Introduction
About 88% of patients with rheumatoid arthritis (RA) experience neck pain. Atlantoaxial instability, subaxial subluxation and vertical migration of the odontoid are diagnosed in respectively 33%, 21% and 14% of the community-based RA population and are associated with increased risk of myelopathy and mortality [1]. Clinical evidence of impending myelopathy and radiologic signs of craniocervical or atlantoaxial instability are indications for occipito-cervical fusion (OCF) [2].
Over the last 50 years, the OCF technique has evolved from simple onlay bone grafting [3] to independent occipital plating and cervical rod constructs [4]. Rigid fixation achieved with screws placed in the occipital squama, pedicles and lateral masses offers nearly a 100% rate of fusion and usually makes it possible to avoid postsurgical external immobilization [2]. The ultimate decision on application and duration of cervical immobilization after surgery depends on the surgeon’s personal judgement.
Hard collars, the halo vest, and the Minerva jacket after rigid OCF may be recommended for 2–3 months when the bone quality is poor, and/or in unreliable or extremely active patients [2]. Despite decreasing the risk of fixation failure, cervical collars are inherently associated with side effects including pressure sores, difficulty eating and hindered maintenance of a surgical wound [5]. Occipital pressure sores (OPS) are the most severe pressure lesions associated with the use of cervical collars and can reach stage IV and require extensive reconstruction [6]. The appearance of OPS is associated with pain and morbidity, increased antibiotic use, length of hospital stay and treatment costs [7].
Recommendations on OPS prevention are tailored for persons with acute trauma and patients in intensive care, as this population is at the highest risk of this complication [8–10]. Knowledge of OPS prevention in patients using collars after elective spinal surgery is lacking.
This report describes the case of a female patient who developed spinal infection involving a metal construct, as a complication of an OPS resulting from hard collar use after OCF. The subsequent systematic literature review aims to address the issue of OPS risk and prevention in persons using cervical collars after spinal surgery with special consideration of the specificity of preventive measures during a pandemic.
Material and methods
We performed a systematic search of Cochrane Central, EMBASE, PubMed Medline, SCOPUS and Web of Science databases for articles published up to 10 January 2022 in accordance with PRISMA requirements using key words and phrases related to OPS, cervical spinal surgery and use of collars. We applied the following search strategy:
Cochrane: (sore or ulcer) and (occipito or occipital) and pressure and (collar or orthosis),
EMBASE: (collar OR orthosis) AND pressure AND (occipital OR occipito) AND (sore OR ulcer OR ‘decubitus’/exp OR decubitus),
PubMed: (occipital or occipito) pressure (collar OR orthosis) (sore or ulcer),
SCOPUS: TITLE-ABS-KEY (occipital OR occipito) AND TITLE-ABS-KEY (pressure) AND TITLE-ABS-KEY (collar OR orthosis) AND TITLE-ABS-KEY (sore OR ulcer OR decubitus),
Web of Science: pressure (sore or ulcer or decubitus) (collar or orthosis) (occipito or occipital).
Reference lists from the retrieved articles and other related articles were also reviewed. To identify publications describing prevention of collar related OPS after cervical spine surgery, we applied the following inclusion criteria:
English language,
participants/populations: patients using collars after cervical spine surgery,
outcome: rate, stage, risk factors of OPS, method and efficacy of prevention and treatment.
Case description
A 61-year-old female patient admitted to an in-patient Rehabilitation Department on 14th May, 2020, 2 months after C0–C6 revision OCF carried out due to a destabilization of prior C0–C5 stabilization performed in September 2018 for occipito-cervical instability. When discharged from the Surgical Department, the patient was equipped with a Philadelphia collar and advised to wear it constantly for 3 months.
The patient had polyarticular juvenile idiopathic arthritis (JIA) diagnosed in childhood. In adulthood, the JIA diagnosis was change into RA. Pain and progressive deformities of peripheral joints preceded the occurrence of spinal involvement.
