Introduction
Generalized joint hypermobility (GJH) is a neglected condition among clinical practitioners [1, 2]. Though there is no universal agreement on the definition of this condition [3], it is a term that usually describes an excessive increase in range of motion (ROM) of multiple joints.
The underlying pathophysiology in joint hypermobility, though unclear, is attributed to imbalances in the proportions of type I to type III collagen tissue, hormonal factors or extracellular protein that affect the soft tissue matrix [4, 5]. With the predominant and more elastic type III collagen over type I, the tissue stiffness decreases and hence the ROM [6].
The worldwide prevalence of GJH has been variably reported depending on age, gender, and ethnicity of the studied population [6–8]. Children have the highest prevalence of GJH, which will normally decrease with increasing age [7].
The prevalence of GJH is often found to be higher among the female than the male population regardless of age [8, 9]. Ethnicity-wise, GJH prevalence is higher in persons of Asian and African descent compared to Caucasians [8], though it is not confirmed by another study [10].
The majority of the GJH prevalence studies in Asia were conducted in Middle-Eastern countries [11–14], while a few were conducted in India [15] and Korea [7].
To date, there is no known GJH study conducted among the Thai population. Giving that ethnicity can influence the prevalence of GJH, it may be worthwhile to also study the prevalence of GJH in Thailand.
Generalized joint hypermobility is frequently assessed using the Beighton scoring system and it is by far the most used system reported in the literature [7, 8, 12, 16–19]. Nine dichotomous joint hypermobility tests are included in this scoring system.
The tests are performed bilaterally on the thumb, the fifth finger, elbow and knee joint. The last test is forward flexion of the trunk with both knees extended.
Each hypermobile joint is scored one point and those with a non-hypermobile joint are scored zero, yielding a total score of nine. The original cut-off Beighton score of ≥ 4/9 indicates the presence of GJH [9].
Based on the Beighton score, all the joints assessed are in the sagittal plane. If an increase in ROM is a result of poor collagen tissue formation as stated [3], another structural characteristic or bony alignment in the frontal plane might also be altered, especially at a weight bearing joint such as the knee joint.
For example, a previous study demonstrated that the quadriceps angle (QA) tends to be greater in those healthy individuals with a higher Beighton score [20].
Though there is no clear conclusion regarding the cause of the difference, change in lower limb bony alignment may be one of the causes. For instance, it has been shown that changes of the tibiofemoral angle (TA) can influence the magnitude of the QA [21].
Additional information regarding frontal plane knee alignment may increase the understanding of GJH and its related problems.
The study was primarily conducted to determine the prevalence of GJH among Thai physical therapy (PT) students.
Secondary aims were to compare the frontal plane lower limb alignments and lower limb joint pain/injury between those with and without GJH.
Lastly, the association between lower limb joint pain/injury and the included parameters of GJH individuals was evaluated.
Material and methods
Participants
Participants were 255 PT students (208 females and 47 males) aged between 18 and 30 years of age from four physical therapy departments of the universities in Bangkok and Metropolitan areas.
After the researcher gave the information and objectives of the study, the participants who were willing to participate were screened as to whether they had ROM limitation which could limit the assessment of Beighton’s criteria. If this was the case, they would be unable to participate in the study.
All eligible participants then gave their informed consent prior to the data collection. This study was approved by the Research Ethics Review Committee for Research Involving Human Research Participants, Health Sciences Group, Chulalongkorn University (COA No. 192/2018).
Equipment and set up
The data collection was conducted in the laboratory room of each PT department. A simple questionnaire asking about general characteristics, exercise history, history of lower limb joint pain/injury, and dominant lower limb was developed to use in this study.
The participants were asked to indicate whether they had joint pain/injury within the past year. They were encouraged to recall the injuries that were caused by their normal activities of daily living or sport participations. The dominant lower limb was determined by asking “which leg would you use to kick a ball?”. The indicated leg was then determined as the dominant lower limb.
The assessment of GJH and the alignments of the lower limb were evaluated by both clinical measurements and photographic-based angle measurements. Elbow extension, knee extension, TA, and QA were measured with the photographic-based angle measurements. 12 mm colored stickers were used to indicate the anatomical landmarks for each of the joint angle or alignment measured.
