Introduction
Rheumatoid arthritis (RA) is the most common destructive chronic inflammatory arthritis [1]. As it is a potentially serious disease [2], many studies have focused on how to achieve clinical remission. Indeed, remission in RA guarantees the patient a better quality of life.
However, achieving remission is not the only purpose of treatment in RA, because even after getting to remission, some patients are more likely to be unsatisfied with their state of health. In this purpose, the overarching principles of the 2014 treat-to-target recommendations [3] suggested that the treatment must be based on a shared decision between patient and rheumatologist. In addition, most studies agreed on the importance of involving the patient in the therapeutic decision not only to ensure better compliance [4] but also to address unmet medical needs and achieve patient satisfaction [5].
The aim of our study was to assess the satisfaction with treatment in patients with RA based on the Treatment Satisfaction Questionnaire for Medication (TSQM v1.4) and to investigate the predictive factors.
Material and methods
Study design and population
The present non-interventional, cross-sectional study was conducted in the Rheumatology Department of Mongi Slim Hospital, Tunisia, covering the period from February to October 2020.
Eligible patients were adults (aged ≥18 years) who had been diagnosed with RA, according to the 2010 ACR/EULAR classification criteria [6] and had been receiving their current approved conventional synthetic DMARD (csDMARD) or biologic DMARD (bDMARD) for at least 12 months at the time of the survey.
The disease activity had to be stable for at least 3 months, attested by a variation of Disease Activity Score in 28 joints (DAS28) less than 0.6 between 2 consultations spaced at least 3 months apart.
Patients had to understand the Arabic, be willing and able to complete patient-reported outcome (PRO) questionnaires and provide written consent to the investigator.
All consecutive patients attending a routine visit and fulfilling enrollment criteria during a period of 9 months were included.
This study was approved by the research ethics committee of our local hospital; the number of ethical approval is REC10/2020.
Data collection
Clinical parameters, including past medical history and demographic characteristics, were collected for all patients, along with details of their current treatment (molecule, duration, dose) and RA characteristics (duration of the disease, immunological profile, erosion, extra-articular manifestations, coxitis and comorbidities related to RA).
The primary outcome was patients’ RA treatment satisfaction assessed using the Treatment Satisfaction Questionnaire for Medication (TSQM; v1.4) [7]. The TSQM is a validated score including 4 subscales: effectiveness, side effects, convenience, and global satisfaction [8]. Treatment satisfaction was defined if the global satisfaction score was ≥ 80% [9].
Disease activity was assessed by DAS28 [10], functional impact assessed by the Health Assessment Questionnaire (HAQ) [11], professional impact was measured by the Rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA) [12] and the impact of RA was assessed by the Rheumatoid Arthritis Impact of Disease (RAID) score [13]. The RAID is a composite index composed of seven domains: pain, function, fatigue, physical well-being, psychological well-being, sleep disturbances, and coping. The total RAID score has a range from 0 to 10, with 10 representing the worst health and a score of ≤ 2 representing an acceptable symptom state.
Satisfaction with medical care management was assessed by three independent questions elaborated and validated by our local team. Each question was a numeric rating scale, with scores ranging from 0 (no satisfaction) to 10 (extreme satisfaction):
Are you satisfied with your medical care management in general (nursing staff, treatment…)?
Are you satisfied with your attending physician?
Are you satisfied with involvement in therapeutic decision-making?
At the end of the interview, an open question was asked to the participants to collect their propositions for improving the satisfaction with treatment.
Statistical analysis
SPSS Statistics version 25 for MacOs was used for statistical analysis.
The mean ±standard deviation (SD) (normal distribution) and median (range) (skewed distribution) were calculated for continuous variables. Student’s t-test (normal distribution) was used for analysis. Categorical variables are presented as frequency (percentage) and were analyzed using the χ2 test. Univariable linear regression analyses were performed for baseline characteristics of the patients to identify factors associated with the global satisfaction of patients. Then, the significant variables were entered into a multivariable linear regression. The linear regressions were performed using the standardized TSQM v1.4 total scores. P-values < 0.05 were considered statistically significant.