Cervical pain radiating to upper limbs started in the fifth decade of life. Due to the progression of the disease and deterioration of functional status the patient was subjected to numerous corrective procedures of the peripheral musculoskeletal system as well as C5–C6 anterior discectomy and fusion with a plate (2010). The patient in the past has been treated with methotrexate, sulfasalazine, hydroxychloroquine, cyclosporine, etanercept and oral glucocorticosteroids (GCs). The patient experienced gastrointestinal bleeding as a side effect of antirheumatic drugs. For this condition the patient underwent right-sided hemicolectomy (2008) complicated with anastomosis leakage. During abdominal revision surgery, the patient underwent splenectomy due to iatrogenic tear of the splenic capsule, followed by the excision of peritoneal adhesions and abdominal hernioplasty performed 6 years before the recent admission.
The patient was also diagnosed with recurrent bilateral deep vein thrombosis of lower limbs, Parkinson’s disease, chronic anaemia requiring multiple blood transfusions and symptomatic osteoporosis with vertebral fractures at levels Th6 and Th8–L3, fractures of bilateral ischial ramus and left-sided pubic ramus.
Multiple episodes of rehabilitation were performed both in in-patient and home settings. Despite those interventions the patient gradually deteriorated with regards to her social participation and activities of daily living. The patient experienced limitations in the ability to work, walk independently, and perform home work and self-care.
According to the instruction from the hospital the cervical collar was worn permanently. A skin abrasion at the right occipital area at the level of the collar rim occurred a couple of weeks following discharge. Neither the patient nor her family was able to consult any health professional such as a general practitioner or a community nurse due to restrictions in out-patient services associated with the COVID-19 pandemic. The sore, deemed superficial and relatively innocuous, was treated with soft dry dressings applied by the patient’s husband a few times a week. The collar use was continued.
On scheduled admission to the Rehabilitation Department the patient had a negative COVID-19 molecular test. The patient was normothermic, ambulant with a walking frame over a short distance, independently turning in bed, requiring partial assistance in eating, washing the upper body, grooming, and using the toilet. Total assistance was required when dressing the body and washing.
Physical examination revealed widespread muscular wasting, in the right occiput a dry lesion sized 2 × 3 cm filled with necrotic tissue and surrounded by crusts (Figure 1 presents the lesion after crust removal), bilateral skin atrophy in the lower leg area, severe bilateral rheumatoid deformities of the lower and upper extremities, bilateral glenohumeral, elbow, hand, hip and knee contractures, lower limb length discrepancy with the right lower limb deficit of 25 mm, and bilateral solidified flat-valgus foot deformity.
We revealed a lack of passive motion of the cervical spine. Medication on admission was methylprednisolone 4 mg daily, oral levodopa/benserazide, clomipramine, estazolam, fexofenadine, omeprazole, oxybutynin, paracetamol/tramadol, warfarin and transdermal fentanyl.
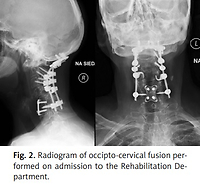
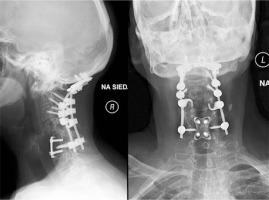
Barthel Index was 35 points indicating severe dependency [11]. The assessment with the Braden scale scored 20 points suggesting no risk of pressure sores [12]. Cervical spine radiographs performed on admission revealed proper cervico-occipital alignment (Fig. 2).
Magnetic resonance imaging was not carried out due to some concerns about safety and expected difficulty in image interpretation in the early period after administration of metal implants [13].
The rehabilitation program aimed at healing of the skin lesion, increase of extension range of the right knee, improvement of fine and gross motor skills was started. We discontinued the collar use, applied soft dressings on the decubitus area and after four days started a local laser stimulation performed every other day (K-Laser Cube-3; Eltech s.r.l., Treviso, Italy) with peak power 1 W, frequency in phases lasting for 5 s: 1st: continuous wave; 2nd: 20 Hz; 3rd: 350 Hz, exposure time: 1st procedure 15 s, 2nd procedure 30 s, 3rd procedure 40 s. The patient was advised not to rest in a supine position, to avoid compression of the occipital area. After 10 days, granulation occurred at margins of the lesion and necrotic tissue was demarked (Fig. 3).
