with the results, such as major psychiatric or neurological illnesses, cancer or other terminal illnesses.
Procedure
All patients who agreed to participate were asked to record clinical changes that occurred during the 6 months of the study. Worsening of less than 24 hours duration was not taken into account. Patients were not instructed as to what triggers, symptoms or measures were usually taken in these cases, so as not to interfere with the final results.
Office Excel 2021 was used for data processing. All continuous data were expressed as means, standard deviations, ranges or percentages. As this is a descriptive study, there is no statistical significance.
Results
Of the total of 124 patients who were instructed to collect data, 92 patients submitted their diaries. The most frequent reasons for abandonment of follow-up were: failure to attend the review (n = 14), inconsistent or incomplete answers (n = 9), voluntary withdrawal from the study (n = 9).
The mean age was 47.8 years (SD 17, range 19–78 years). The vast majority were female (94.6%) and white (96%). Seventy-six percent were married or cohabiting, 16% divorced and 8% single. Thirty-six percent were working, 32% were on sick leave or had a permanent disability, and another 32% were homemakers. Regarding educational level, 36% had secondary or university education, 58% had primary education, and 6% had no basic education.
Number and duration of flares
A remarkable aspect was that almost half of the study time was conducted during the global coronavirus pandemic, with a period of confinement in our country of 14 weeks included in the study time. The number and duration of flares did not vary significantly, either during the pandemic or during confinement, but the triggers did, as we discuss below.
A total of 189 flares were counted during the study; 23 patients (25% of the total studied) reported no clearly defined outbreaks, only small fluctuations in their usual state; 69 patients (75%) reported at least one outbreak; of these, 35 patients (38%) reported only one outbreak, 22 patients (24%) reported 2 outbreaks, 30 patients (32.6%) described 3 or more outbreaks. The mean was 2 outbreaks in 6 months, SD ±1.2 (range 0–18).
To calculate the duration of flares, we took into account those that started and ended during the study period, with a mean of 11 weeks, SD 13 weeks and a range of 1–20 weeks. Therefore, 8 outbreaks that had not ended by the end of the study were not counted.
Triggers of flares
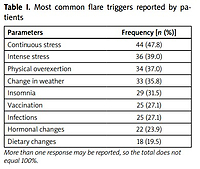
The causes to which patients related their outbreaks are listed in Table I. The most frequent cause, which was reported by more than half of the patients, was sustained stress (stress lasting more than 1 month, e.g., ongoing bullying at work) followed by sufficiently intense acute stress (less than 1 month but experienced as high intensity, e.g., the death of a family member or a traffic accident).
Table I
Most common flare triggers reported by patients
Other reasons given were physical overexertion (at work, social events and even a pleasant trip). More than 1/3 of the patients related their outbreaks to changes in the weather, especially when these occurred suddenly, and especially changes from hot to cold, including seasonal changes. Lack of sleep was also commonly reported, although as discussed later, the interrelationship between FM and sleep is bidirectional. Vaccinations, especially those related to coronavirus, were mentioned in a high percentage of cases as a possible trigger for the outbreak, as were concomitant infections, with COVID-19 again being the main agent involved. Hormonal changes, especially menstruation, especially if it is very painful, could also cause an outbreak. Finally, dietary changes, especially if these were radical, such as exclusion diets, or introduction of previously excluded foods, were also associated with 20% of the outbreaks.
When we analysed the results for the pandemic period, compared to the rest of the time, we found decreases in the percentages of physical overexertion (25% less), vaccinations (63% less) and infections (71% less). On the other hand, there were increases in intense stress (33% more) and insomnia (24% more).
Symptoms during flares
The first question asked was whether the symptoms experienced by patients during outbreaks were the same as their usual symptoms or whether they differed in any way, apart from frequency. In general, they reported that the clinical features were very similar to their usual day-to-day life, but more intense and disabling. Generalised pain, fatigue, cognitive impairment with deterioration of concentration (brain fog/fibro fog) and sleep problems were observed in almost all patients. However, as we have previously explained, sleep disorders can be both a trigger and a symptom of this disease. The relative frequencies are shown in Table II.
Table II
Most common symptoms in flares
Some symptoms not reported by the patients during the rest of their days, such as marked weakness or “flu-like” symptoms (but without fever), were described quite frequently. The rest of the symptoms did not differ much, except in intensity, from the rest of their usual days.
