Dear Editor,
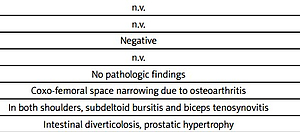
An 83-year-old male presented to our outpatient clinic with complaints of sudden bilateral pain in the scapular girdles, hip pain, low-grade fever, and general malaise without other joint involvement. Table I summarizes patient’s main clinical, laboratory and imaging findings.
Table I
Main clinical, laboratory and imaging data at the time of first referral
[i] ANA – anti-nuclear antibodies, ANCA – anti-neutrophil citoplasmic antibodies, ACPA – anti-citrullinated protein antibodies, BMI – body mass index, CRP – C-reactive protein, ESR – erythrocyte sedimentation rate, Hb – haemoglobin, MS – morning stiffness, RS3PE – remitting symmetrical seronegative synovitis with pitting edema, n.v. – normal values, RF – rheumatoid factor, US – ultrasound, VAS – Visual Analogue Scale.
The patient provided written consent for publication.
According to the 2012 European Alliance of Associations for Rheumatology/American College of Rheumatology (EULAR/ACR) classification criteria [1], our patient scored 5 points (hip pain – 1 point; absence of rheumatoid factor or citrullinated antibodies – 2 points, absence of other joint involvement – 1 point, bilateral subdeltoid bursitis and biceps tenosynovitis – 1 point) and was diagnosed with polymyalgia rheumatica (PMR).
We started treatment with 12.5 mg/day prednisone. While erythrocyte sedimentation rate (ESR), C-reactive protein (CPR) and hip pain improved (ESR = 28 mm/h; CPR = 2 mg/dl), bilateral pain in the scapular girdles, general malaise and low-grade fever persisted even after doubling the prednisolone dose. A total body computed tomography (CT) suggested the presence of a prostate cancer. A radical prostatectomy confirmed the first diagnostic suspicion and favour the complete resolution of these clinical manifestations.
Polymyalgia rheumatica is a common inflammatory rheumatic disease in the elderly. Although no diagnosis test is available, the diagnosis is based on clinical and laboratory findings, with morning stiffness (MS) lasting > 45 minutes being one of the most significant features [2, 3].
According to the 2012 EULAR/ACR classification criteria, a patient aged 50 years or older complaining of bilateral shoulder aching associated with elevated ESR and/or CRP, may be categorized as having PMR if he has a minimum score of 5 when clinical and ultrasound (US) criteria are used [1].
This means that PMR categorization is possible even if MS does not last > 45 minutes, provided that all the other classification criteria are met. Polymyalgia rheumatica has been described as paraneoplastic syndrome, and some researchers have suggested that its prevalence may be underestimated in routine clinical practice [4–7].
The possibility that absence of prolonged MS can be a neoplastic warning has been scarcely reported in published literature. Niccoli et al. [8] reported three patients presenting with PMR-like manifestations, absence of prolonged MS, some atypical clinical findings, inefficacy of corticosteroids, and the absence of shoulder US pathological findings, which led to the diagnosis of renal cell carcinoma.
In our patient, the absence of long-lasting MS and the partial efficacy of glucocorticosteroids (GCs) were the only atypical findings, and PMR was the onset of prostate cancer. A systematic review argued that there was little evidence to suggest which presenting features may be associated with cancer [9]. However, the presence or absence of prolonged MS at the time of diagnosis of PMR was not evaluated.
The EULAR/ACR collaborative study indicated that prolonged MS lasting more than 45 minutes duration had an odds ratio > 5, much higher than that of the other assessed factors. Therefore, its absence should raise serious diagnostic concerns. However, in the same study, among 125 patients with PMR, MS duration was not > 45 minutes or data were not available in 33 [1].
Further studies are required to evaluate an association between cancer and the absence of prolonged MS. Nevertheless, its association with a partial efficacy of GCs may justify the search for cancer.