A digital camera (Sony alpha-6000, Tokyo, Japan) was used for taking photos of participants. The photos were taken at the resolution of 24.3 megapixels. Then, they were downloaded onto a personal computer and analyzed with the angle tool in ImageJ software (IMAGEJ, National Institutes of Health, US) [22].
The camera setting was followed the guideline of Dunlevy and colleagues [23]. The camera was mounted on the tripod and positioned perpendicular to the joint being measured. The camera was set at two meters away from the participants. The camera focus was then adjusted to keep all the markers within the center of the picture.
For elbow extension, the camera focused on the marker at the joint while the elbow was in its maximum extended position. For knee extension, QA, and TA, the camera was set to focus on the markers at the knee joint in either the sagittal or frontal plane accordingly.
The photo of each joint angle and alignment was taken once but measured three times and the average value was used to indicate the measured angles.
Data collection
The data collection was conducted between May and November 2019. Two experienced physical therapists were responsible for assessing the GJH and localized all anatomical landmarks. The protocol for GJH assessment proposed by Juul-Kristensen et al. [24] was followed.
The opposition of thumb toward the forearm, hyperextension of the fifth finger more than 90°, and bending the trunk forward with both palms placing flat on the floor were inspected and scored at the site of data collection.
The elbow extension and knee extension angles were photographed and analyzed with the ImageJ program before the scores were given. For elbow extension, the stickers were placed on the skin over head of the humerus, lateral epicondyle of the humerus, and radial styloid process.
For knee extension, the stickers were placed on the skin over the greater trochanter of the femur, lateral epicondyle of the femur, and lateral malleolus. Individuals with a Beighton score of ≥ 4 were then classified as GJH, while those with a score of < 4 were classified as non-GJH.
The pelvic tilt angle was measured with the palpation meter (Performance Attainment Associates, St. Paul, MN). Participants stood with their feet hip-width apart and fully extended their knees.
A researcher placed one tip of the palpation meter over the anterior superior iliac spine (ASIS) and placed the other tip over the posterior superior iliac spine (PSIS). The pelvic angle was read directly from the palpation meter. The navicular drop was the height difference between the navicular head during sitting and standing positions, which was measured with a straight edge ruler.
The QA and TA were measured during relax standing (QArelax, TArelax) and while the quadriceps muscle was fully contracted and the knee joint was fully extended (QAcon, TAcon). The anatomical landmarks for QA were the ASIS, center of the patella, and tibial tubercle.
For the QArelax condition, the researcher visually checked if the participant fully relaxed the muscle prior to identification of the landmarks and sticker placement.
The sticker at the patella was then carefully placed on the center of patella. Later, this sticker was relocated after the participant fully contracted the quadriceps muscle and their knee was fully extended in the QAcon condition. This was done to localize the new position of the patella that normally moves upwards and laterally with quadriceps muscle contraction.
The landmarks for TA were the mid-way between ASIS and greater trochanter, center of knee joint, and center of the ankle joint.
Statistical analysis
The statistical analysis was conducted using SPSS (SPSS Inc., Chicago, IL) for Windows. The Kolmogorov- Smirnov test showed that data were normally distributed. To fulfil the first objective, descriptive statistics was used to describe participants’ characteristics and determine the prevalence of GJH.
Secondly, the independent sample t-test was used to compare the lower limb alignments and Fisher’s exact test was used to compare the lower limb joint pain/injury between groups.
Finally, the binary logistic regression analysis was used to fulfil the third objective of the study. Univariate analysis was first used to determine the association between lower limb joint pain/injury of the GJH group and included factors. Variables with a statistically significant (p < 0.2) association on univariate analysis were included in the multivariable binary logistic regression model.
The exercise history and QArelax were logically reasonable and were previously found to be related to lower limb joint pain/injury, and hence were also included in the multivariate models.
The odds ratios (OR) associated with particular factors were adjusted for the effect of all other factors in the model. The adjusted OR and 95% confidence intervals (CI) were calculated. Statistical significance was set at the 5% level.
Results
Prevalence of the generalized joint hypermobility
The general characteristics of the two groups were not significantly different.
The overall prevalence of GJH was 21.18% (20.00% females and 1.18% males).