Multivariable regression analysis was applied to determine the factors associated with treatment satisfaction.
Results
Clinical parameters and demographic characteristics
A total of 70 patients were included in this study and the majority (90%) of them were female with a mean (SD) age of 57.8 years (10.6). The ages ranged from 29 to 81 years. There were 5 (7%) smoking patients. Forty-five (64%) patients had at least another past medical history apart from RA and comorbidities related to RA. The mean (SD) disease duration was 13.7 (7.2) years. Rheumatoid factor (RF) status was positive for 54% of patients, as was anti-citrullinated protein antibody (ACPA) status for 69%, with a total of 74% immunopositive patients. Rheumatoid arthritis was the erosive form in 81% of patients. A quarter of patients had comorbidities related to RA; the most common ones were osteoporosis (17%) and metabolic disorders (9%).
Seventeen percent of patients used systemic glucocorticosteroids for RA and 11% used a nonsteroidal anti-inflammatory drug (NSAID). A total of 57.1% of patients reported daily use of treatments for pain.
Methotrexate was the most frequently prescribed medication, used by 70% of patients, while only 34.2% of patients were taking bDMARDs, among them: antitumor necrosis factor monoclonal antibodies such as: etanercept (20.8%), golimumab (8.3%), adalimumab (4.1%), infliximab (4.1%); anti-IL-6 – tocilizumab (54.1%) and anti-CD20 monoclonal antibody – rituxi-mab (8.3%).
Treatment satisfaction
The mean (SD) TSQM scores were 67% (18) for effectiveness, 71% (24.5) for side effects, 65% (14.7) for convenience, and 68% (17.1) for global satisfaction. Based on a TSQM global satisfaction subscore cut-off value of ≥ 80%, only 30% of patients were considered satisfied with their current treatment.
Patient-reported outcomes
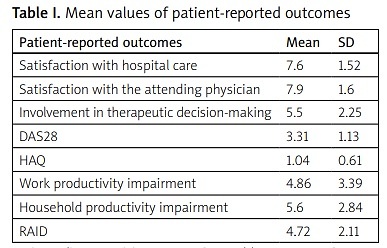
Table I summarizes mean values of patient-reported outcomes (PRO).
Table I
Mean values of patient-reported outcomes
Comparison between satisfied and unsatisfied patients
Taking into consideration global satisfaction, 30% of patients were satisfied with their treatment. We compared demographic data, characteristics of RA and PRO records of these two groups of patients. Statistically significant differences were found for coxitis, DAS28, satisfaction with the attending physician, RAID score and householding productivity impairment (Table II).
Table II
Comparison between satisfied and unsatisfied patients
Correlation between treatment satisfaction and rheumatoid arthritis characteristics
For global treatment satisfaction, a positive correlation was noted with satisfaction with hospital management (p = 0.035) and satisfaction with the attending physician (p = 0.035). Meanwhile it was inversely related to DAS28 (p = 0.004), HAQ score (p = 0.010), household productivity impairment (p = 0.001) and RAID score (p < 10–3).
Satisfaction with convenience was inversely related to treatment with bDMARDs (p = 0.013), HAQ score (p = 0.003) and RAID score items: physical difficulties (p = 0.007), emotional difficulties (p = 0.019) and coping difficulties (p = 0.005). A positive correlation was noted with satisfaction with hospital care (p < 10–3) and satisfaction with the attending physician (p < 10–3).
Satisfaction with effectiveness was inversely related to DAS28 (p = 0.012), HAQ score (p = 0.003), household productivity impairment (p < 10–3) and RAID score (p < 10–3). A positive correlation was noted with satisfaction with hospital management (p = 0.010) and satisfaction with the attending physician (p = 0.046).
Satisfaction with treatment side effects was inversely related to work productivity impairment (p = 0.004), household productivity impairment (p < 10–3), and RAID score (p = 0.011). A positive correlation was noted for treatment with methotrexate (p = 0.001) and involvement in therapeutic decision-making (p = 0.012).
Factors influencing treatment satisfaction
Factors influencing treatment satisfaction are presented in Tables III–VI.