The lesion became exudative. A microbiological test of the discharge revealed the abundance of methicillin-sensitive Staphylococcus aureus (MSSA); therefore oral clindamycin 600 mg TID was started. Seven days later dehiscence in the lower part of the previously well-healed surgical scar in the nuchal area and massive evacuation of purulent exudate spontaneously occurred (Fig. 4).
Cultures of the pus showed massive growth of Staphylococcus aureus. According to the antibiogram intravenous ceftriaxone 2 g daily was used. Despite significant regional deterioration, the functional status of the patient remained unchanged, and no fever was observed. The patient was admitted to the Neuroorthopaedic and Neurology Clinic and Polyclinic. Pharmacotherapy included administration of antibiotics (clindamycin and intravenous ceftriaxone for 14 weeks, then changed to intravenous cefuroxime 1.5 g daily for 2 weeks), enoxaparin, and oral protein supplementation. Non-pharmacological treatment consisted in serial surgical debridement (at 5th, 8th 10th and 12th week of the hospital stay), as well as negative-pressure wound therapy with the pressure of –80 mm Hg (Avelle NPWT System, ConvaTec, UK) applied to both lesions for 7 weeks after admission to the Neuroorthopaedic and Neurology Clinic and Polyclinic.
Gradual suppression of the discharge and finally closure of the fistula were achieved and a decrease of inflammatory markers was observed. The therapy of the OPS was concluded with healing of the lesion by granulation and epidermalization. The patient was discharged after overall 124 days of hospitalization and 110 days on antibiotics.
The patient’s mobility and self-care abilities did not differ significantly from the status on admission. The patient was advised to continue oral and transdermal medication as before the admission with gradual decrease a dose of methylprednisolone (8 mg daily for 2 weeks then a decrease to 4 mg) and scheduled for follow-up appointments in orthopaedic, rheumatologic and hematologic outpatient clinics.
Results
Figure 5 provides a flowchart of the process used to select the included papers. The search retrieved 1 record in Cochrane Central, 12 in EMBASE, 13 in PubMed, 14 in SCOPUS, 9 in Web of Sciences. Additionally 2 records came from manual searching. Article titles and abstracts were screened for eligibility by 2 reviewers (P.T. and V.P.K.) independently. Articles that at least one reviewer assessed as meeting the eligibility criteria were included. Full texts of eligible papers were analysed and relevant data were recorded in extraction forms. The Downs and Black quality assessment checklist [14] was applied for the appraisal of the eligible studies independently by 2 reviewers (P.T. and V.P.K.).
Fig. 5
The PRISMA flow diagram. © Reproduced with permission of the PRISMA IPD Group, which encourages sharing and reuse for non-commercial purposes.
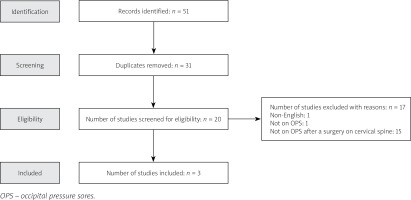
Disagreements were resolved by discussion between reviewers. Studies meeting inclusion criteria are described in Table I.