The majority of the participants (92.54% in non-GJH and 94.44% in GJH) were right leg dominant. The highest frequency of hypermobile joint was found at the elbow joint for both groups. The data regarding general characteristics are listed in Table I.
Table I
Characteristics and general information of normal and generalized joint hypermobility groups
| Parameters | Normal | GJH | p-value |
|---|---|---|---|
| Number of respondents [n (%)] | 201 (78.82) | 54 (21.18) | – |
| Gender [n (%)] | |||
| Male | 44 (21.89) | 3 (5.56) | |
| Female | 157 (78.11) | 51 (94.44) | – |
| Age [years], [mean (SD)] | 21.10 (1.38) | 21.19 (1.84) | 0.707 |
| Weight [kg], [mean (SD)] | 57.46 (11.48) | 57.62 (13.26) | 0.930 |
| Height [m], [mean (SD)] | 1.63 (0.08) | 1.62 (0.06) | 0.372 |
| BMI [kg/m2], [mean (SD)] | 21.46 (3.50) | 21.80 (4.45) | 0.556 |
| Exercise [n (%)] | 121 (60.20) | 32 (59.26) | 1.000 |
| [hours/week] | 1.89 (2.37) | 1.89 (2.31) | 0.996 |
| Dominant LE | |||
| Left [(%) yes] | 15 (7.46) | 3 (5.56) | 0.772 |
| Right [(%) yes] | 186 (92.54) | 51 (94.44) | – |
| Beighton score (mean) | 1.28 (1.10) | 4.91 (1.19) | < 0.001* |
| Thumb | |||
| Right | 20 (9.95%) | 26 (48.15%) | < 0.001* |
| Left | 21 (10.45%) | 33 (61.11%) | < 0.001* |
| Fifth finger | |||
| Right | 8 (3.98%) | 19 (35.19%) | < 0.001* |
| Left | 14 (6.97%) | 23 (42.59%) | < 0.001* |
| Elbow | |||
| Right | 47 (23.38%) | 39 (72.22%) | < 0.001* |
| Left | 58 (28.86%) | 41 (75.93%) | < 0.001* |
| Knee | |||
| Right | 25 (12.44%) | 33 (31.11%) | < 0.001* |
| Left | 45 (22.39%) | 33 (31.11%) | < 0.001* |
| Trunk forward flexion | 19 (9.45%) | 18 (33.33%) | < 0.001* |
Lower limb alignments and lower limb joint pain and injury
The lower limb alignments are shown in Table II. The non-dominant QArelax was the only anatomical characteristic that showed a significant difference between GJH and non-GJH groups (24.84 ±9.41° vs. 21.11° ±8.59°, p = 0.006).
Table II
Comparison of lower limb alignment between normal and generalized joint hypermobility groups
| Anatomical measured | Side | Normal (n = 201) | GJH (n = 54) | p-value | ||
|---|---|---|---|---|---|---|
| [mean (SD)] | Min–Max | [mean (SD)] | Min–Max | |||
| Pelvic angle (°) | DMNT | 14.99 (4.51) | –5.00–25.00 | 15.81 (5.06) | 4.67–26.33 | 0.248 |
| Non-DMNT | 14.68 (4.59) | –5.00–25.33 | 15.47 (5.41) | –1.67–27.33 | 0.283 | |
| Tibiofemoral angle (°) | ||||||
| Relax standing | DMNT | 10.84 (3.12) | 2.64–19.8 | 10.92 (3.34) | 4.68–19.50 | 0.869 |
| Non-DMNT | 11.16 (3.08) | –1.53–19.36 | 11.39 (3.23) | 4.72–18.42 | 0.623 | |
| Quadriceps contracted | DMNT | 10.78 (3.03) | 2.46–18.97 | 10.81 (3.55) | 3.95–19.78 | 0.950 |
| Non-DMNT | 11.23 (3.32) | –1.25–21.01 | 11.12 (3.42) | 3.68–18.71 | 0.828 | |
| Quadriceps angle (°) | ||||||
| Relax standing | DMNT | 18.00 (8.43) | –7.56–38.55 | 19.89 (8.88) | –6.8–39.57 | 0.149 |
| Non-DMNT | 21.11 (8.59) | –0.81–45.72 | 24.84 (9.41) | 2.58–42.42 | 0.006* | |
| Quadriceps contracted | DMNT | 15.53 (6.70) | –2.43–33.10 | 15.51 (6.94) | –2.36–30.14 | 0.982 |
| Non-DMNT | 17.54 (7.93) | 0.00–53.75 | 19.41 (7.65) | 2.89–36.58 | 0.121 | |
| Navicular drop [mm] | DMNT | 9.87 (3.62) | 3.00–23.00 | 9.55 (3.70) | 2.00–18.5 | 0.558 |
| Non-DMNT | 9.67 (4.12) | 0.00–27.00 | 9.79 (3.24) | 3.00–16.00 | 0.846 | |
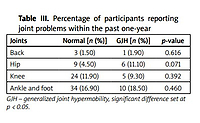
In addition, there was no significant difference in the rate of joint pain/injury during the past year between groups for any joints (Table III).
