Dear Editor,
The skin and gastrointestinal tract are the most involved organs in patients with systemic sclerosis (SSc). Gastrointestinal involvement was found in more than 90% of the patients, and every segment of the tract can be affected [1]. The small intestine is commonly affected in SSc patients, although clinical manifestations vary from asymptomatic to severe, including pseudo-obstruction, bacterial overgrowth and diarrhea [2]. They can be associated with disruption of the intestinal barrier that plays a vital role in control of the translocation of substances from the gut lumen into the bloodstream due to tight junctions. Tight junctions are regulated by zonulin. The serum level of zonulin is believed to be a marker of intestinal barrier permeability [3].
This letter reports the determination of serum zonulin level in 49 patients with SSc as compared to 23 healthy controls. The SSc patients (37 women, 12 men; aged 22–58 years) fulfilled ACR/EULAR classification criteria for SSc. Patients with disorders other than SSc and overlap syndromes were excluded from the study.
A venous blood sample was obtained in the morning after overnight fasting, and the serum was separated. The zonulin level was determined with a commercially obtained ELISA kit (Immunodiagnostik AG, Bensheim, Germany).
All other measurements were taken using routine procedures during an annual check-up of the patients. The study protocol was approved by the Ethical Committee of the Medical University of Silesia in Katowice (No. CBN/0052/KB1/31/1/22).
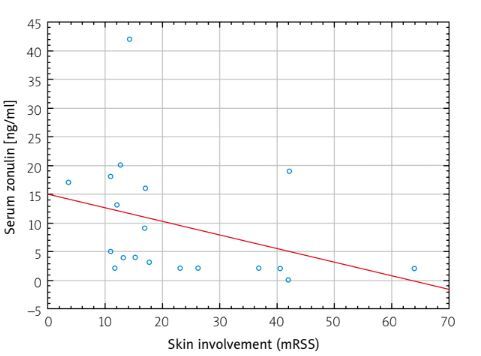
The serum zonulin level was lower in SSc patients as compared to healthy controls (14.3 [9.2–19.2] vs. 22.6 [17.3–31.0] ng/ml, p < 0.01, respectively). The SSc patients with earlier disease, i.e. > 6 years after the first non-Raynaud symptom, had a higher zonulin level than those with the disease lasting longer (for less than 6 years of overt disease = 16.9 ng/ml, more than 6 years = 12.4 ng/ml). A negative correlation was found between cutaneous involvement and zonulin level only in early forms of the disease (Fig. 1).
Fig. 1
Correlation between serum zonulin and skin involvement in SSc patients with overt disease lasting less than 6 years (r = –0.51, p < 0.03).
A negative correlation in all SSc patients was found between zonulin level and CRP level (r = –0.30, p < 0.04). There was a positive correlation between zonulin level and forced vital capacity (FVC) (r = 0.36, p < 0.03) in all SSc patients, while a positive correlation between zonulin level and diffusion lung capacity for carbon monoxide (DLCO) (r = 0.47, p < 0.02) was observed in the patients with diffuse SSc only.
There was no correlation between serum zonulin level and sex, age, body mass index, subgroup of SSc (limited vs. diffuse), and autoantibody profile. Unexpectedly, there was no correlation between symptoms and signs of gastrointestinal tract involvement evaluated with the UCLA SCTC GIT 2.0 questionnaire and serum zonulin level.
Zonulin has been suggested to be a marker of mucosal barrier integrity, but it should be interpreted with some caution. Application of other methods for determination of the intestinal barrier revealed inconsistent results in patients with SSc. A low level of zonulin may be associated with fibrosis of the intestinal wall and subsequent malabsorption [4]. It is interesting that patients with more severe and long-lasting disease had a lower zonulin level. It may be due to widespread fibrosis, dysbiosis as well as immune alterations affecting the intestine and its local immune system [5]. Further studies with simultaneous application of various methods of permeability measurement are needed.