Introduction
Fibromyalgia (FM) is a disease of unknown origin, affecting approximately 5% of the population, mostly young women [1]. According to some studies, 90% of people with FM use complementary medicine to control their symptoms [1].
The results show a higher acceptability of non-pharmacological treatments compared to pharmacological treatments, although the assessment of efficacy is similar [2]. Many patients find that food exacerbates their symptoms [3], so elimination diets can be both a diagnostic tool and a therapeutic intervention for people with a suspected food sensitivity or allergy [4]. They are clinically relevant not only for patients with functional gastrointestinal disorders, but also for those with conditions where symptoms are refractory and diagnosis is elusive. Elimination diets may help the clinician to make a diagnosis or to identify an underlying cause of symptoms. Although no particular diet has been found to have a significant impact in FM, they may be useful in improving gastrointestinal distress in certain FM patient populations [5].
So far, there is insufficient evidence to recommend a specific nutritional intervention for the treatment of FM [6], and no specific foods that may exacerbate or cause symptoms have been investigated [4].
The main purpose of this prospective study was to determine whether after applying a specific histamine intolerance test, and applying a diet of exclusion of those foods with high indices in the test, the symptoms typical of the disease improve.
Material and methods
A total of 84 patients with FM according to the 1990 ACR classification criteria [7] and the new 2010 diagnostic criteria [8] were recruited during the years 2019–2020, all of whom were women between 18 and 65 years of age. Patients with any other disease that could interfere with the results, e.g. coeliac disease, or patients following a vegetarian diet or already following an exclusion diet, were excluded from the analysis.
Forty participants underwent a food intolerance test by measuring direct basophil degranulation incubating overnight patients’ blood with different food allergen extracts – the 11 most commonly consumed food groups in the Mediterranean diet (Table I).
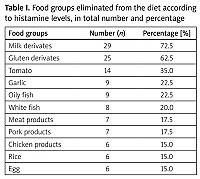
Table I
Food groups eliminated from the diet according to histamine levels, in total number and percentage
Histamine was measured as a marker of basophil degranulation by means of a commercial histamine assay kit. This test uses natural allergens. To analyse the results, a standard curve with known amounts of histamine is performed. The total blood histamine content and its basal release in the absence of food antigens must also be known. The results are expressed in terms of histamine release values when the patient’s blood is confronted with the battery of foods studied.
According to the results obtained, the foods that gave the highest histamine indices were completely excluded from the diet, under the supervision of a nutritionist. The remaining 44 patients were allowed to continue with their usual diet, explaining to all patients that they should not modify other parameters, such as medication, exercise or alternative therapies, during the 6 months of the study.
Prior to participating in the study there were no significant differences between the groups in terms of pharmacological and non-pharmacological therapies.
The assessment scales were those specific to FM, the pain Visual Analogue Scale (VAS, scored from 0 to 10) and the Fibromyalgia Impact Questionnaire – Spanish version [9] (FIQ, scored from 0 to 100), and the Gastrointestinal Symptom Rating Scale – Spanish version [10] (GSRS, scored from 0 to 7); for all of them, 0 indicates better health and higher values indicate worse health. Also the patients’ weight was measured at the start and end of the study (Table II).
Table II
Results of the means and confidence intervals (CI) of the biodemographic data, and different scales at the beginning (1) and end (2) of the study, with their statistical significance (p), both in the group that followed the exclusion diet and in the control group
Student’s t-test for paired samples was used as the main statistical method, with a significance of p < 0.05.
Results
After 6 months of follow-up, 32 out of 40 in the diet group and 35 out of 44 in the control group completed the study. The main reason for dropout in the first group was monotony of the diet, and in the second group dropout from follow-up. No side effects were reported in either group.
The foods excluded after histamine intolerance testing and their respective percentages are shown in Table I. The mean number of positive foods per patient was 3, with a range of 1 to 5. The most common combination was milk products and gluten-containing cereals (which occurred in 47% of the patients). At the end of the study there was variation in the scales studied as shown in Table II, being statistically significant (p < 0.05) for GSRS and total body weight, but not for VAS and FIQ.
When performing a sub-analysis of the parameters in the GSRS scale, the parameters that changed the most were: bloating, belching, constipation, bowel sounds and hunger pains. It is noteworthy that 3 patients who underwent the exclusion diet noticed an improvement not only in GSRS and body weight, but also in VAS and FIQ from the first days until the end of the study.
Discussion
There is growing interest in food intolerance problems that create non-specific abdominal complaints, in certain population groups, such as FM patients. However, studies to date on these patients with different dietary approaches have been contradictory [6]. It has been reported that 40% of FM patients consider that diet has a major influence on their symptoms, and 42% report an aggravation of their symptoms following the ingestion of certain foods [11].
In another study, 68% of patients were reported to use nutritional supplements in an attempt to improve symptoms [3]. Despite this, it is not known to date which foods cause such worsening [5], and there are no studies to date that specifically study these foods, only studies that eliminate foods based on what the patient assumes may be bad for them [12].
Our study attempts to make the link by means of a specific intolerance test, confronting the patient’s blood with certain common foods in our diet, mainly proteins, and measuring the elevation of blood histamine. We found a strong relationship between the exclusion of certain foods and releving digestive symptoms (including assesment of body weight) in patients after 6 months of follow-up. No significant improvements in other parameters were obtained, except in isolated cases of patients who reported a clear improvement in pain or fatigue.
A disproportionate amount of histamine in the body is suspected to be the result of the consumption of histamine-containing foods or beverages, and the reduced ability of enzymes to digest and degrade histamine [13]. In so-called histamine intolerance, impaired histamine degradation in the gastrointestinal tract causes functional, non-specific intestinal and extraintestinal discomfort [14]. Unbalanced and elevated histamine in intolerances seems to be the main consequence of ingestion of histamine-containing foods [15].
There is growing scientific evidence and studies supporting this idea [16]. However, standardised assessments and/or reliable laboratory tests are needed for the define diagnosis of histamine intolerance [13].
We propose this new specific histamine release test as a diagnostic and therapeutic method in FM patients suffering from various digestive disorders, and even in some cases extraintestinal disorders.
Study limitations
This work has the limitations of an observational study, with a small sample of patients, but it opens up an interesting avenue for future research. Therefore, although dietary aspects appear to be a promising complementary approach to the treatment of FM, more research is needed to provide the most effective strategies for the management of this disease.