Table III
Percentage of participants reporting joint problems within the past one-year
| Joints | Normal [n (%)] | GJH [n (%)] | p-value |
|---|---|---|---|
| Back | 3 (1.50) | 1 (1.90) | 0.616 |
| Hip | 9 (4.50) | 6 (11.10) | 0.071 |
| Knee | 24 (11.90) | 5 (9.30) | 0.392 |
| Ankle and foot | 34 (16.90) | 10 (18.50) | 0.460 |
The ankle and foot areas were reported to have the highest rates of joint pain/injury for both groups. The hip ranked second while the knee ranked third for the GJH group. The non-GJH group had knee and hip as the second and third location of joint pain/injury.
Association between generalized joint hypermobility and lower limb joint pain and injury
Univariate analysis showed that the p-value of age and the navicular drop of the dominant leg were less than 0.2. Thus, these two variables were included in the multivariable binary logistic regression model along with the exercise history and QArelax. When multivariable binary logistic regression was used, only age and the navicular drop of the dominant leg were included in the final model.
However, there was no significant association between GJH and age (B = 0.315, ORadj = 1.371, 95% CI: 0.973–1.932, p = 0.071) and the navicular drop of the dominant leg (B = –0.173, ORadj = 0.841, 95% CI: 0.692–1.022, p = 0.082).
Discussion
Prevalence of the generalized joint hypermobility
The primary objective of this study was to investigate the prevalence of GJH among Thai PT students. Overall, we detected the GJH prevalence of 21.18% using the Beighton cut-off score at ≥ 4 [9].
Although various Beighton scores, including 4/9, 5/9 or 6/9, have been recommended to determine GJH in different population [9, 25], a consensus has not been established. Thus, the original cut-off score of ≥ 4 was used to determine GJH in current study.
The GJH prevalence found in this study was within the range reported in other studies [7, 8, 11, 12, 14, 15]. Studies in Asian countries reported varying number such as 7% in Pakistan [11], 20% in patients who were referred to the rheumatology clinic in India [15], 22.3% in undergraduate students in Kuwait [12], 29.76% in university students in Iraq [14], and 36.5% among Korean women [7].
Other than joint hyperextension, the poorer postural orientation has also been reported in GJH individuals. A study by Booshanam et al. [17] also reported a significantly lower Reedco Posture score for upper back, trunk, and lower back alignment in the sagittal plane in benign joint hypermobility syndrome (BJHS) individuals compared to those of non-hypermobile individuals. Changing trunk alignment may also influence pelvic and lower limb alignment.
Eventually, these potential alignment variations in conjunction with joint instability might influence the joint load distribution, which can cause unwanted mechanical force. This then increases joint stress which leads to ligament and soft tissue injuries, overuse injury, and predisposes to osteoarthritis from years of excessive joint motion [26, 27].
The above statement seems convincing since there are many studies reporting that GJH is associated with an increased risk of musculoskeletal injury in general and athletic populations [17, 19, 28].
A prospective study by Tobias et al. [19] found that adolescents who had been classified as having GJH (Beighton score ≥ 6) were at a greater risk of developing musculoskeletal pain at the shoulder, knee, and ankle/foot areas twice as much as those who did not have GJH. The knee pain could be even worse if GJH individuals were also obese.
Another study by Booshanam et al. [17] found that the knee was the first and the most painful joint reported by individuals with BJHS which was significantly higher than the non-hypermobile group. Moreover, Pacey et al. [28] reported that athletes with GJH had higher risk of knee joint injury during contact sport.