Table III
Factors influencing patients’ global satisfaction with DMARDs, detected using multivariable linear regression analysis
| Influencing factors | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Min | Max | |||
| Satisfaction with physician | 1.70 | 1.062 | 2.980 | 0.029 |
| RAID | 0.620 | 0.450 | 0.850 | 0.003 |
| Functional disability | 0.589 | 0.432 | 0.803 | 0.001 |
Table IV
Factors influencing patients’ satisfaction with convenience with DMARDs, detected using multivariable linear regression analysis
| Influencing factors | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Min | Max | |||
| Coping | 0.728 | 0.535 | 0.991 | 0.043 |
| Treatment with biologics | 0.086 | 0.010 | 0.761 | 0.027 |
Table V
Factors influencing patients’ satisfaction with side effects with DMARDs, detected using multivariable linear regression analysis
| Influencing factors | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Min | Max | |||
| Degree of interference with domestic work | 0.692 | 0.551 | 0.870 | 0.020 |
| Degree of participation in treatment decision-making | 1.426 | 1.070 | 1.894 | 0.014 |
Table VI
Factors influencing patients’ satisfaction with efficiency with DMARDs, detected using multivariable linear regression analysis
| Influencing factors | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Min | Max | |||
| RAID | 0.83 | 0.12 | 0.94 | 0.032 |
| Coping | 0.54 | 0.33 | 0.87 | 0.013 |
In multivariable analysis, satisfaction with the physician was correlated with a better global satisfaction (OR = 1.77, 95% CI: 1.062–2.98, p = 0.029). Meanwhile, the factors that had a significant impact on global dissatisfaction were the RAID overall score (OR = 0.62, 95% CI: 0.45–0.85, p = 0.003) and one of the RAID items: the degree of physical difficulties (OR = 0.589, 95% CI: 0.432–0.803, p = 0.001).
Predictors of dissatisfaction with convenience were difficulties in adapting to RA (OR = 0.728, 95% CI: 0.535–0.991, p = 0.043) and current treatment with biologics (OR = 0.086, 95% CI: 0.010–0.761, p = 0.027).
Predictors of dissatisfaction with efficiency were the overall RAID score (OR = 0.83, 95% CI: 1.12–13.04, p = 0.032) and the difficulties of adapting to RA (OR = 0.54, 95% CI: 0.33–0.87, p = 0.013).
Finally, the predictors of satisfaction with side effects were a lower degree of interference with domestic work (OR = 0.692, 95% CI: 0.551–0.870, p = 0.02) and better involvement of the patient in the treatment decision (OR = 1.426, 95% CI: 1.07–1.894, p = 0.014).
Patients’ preferences information
When asked about their propositions on how to improve therapeutic management, patients suggested consulting a psychologist in 11% of cases, organizing an open information day in 10% of cases, teleconsulting in 10% of cases and consulting the same physician each time in 9% of cases.
Discussion
To the best of our knowledge, this is the first study to assess treatment satisfaction, among RA patients, and its predictive factors, in our country. Our study highlighted the importance of good communication between patients and physicians as well as the involvement of the patient in the treatment decision and the management of the impact of RA on the quality of life, in order to achieve better satisfaction of patients with their treatment.
Indeed, patient satisfaction is an essential pillar in the management of RA. It is closely linked to adherence to the therapeutic regimen [14] and it allows the clinician a better understanding of the patient’s needs and preferences in order to achieve clinical remission [15]. Unfortunately, satisfaction with treatment remains insufficiently documented and poorly evaluated, despite available recommendations. To assess treatment satisfaction, we used a validated tool: TSQM. Only a few studies have used validated tools [9, 16, 17]. The other studies opted for questions graduated according to the Likert scale [18, 19].
In our study, only 39% of patients reported good global satisfaction with their treatment as measured by the TSQM v1.4. Previous studies that also used TSQM to evaluate patients’ satisfaction with treatment showed that satisfaction scores were generally in the same range, going from 5.9% to 26%, as those described here [9, 16, 17, 20]. However, other studies that used local questionnaires, such as a German study, showed that the patients’ satisfaction was higher, but that some expectations remain unmet [19].