Table I
Studies meeting inclusion criteria
| Authors and year | Study design | Study purpose | Number of participants | Type of cervical spine surgery | Type and time of spinal immobilization | Number and rate of OPS cases | OPS grade/description | OPS risk factors | OPS prevention | OPS treatment | Downs and Black quality assessment checklist |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fehlings et al. (1993) [15] | Retrospective case series | To present an experience with OCF using a 5-mm malleable rod fixed to the skull by wires | 16 | OCF | Philadelphia (in 13/16 cases), Halo vest in 3/16). Immobilization time NS | 1/16 (6.2%) | Small, supeficial | NS | NS | NS | 13/27 |
| Hirano et al. (2010) [16] | Retrospective case series | To present outcomes of two methods of OTF for severe destructive cervical lesions in patients with RA | 56 | Group A: OTF with rods, sublaminar wiring, transverse process or pedicle hooks in the thoracic spine, and thoracic PS (38/56), Group B: OTF with cervical PS and platerod system (18/56) | Group A: HALO west (1–2 months) followed by SOMI or Philadelphia (2 months), Group B: HALO west (1 week), followed by SOMI (2 months), followed by Philadelphia (2 months) | 2/56 (3.6%) | NS | NS | NS | NS | 15/27 |
| Singh et al. (2021) [17] | Prospective nonrandomized single-blind study | To compare the surgical outcomes among patients withcranioceevical anomaly undergoing spinal fusion With or without ganglion C2 preservation | 171 | OCF, C1-C2 fusion | Philadelphia, immobilization time NS | 6/171 (3.5%) | NS | OCF to pars interarticularis of C2 Resection of ganglion C2 | NS | The pedicle skin graft in one patient | 18/27 |
The selection process yielded the inclusion of 2 retrospective case series and one prospective single-blind comparative study aimed at presenting outcomes in a total of 243 patients undergoing cervical spine stabilization surgery. Principal outcomes included mean blood loss during surgery, fusion quality, neurologic statement, wound healing and presence of pressure sores.
A single case of a superficial OPS due to collar use in a 45-year-old patient with severe tetraparesis due to a rheumatoid C1C2 instability treated with rigid O–C7 fixation was mentioned by Fehlings et al. [15] in a retrospective analysis of 16 patients stabilized with a malleable rod wired to the skull and vertebral structures.
Hirano et al. [16] in their retrospective study comparing two methods of occipito-thoracic fusion for RA-related cervical spine destruction reported two cases of OPS. There were no details provided about which surgical group this complication occurred in, ulcer severity, or treatment applied.
The bi-centre single-blind study of Singh et al. [17] described a group of 171 patients who underwent OCF or C1C2 fusion for craniovertebral junction anomaly. In 88 cases a surgical technique for C2-ganglion preservation was applied and in the remaining 83 cases, the C2 ganglion was sacrificed for joint manipulation aimed at achieving better fusion. Occipital pressure sore were observed in detail in a group of patients in whom fusion from the occiput to the pars interarticularis of C2 was performed (54 patients, 6 OPS – 11%), in comparison with patients stabilized between the C1 lateral mass and the pars inter-articularis of C2 (107 patients, 0 OPS) and between the occiput and the C2 pedicle (10 patients, 0 OPS). Comparison of the results between patients with preserved and resected C2 ganglion was performed in 153 cases. Within this group, there were 3 OPS observed in 75 patients with the C2 ganglion resected (4%) and no cases OPS in patients with the C2 ganglion preserved. The report does not contain information on the severity of OPS, besides an anecdotal mention that one of the patients required a pedicle skin graft for the OPS.
Discussion
According to the authors’ knowledge, this is the first description of an OPS associated with deep infection involving a spinal construct complicating OCF and the first report of a pressure sore associated with the delay in care provision related to a pandemic. Our patient could be at significant risk both of OPS and surgical site infection due to the RA itself, chronic immunosuppression, prolonged steroid use, cachexia, poor skin quality, multimorbidity and the revision spinal surgery. Elimination of neck movements due to a wide stabilization of the cervical spine could additionally raise the risk of skin damage when a stiff collar is used [2].
Probably, OPS served as an entry point of infection that subsequently spread to deeper tissues along metal rods. The abscess settled in the lowest part of the surgical site due to gravitation. One cannot, however, rule out that the OPS and deep infection started independently, but early in the course of the disease, skin lesions located at the upper and lower end of the scar became communicated. The lack of an accurate professional follow-up procedure could have been a critical factor for the development of OPS and its consequences.
Rheumatoid arthritis patients after OCF should be recognized as at risk of serious complications of collar application and other complications of spinal surgery, in particular infections, due to consequences of the use of steroid and disease-modifying antirheumatic drugs, concomitant diabetes mellitus, cardiovascular conditions and frequently advanced age at surgery [18].