On the other hand, some studies found no significant difference in rate or type of musculoskeletal injury between individuals with and without GJH [18, 29, 30].
Moreover, some GJH individuals have been found to be asymptomatic throughout their lives [5]. These conflicts might indicate a lack of thorough understanding of GJH and whether or not GJH is really associated with the musculoskeletal problems. Addressing the prevalence and consequences of having GJH could help improve knowledge for a preventative exercise program for the upcoming problems.
Considering the prevalence of GJH among university-aged persons, Reuter and Fichthorn reported [10] 12.5%, Oddy et al. [31] reported 20%, Russek and Errico reported [18] 26.2%, and Antonio and Magalhaes [16] reported 26.8% GJH prevalence. Based on these results, it could be implied that GJH is also not uncommon in Thai PT students.
Among the joints assessed with the Beighton score, the current study found that elbow hyperextension was the most prevalent positive joint hyperextension, unlike other studies which reported that fifth finger hyperextension was the highest in prevalence [12, 16].
One reason could be that the assessments for hyper- mobility were different, for example, using a 5-point self-administered questionnaire [16], or might be due to different testing positions used which was not clearly reported nor assessed with a standardized protocol in previous studies [7, 12].
The current study followed the standardized protocol reported by Juul-Kristensen et al. [29], which could potentially put the joint and other soft tissues at their maximum stretch. Thereby, the measurements truly represented the end range of joint motion.
The results also indicated that the prevalence of hypermobile joints was often higher on the left side than that on the right side in both groups. This was consistent with previous studies showing the higher prevalence of hypermobile joints on the left side [12–14].
Additionally, Al-Rawi et al. [14] analyzed the prevalence of hypermobile joint according to handedness. They found that thumb and fifth finger hyperextension was significantly more frequent in the non-dominant hand of the right-handed participants.
Lower limb alignments
The current study showed that only the QArelax on the non-dominant side of the GJH group was found to be significantly higher than that of the non-GJH group.
This result was in line with a previous study by Sendur et al. [20], who reported significantly higher QA in individuals with a higher Beighton score, irrespective of side measured or limb dominancy. They supported the idea that GJH results from increased ligamentous laxity and hence increased magnitude of QA [20].
Considering the effect of leg dominancy, the current results were in contrast to the study by Jaiyesimi and Jegede [32], who reported that leg dominancy did not have a significant impact on the QA in healthy individuals. The higher QA on the right leg found in their study was also in contrast to the current results, as the non-dominant leg was the left leg of most participants [32].
Multiple factors have been found to influence the magnitude of the QA measurement. Mainly, the state of the quadriceps muscle contraction [33] and anatomical characteristics [21, 34, 35] can influence the magnitude of the QA. As all lower limb alignments were measured in a standing position, the participants were encouraged to stand with their weight equally distributed between legs.
Furthermore, the state of the quadriceps contraction was visually inspected before photos were taken to reduce the difference in level of muscle contraction which could alter the magnitude of the angle measured, especially the QA [33].
By following these procedures, the difference magnitude of the QArelax found in this study could surely represent the true difference between groups. This difference could have resulted from change in the soft tissue property of the GJH individuals, which will be further discussed.
The difference of the magnitude of QArelax between groups disappeared in the QAcon condition. This result indicated that the GJH did not impact the frontal plane bony alignment, i.e., TA, but might, by some means, impact the musculotendinous unit (MTU) component controlling the frontal plane patellar alignment on the non-dominant leg.
Previous studies reported similar levels of muscle stiffness [36] and muscle activation [37] of vastus medialis and vastus lateralis muscles during active muscle contraction between GJH individuals and non-GJH individuals.
However, the difference found only in the QArelax condition in the current study might indicate that the QA- related parameters differ at low level muscle contraction (resting muscle tone) or in the musculotendinous stiffness.
This raised the question whether GJH could also influence the MTU property and neuromuscular control during the resting or inactive state. Further studies regarding these topics would be beneficial to clarify the physiology or function of the MTU in the GJH population.
