Introduction
Atherosclerosis is a process whose onset can be observed even in the foetal period. A number of risk factors, such as hyperlipidaemia, hyperhomocysteinaemia, arterial hypertension, hyperuricaemia, smoking, metabolic syndrome, hypertriglyceridaemia, and diabetes, accelerate the progression of atherosclerotic lesions leading to the development of atherosclerotic cardiovascular disease (ASCVD) [1].
Atherosclerotic cardiovascular disease is defined as coronary artery disease (CAD), cerebrovascular disease, or peripheral arterial disease of atherosclerotic origin. This disease represents the number one cause of morbidity and mortality worldwide. The number of patients with cardiovascular diseases in the world in 2019 was 523 million, while the number of deaths due to them reached 18.6 million [2].
Atherosclerosis – general look on pathogenesis
The pathogenesis of atherosclerosis is a multifactorial process involving large and medium-sized arteries, the head of the aorta, and coronary vessels, and it occurs especially in the places of their branches and bifurcations. According to modern concepts, atherosclerosis is a consequence of a long-term defence reaction of the organism, which increases with time, in the form of a chronic inflammatory response, leading to degenerative and productive changes in the inner and middle layers of the arteries. Atherosclerosis is a complex inflammatory disease involving aberrant immune and tissue-healing responses, which begins with endothelial dysfunction and ends with plaque development, instability, and rupture, which leads to MI, stroke, or critical ischaemia of the lower limbs [3].
Atherosclerosis in patients with rheumatological diseases
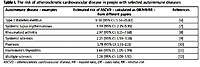
Many authors indicate that atherosclerosis is an auto-inflammatory disease but also an autoimmune disease, because it produces antibodies to oxidized low-density lipoprotein (oxLDL) [4, 5]. It should be noted that the progression of atherosclerosis is particularly pronounced in patients with autoimmune diseases (Table I).
Table I
The risk of atherosclerotic cardiovascular disease in people with selected autoimmune diseases
| Autoimmune disease – examples | Estimated risk of ASCVD – calculated as OR/HR/RR – from different papers | References |
|---|---|---|
| Type 1 diabetes mellitus | 9.38 (95% CI: 5.56–15.82) | [6] |
| Systemic lupus erythematosus | 3.39 (95% CI: 2.15–5.35) | [7] |
| Rheumatoid arthritis | 2.97 (95% CI: 1.15–7.68) | [8] |
| Systemic sclerosis | 2.25 (95% CI: 1.59–3.18) | [9] |
| Psoriasis | 1.78 (95% CI: 1.51–2.11) | [10] |
| Hashimoto’s thyroiditis | 1.44 (95% CI: 1.05–1.99) | [11] |
| Multiple sclerosis | 1.28 (95% CI: 1.09–1.51) | [12] |
Based on the data presented in Table I, it should be emphasized that autoimmune diseases are a strong independent risk factor for ASCVD. It should be stressed that the presence of autoimmune inflammatory diseases (such as rheumatoid arthritis, systemic lupus, or psoriasis) is an indication for early and regular lipid profile control and should be included in the cardiovascular risk stratification [13].
Importantly, systemic autoimmune diseases and atherosclerosis share common pathogenic pathways (chronic inflammatory background mediated by the toll-like receptors and inflammasome Nucleotide-binding oligomerization domain, Leucine rich Repeat and Pyrin domain containing 3/interleukin 1 (NLRP3/IL-1) pathways as seen in auto-inflammatory diseases and endothelial dysfunction) [5]. Moreover, autoantibodies (an essential component of autoimmune diseases) may ultimately cause structural and irreversible arterial wall damage with subsequent atherosclerotic plaque development and rupture [5]. It is worth adding that oxLDL and anti-β2-glycoprotein I (β2-GPI) are both inflammatory (innate) and immunogenic (adaptive) molecules.
One possible role for these molecules is that they can serve as biological linkers to link the progression from chronic inflammation to a complete autoantibody response in the later stages of atherosclerosis. When autoantibodies are present, rheumatoid arthritis patients have an accelerated atherosclerosis compared to rheumatoid arthritis patients who do not have these antibodies. Similarly, autoantibodies in systemic lupus erythematosus exacerbate atherosclerosis [5].
In rheumatic diseases, atherosclerosis can be accelerated by both systemic inflammation and local vasculitis. Levels of pro-inflammatory cytokines such as TNF-α, IL-6, IL-17, and IFN1 are often chronically elevated in rheumatic diseases, further exacerbating endothelial dysfunction, macrophage activation, and thrombosis [3]. A characteristic feature of rheumatological diseases is the production of autoantibodies, some of which may be deposited directly in the lesions of the vessel wall, intensifying the progression of atherosclerosis. T and B lymphocytes play a key role in the pathogenesis of rheumatological diseases. It is worth mentioning that a specialized population of T lymphocytes, CD4+ CD28- cells, was isolated from inflammatory lesions of the synovium and ruptured plaque [3].
An important factor contributing to the intensification of atherosclerosis progression in rheumatological diseases is the presence of various genetic polymorphisms, such as NFKB1–94ATTG ins/del polymorphism, HLA-DRB1*0404 shared epitope allele, and a TNF-α rs1800629 gene polymorphism [3].
From a clinical point of view, the influence of rheumatological disease treatment on the risk of ASCVD is significant. Ideally, such a therapy would work to reduce the risk of ASCVD. For example, in a study by Ozen et al. [14] was compared the effects of biologic disease-modifying anti- rheumatic drugs (bDMARD) and conventional synthetic DMARD (csDMARD) on incident cardiovascular disease in patients with rheumatoid arthritis. Cardiovascular risk reduction with TNF inhibitors (HR 0.81, 95% CI: 0.71 –0.93) and abatacept (HR = 0.50; 95% CI: 0.30 –0.83) compared to csDMARD was demonstrated. Also, it was found that minimizing the use of glucocorticoids and optimizing the dose of methotrexate may improve cardiovascular outcomes in patients with rheumatoid arthritis [14].
Moreover, a study by Yang et al. [15] assessed the long-term effect of treating patients with systemic lupus erythematosus (SLE) with hydroxychloroquine (HCQ) on the risk of ASCVD. Decreased risk for CAD was found among SLE patients with a high usage of HCQ for at least 318 days (HR = 0.31; 95% CI: 0.12–0.76). A low risk for CAD was observed in SLE patients with a high cumulative dose of at least 100.267 mg HCQ (HR = 0.25; 95% CI: 0.09–0.66) [15].
Thus, patients with rheumatological diseases have an increased risk of ASCVD, which is a result of increased inflammation and autoimmune processes. Treatment of these conditions reduces the risk of ASCVD in this group of patients.
Conclusions
Atherosclerosis with its background in inflammation and autoimmunity processes is not only a pathology of the cardiovascular system. Lots of autoimmune and rheumatological conditions are currently viewed as risk factors for accelerated atherosclerosis. Thus, cardiovascular check-ups must be included in rheumatology practice. New methods of treatment and new data on some drugs influencing both cardiovascular and rheumatological diseases (like statins) are increasing our mutual recognition of both fields of medicine.