In a multivariate model, we identified the RAID overall score (OR = 0.62, 95% CI: 0.45–0.85, p = 0.003) and one of the RAID items, the degree of physical difficulties (OR = 0.589, 95% CI: 0.432–0.803, p = 0.001), as negative predictors of global treatment satisfaction. Consistent with our findings, Radawski et al. [9] reported that global treatment satisfaction was correlated with the RAID score.
In order to assess the impact of RA on the quality of daily life, the international study SENSE, a Japanese study and a Palestinian study used the 36-item short-form Health Survey (SF-36) [17, 20, 21]. The international study showed that SF-36 in its physical and mental components was a predictive factor of global treatment satisfaction – respectively (OR = 1.057 [1.036–1.078], p < 0.001) and (OR = 1.035 [1.019–1.050], p < 0.001) [17]. In the Japanese study, a high score on the mental component of the SF-36 was predictive of global satisfaction (OR = 1.27 [1.08–1.49]) [21]. A Greek study showed that fulfillment of patients’ preferences was a strong predictor of good treatment response [22].
Furthermore, we noted that satisfaction with the physician was a positive predictor of global treatment satisfaction (OR = 1.77, 95% CI: 1.062–2.98, p = 0.029). Similar results were described in the Chinese study [16]. Indeed, this study revealed that good communication with the treating physician was a predictor of global satisfaction with treatment (p < 0.01) [16].
Despite the multiple studies showing the effectiveness of bDMARDs [21, 23], we noted that these treatments were inversely correlated with satisfaction with convenience. This result can be explained by the high costs of bDMARDs [16]. Indeed, a study carried out in Japan showed that the use of biological treatment was a predictive factor of dissatisfaction (OR = 2.21, p < 0.001) [24].
Of note, the results of our study underlined the importance of psychological care, therapeutic education and shared decision-making in improving satisfaction with treatment. These results were also obtained in other studies [21, 25].
Interestingly, DAS28 was inversely correlated with all the domains of treatment satisfaction of TSQM but it was not a predictive factor of dissatisfaction. This could be explained by the fact that DAS28 represents the current level of disease activity, which is different from the severity throughout the course of the disease, unlike other subjective parameters that could better reflect the satisfaction of the patient [9].
Even though many studies have underlined the importance of collaboration between the patient and the doctor in the development of therapeutic objectives [26, 27], most of our patients did not give any propositions to improve their therapeutic management. This reluctance could be explained by the limited knowledge of patients about the disease and the treatment options. Indeed, in a study by Khalil et al. [28], 74.5% of patients were unaware of RA symptoms, complications and treatments.
Other factors could contribute to clinical inertia in patients, in particular, socioeconomic conditions, lack of communication between doctor and patient, and the complexity of treatment programs.
Study limitations
Some limitations to this study should be noted and kept in mind. First, our study was non-interventional. A randomized study would have allowed more solid conclusions.
Second, a Tunisian version of TSQM v1.4 was not assessed, so the questionnaire was translated by the physician charged with collecting data. However, to avoid disparity between patients, the same operator asked all the patients.
During the observation period adopted in the study, cases of SARS-CoV-2 infection were already recorded in Tunisia. However, this did not change the work of the rheumatology ward; the peak incidence fell in Tunisia later in 2021 [29]. Therefore, it was concluded that the pandemic had no significant impact on the assessment of the parameters included in the present study.
And finally, the generalizability of the results could be limited since the study was conducted in only one hospital. Moreover, our results do not rule out the influence of other unknown confounding factors, as satisfaction can include other aspects that were not evaluated in our study such as the cost of treatment, the economic conditions of patients and the mental health.
Conclusions
The findings from our study demonstrate that despite the diversity of therapeutic strategies, almost two-thirds of our patients remain dissatisfied with their treatment. The satisfaction with the attending physician, the participation in the treatment decision, and the impact of RA seem to be the factors that influence treatment satisfaction the most.
These data suggest that a better understanding of patients’ medical needs and preferences would improve satisfaction with treatment, and they highlight the critical need to adopt the shared decision-making approach.