The anatomical characteristics that have been reported to influence or have an association with the magnitude of the QA included TA, femoral anteversion, hip rotation, tibial torsion, and navicular height [21, 34, 35]. Among these, TA and navicular height were reported to have a substantial impact on the magnitude of QA [34, 35].
The current results did not find a difference in magnitude of TA in both quadriceps contraction states, so it was implied that the TA did not influence the magnitude of the QA in the current study.
Since the navicular height was not recorded, its influence on the QA could not be discussed. Even though Nguyen et al. [35] reported that the bony alignment in the frontal plane has a more forceful impact on the magnitude of QA, the influence of femoral anteversion and hip rotation could not be neglected since asymmetrical rotational alignment had been observed in many participants.
In addition, it could be postulated that there was another factor that was not measured in the current study but could affect QA.
Lower limb joint pain and injury
The current results did not find the prevalence of joint pain/injury within the past year of the GJH group to be significantly greater than those of the non-GJH group at any joints.
Moreover, the results showed that the age, exercise history, and lower limb alignments measured in this study were not associated with lower limb joint pain/ injury in GJH individuals. This was in line with some previous studies which reported that there was no difference in prevalence of injury and no correlation or association between type of injury and GJH [10, 18, 38].
Other studies regarding joint pain or injury in GJH among the college-aged population obtained similar results that GJH did not increase the risk of musculoskeletal pain/injury [10, 12 ,18, 31].
Among these studies, two were conducted among students in anatomy and physiology [10] and health science faculties [12] which most resembled the current study’s participants, physical therapy students.
With the knowledge regarding their expertise such as human anatomy and physiology, these participants could be more aware of their physical status. Thus, they might be more likely to understand and be more careful in order to prevent joint pain/injury.
Physical activity or participation in sport can be another factor contributing to the occurrence of pain/injury as found in other studies [16, 18, 38]. Participants who actively and always participated in sport could be at higher risk of getting joint pain/injury [38]. However, the current study did not find this to be the case.
One reason might be the comparable time spent in exercise of the two groups. Both groups spent nearly two hours (1.89 hours) per week, which is under the time recommended by the World Health Organization (WHO) for this age group [39].
Therefore, there was low incidence of lower limb joint pain/injury, as found in the current study, which may explain why there was no difference between the groups. Another possible explanation is that it was because the exercise reported in the current study was recreational activity.
Thus, the results did not support the idea that GJH increased the risk of musculoskeletal pain/injury in low intensity type of exercise. Consequently, further research is required to investigate the relationship of GJH and musculoskeletal pain/injury in more strenuous exercises.
There is a paucity of research on lower limb alignment in GJH as a risk factor for increasing lower limb joint pain/injury. QArelax, TA, and navicular drop were measured in this study to investigate the impact of GJH on frontal plane lower limb alignments and whether or not these factors in conjunction with the presence of GJH would be associated with lower limb joint pain/injury. The results did not confirm this.
Even though greater QA was found to be related to knee pain and knee injury [40], the participants of both groups reported similar rates of knee problems. Moreover, the current results revealed no association among those alignments and lower limb joint pain/injury in the GJH individuals.
Though the current findings indicated that GJH did not increase the rate of or was associated with lower limb joint pain/injury, the clinician or physical therapist should not omit this condition altogether.
This is due to the paucity and conflicting information regarding GJH. Additionally, participants in the current study may not be representative of all GJH individuals.
Moreover, there is evidence that joint hypermobility can become problematic [24, 26], and that physical therapy could be more beneficial in managing the musculoskeletal pain/injury for hypermobile people than using medication [6].
It would be beneficial to screen for GJH and QA in the clinical setting and the physical therapist should raise awareness that musculoskeletal problems can be a result of hypermobility as well as those of the limited ROM. By doing so, a suitable intervention can assuredly be prescribed.
Conclusions
The current study reported the prevalence of GJH in Thai PT students as 21.18%. The most common hypermobile joint was found to be the elbow joint. Generalized joint hypermobility individuals showed higher QArelax of their non-dominant leg than the non-GJH ones but the difference disappeared once measured during quadriceps muscle contraction.
Nonetheless, the results showed that the GJH individuals did not have an increased rate of lower limb joint pain/injury.
Moreover, none of the outcome measures – age, exercise history, and lower limb joint alignment – was associated with lower limb joint pain/injury in college-age GJH individuals.