The systematic review of the literature revealed a small number of studies describing OPS in persons undergoing cervical surgery. The frequency of OPS development was 3.5–6.2%. One study allowed the detection of OPS risk factors related to a surgical technique. None of the studies provided OPS risk factors associated with patient-related factors, underlying health conditions, OPS grading, or description of OPS prevention. There have been no studies evaluating the influence of a pandemic on the prophylaxis and management of OPS.
The literature does not allow one to assess the applicability of existing OPS prevention guidelines to patients after elective spinal surgery. To date, pressure ulcers resulting from collar use have mostly been described in trauma patients treated in an intensive care unit [6, 19]. The incidence of collar-related pressure ulcers in this group was 6.8% to 38% and lesions most frequently occurred at the occiput, chin, shoulders and back [20]. Risk factors for pressure ulcers due to collar use included: prolonged use of the collar, having a hard collar, longer period of unconsciousness, prolonged time to cervical spine clearance, malnutrition and anaemia [7, 19, 21].
Widely accepted preventive measures established for persons after trauma included: selection of the correct size of the cervical orthosis to fit the individual, protection of the skin with dressings in high-risk areas, daily assessment of the skin under the orthosis, avoidance of placement of the device over the area of prior or existing pressure ulceration, education of staff on the correct use of orthoses and prevention of skin breakdown, increasing awareness of oedema under orthosis and potential for skin breakdown [8–10].
Patients after elective spinal surgery may need prolonged use of a cervical orthosis, but they are usually mobile and for most of the time they stay outside the hospital. The selection of an adequately designed collar appears to be of crucial importance for the patient’s safety. Mass-produced braces such as the Philadelphia collar appear not to be an ideal choice in patients with RA due to the specific appearance of a RA patient (shortened neck, small chin, prominent and frequently asymmetric clavicles and shoulder bones, fragile skin, rheumatoid nodules), swelling, scar localization and overlapping of occipital plates with areas of peak pressures exerted by the device [5, 22].
An adequate appliance should be light and the contact surface with the neck and shoulders spread out sufficiently in order to avoid excessive pressure on the vulnerable areas, be easily removable to facilitate hygiene and wound care, enabling mouth and larynx access and arms free as possible to allow for maintenance of the patient’s general mobility and comfort [5]. Philadelphia collars are inferior to other appliances (e.g. Aspen, Miami J collars) with regards to the efficacy of neck stabilization, possibility of individual adjustment and risk of OPS [5, 23–25].
The halo vest, being more effective than other cervical orthoses and not compressing the OCF implant vicinity, should be considered in patients below the age of 65 if neck immobilization is necessary and collars are contraindicated [4, 5]. On the other hand, the Philadelphia collar can effectively eliminate a snake-like movement of the middle and lower cervical spine observable even with a properly placed halo vest [26].
Irrespectively of the type of orthosis applied, health professionals need to be aware of the risk of a pressure sore in the occipital area and should assure the patient’s safety by educating on how to use the appliance, perform daily skin inspection, apply extra padding or pressure-relieving appliances over vulnerable skin areas, and become knowledgeable about when to seek professional advice [8, 9, 19, 23].
The ongoing COVID-19 pandemic presents an important lesson to healthcare systems on how to involve professionals of different healthcare settings in remote prophylaxis, diagnosis and treatment of a wide number of health conditions [27]. Properly timed follow-ups by healthcare professionals should be scheduled for all patients at risk of pressure ulcers even during the time of restrictions resulting from the pandemic. The broad accessibility of information technologies allowing for transfer of good quality images increases effective telemedical interventions aimed at assessment of skin and the musculoskeletal system [28, 29].
The effectiveness and safety of telemedical technologies in the prophylaxis of pressure sores should be urgently examined, and included in revised preventive protocols when appropriate.
Conclusions
Patients with RA especially long-treated with GCs, using collars after OCF are at risk of OPS – a complication endangered with serious consequences requiring time-consuming and costly treatment. An individually adjusted appliance, effective skin care and adequately timed follow-up procedures should be assured to all RA patients after OCF in whom a cervical orthosis was deemed necessary.
Preventive protocols should be reviewed with respect to challenges resulting from epidemiological restrictions and accessibility of telemedical technologies.