Measures taken to alleviate flares
The most frequently repeated measure was to increase rest periods (Table III) – if the patient was working, requesting temporary sick leave, and if not working, increasing time at home and reducing social activities. The second measure was to increase the intake of medication, mainly analgesics, although they asked their doctors to prescribe other types of drugs, mainly neuromodulators (antidepressants or antiepileptics) and opiates. Half of the patients used physical therapies, such as massage, acupuncture or physiotherapy. Almost half tended to use complementary therapies, such as natural remedies, herbs, vitamins or dietary supplements. More than 1/3 tried to modify their dietary habits, such as exclusion or avoidance diets, prolonged fasting or a diet low in short-chain carbohydrates (sugars) that is poorly absorbed in the gut, which is knows as the FODMAP (fermentable oligo-, di- and mono-saccharides and polyols) diet.
Table III
Actions most commonly taken by patients after a flare
Other, less frequently used measures were psychotherapy, physical exercise or hydrotherapy. Eleven percent of patients decided not to make any changes in their lives, waiting for the “storm” to pass. These patients were those who had previously tried other measures in other flares, with little or no efficacy.
Discussion
Fibromyalgia, despite being a chronic disease, is not a uniform disease in its evolution, but exacerbations occur over time, sometimes with a known trigger, at times without [7]. Within this fluctuating course, very often patients and clinicians who treat this process describe a clear worsening, continued over time, commonly referred to as “flares”.
Although the term flare is commonly used, we have found only one study in the medical literature that has specifically evaluated the presence and characteristics of FM flares. Since this paper published in 2014 by Vincent et al. [6], no further study has described the characteristics of FM flares. The previously mentioned study was a survey with open-ended questions to a specific group of FM patients.
Our prospective study describes the characteristics over time of patients with a flare or worsening, and quantifies the number and duration of flares during the follow-up period.
We observed that two out of three patients had at least one outbreak during the follow-up period (6 months), with a mean of two outbreaks in that time. The average duration of the flares was 11 weeks. By far the most frequent flare triggers were as follows: stress, then physical overexertion, and in 4 of the cases, it was related to changes in the weather. The latter relationship has been studied previously in several studies, and seems to be associated mainly with lowering of atmospheric pressure [8, 9].
They also described patients relating their worsening to hormonal changes (mainly menstruation) and dietary changes (especially certain foods, such as milk or gluten). These triggers have been investigated in previous studies [10, 11].
A remarkable and understandable fact is that, after the start of the global COVID19 pandemic, the percentages of stress and insomnia as triggers increased markedly, by 33% and 24% respectively.
Regarding the clinical features of the flares, the symptoms did not differ from those usually reported by patients; they were only more pronounced and longer lasting. There were some exceptions, such as “flu-like” symptoms without fever, or general weakness, both of which have been described previously [6].
The most frequent measures taken by patients were rest, taking analgesic or neuromodulatory medications, and physical therapies, such as physiotherapy or acupuncture, all of which were performed in more than half of the patients. However, more than one third of the patients used complementary medicines (mainly natural compounds), and another third used dietary measures (mainly food restrictions).
Our results are consistent with the few previous articles that mention FM flares in any way [4–6]. As in other studies, stress, both sustained and acute, was identified as the main trigger for flares. The symptoms were interrelated, with flares of one symptom often exacerbating another [12]. In addition, in an attempt to explain why flares occur, some authors relate such exacerbations to a central sensitization phenomenon [13].
Study limitations
Although this study helps to better understand how FM behaves in its evolution, it certainly has some limitations. First, it was carried out in a group from the same geographical area, which may not be extrapolated to other societies or cultures. Second, each patient’s description of their flare may be different from another patient. That is, what some patients understand as an outbreak may be different for others. And third, due to the limited sample size, sub-analysis by gender, age groups, educational level, or marital status, among other variables, was not performed.
Therefore, we believe that it would be desirable to extend the sample to more patients, to carry out these secondary analyses, and to continue to study these natural exacerbations, known as flares, in greater depth with more specific studies.
Conclusions
Despite the usual complaint by patients that their disease manifests significant acute worsening, this fact has not been given sufficient interest by the scientific community, and has not been studied quantitatively as it deserves. We describe in this article how often and for how long flares occur, as well as what triggers patients relate them to, what clinical symptoms they have, and how they try to alleviate the symptoms.
Future research should continue to quantify and explain why these episodes occur, and whether they can be prevented or treated in any appropriate way.