Dear Editor,
Patients with inflammatory rheumatic diseases are at high risk for severe outcomes associated with coronavirus disease 2019 (COVID-19) due to the immune disturbances related to the disease, administration of immuno-suppressive drugs and comorbidities [1, 2].
IgG4-related (IgG4-RD) disease is a chronic inflammatory disease that can affect different organs and systems such as the pancreas, bile duct, major salivary glands, lacrimal glands, and retroperitoneum and lymph ducts [3]. IgG4-related disease is characterized by elevated serum IgG4 levels, neoplastic-like swelling of the affected organs, specific histopathological features, and good response to glucocorticosteroids (GCs) therapy. Recently, elevation of serum IgG4 was suggested as a predictor of mortality in hospitalized COVID-19 patients, raising the possibility that an immunological background predisposed to increasing IgG4 production may lead to a severe course of SARS-CoV-2 infection [4].
It is however difficult to consider IgG4 level as a marker due to its variability under conditions of a number of diseases [5]. There are only a few and in some aspects contradictory data in the literature on the course and prognosis of SARS-CoV-2 infection in IgG4-RD patients.
The letter reports the clinical course of SARS-CoV-2 infection of a patient who was followed up with IgG4 related disease and had received GCs therapy.
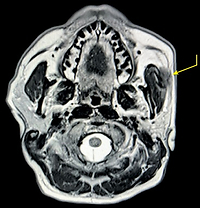
A 45-year-old male patient due to swelling of the left parotid gland had been seen by an otolaryngologist a year ago. Magnetic resonance imaging (MRI) was recommended and revealed a solid parotid mass was found (Fig. 1), and an excisional biopsy was performed.
The patient was referred to the rheumatological clinic because the pathological findings of the excised tissue indicated IgG4-RD. There were no symptoms and signs suggesting rheumatic disease in the medical history and physical examination. There were no symptoms rheumatic disease in the medical history and physical examination, however, a soft tissue swelling ine the left parotid gland was observed. Results of laboratory tests (ANA, ENA profile, ACPA, serum ACE, ANCA, and RF) were unaltered. Acute phase reactants were slightly elevated, erythrocyte sedimentation rate (ESR): 43 mm/h (normal range 0–20 mm/h), C-reactive protein (CRP): 7 mg/dl (normal range 0–5 mg/dl). Serum total IgG and IgG4 levels and IgG1/IgG4 ratio were slightly increased. Medication with GCs was administered (48 mg of prednisone daily).
Significant regression was observed in the follow-up, and significant regression and later disappearance of the mass within the parotic gland were revealed with ultrasonography examination. The GCs dose was gradually reduced and the patient continued management with 4 mg of prednisone daily.
Two months ago, the patient was admitted to the clinic with fever, dry cough, weakness, parotid swelling and muscular pain. There was a history of COVID-19 in his family, so the patient underwent a SARS-CoV-2 PCR test and was found to be infected. A mild increase in acute phase reactants was found. Thoracic computed tomography did not reveal any abnormality. A mass within the parotid gland was detected with ultrasound investigation, and a relapse of the previously diagnosed IgG4-RD disease was considered. Medication with anti-pyretic drugs, liquid and vitamins were administered according to recommendations for COVID-19 management. The relapse of IgG4-related disease was managed with 32 mg of prednisone daily.
Symptoms of both disorders regressed, and the PCR was negative after 15 days of treatment. Acute phase reactants determined one month later were normal, and almost complete regression was observed in the follow-up parotid nuclear magnetic resonance findings.
The patient, whose general condition is good, continues to be followed up in the outpatient clinic and was receiving a low dose of GCs.
Herein, we report disease activation in an IgG4-related patient in remission as a result of SARS-CoV-2 infection. COVID-19 is not a trifling viral infection; it may be a fatal disease resulting in acute respiratory distress syndrome, especially in patients with risk factors including reduced immunity [6].
Data on the course and prognosis of COVID-19 in IgG4-related patients are contradictory and limited. Chen et al. [7] reported SARS-CoV-2 infection in two of 91 IgG4-related patients, both of whom had fever and cough, and found no significant lung involvement. In a multicentre retrospective study, COVID-19 was detected in 32 (10%) of 305 IgG4-RD patients [8].
Fever, dry cough and dyspnoea were the most commonly reported manifestations. Eleven out of 32 patients with COVID-19 (34%) were hospitalized; two (6%) required admission to an intensive care unit and four (13%) died. According to the results of the study, it was speculated that the clinical course of COVID-19 is more severe in IgG4-related disease patients. In the reported case, COVID-19 clinical symptoms were similar to the general population. Activation of the primary disease was observed after the COVID-19, and was controlled with an increased dose of GCs.
It has been reported that during SARS-CoV-2 infection, high IgG4 serum levels are detected, and this has been suggested to be related to mortality [4, 5]. Specifically, a concentration of serum IgG4 > 700 mg/dl and an IgG4/IgG1 ratio > 0.05 were associated with a significantly increased mortality at a month interval. The mechanism of the relapse is not clear. The simplest explanation is that non-specific enhance of immune-inflammatory reaction by viral infection. Such phenomenon occurs in any kind of stimulation of the immune system. The other hypothetical mechanisms include a more expressed response to SARS-CoV-2 infection in individuals with higher IgG4 secretion.
On the other hand, it is possible that anti-IFN antibodies associated with impaired anti-SARS-CoV-2 immunity and severe COVID-19 pneumonia might also belong to the IgG4 subclass [9].
In conclusion, the results regarding the clinical course, susceptibility and prognosis of COVID-19 in IgG4-related disease patients are still contradictory and further studies in this field are needed.