Introduction
Rheumatoid arthritis (RA) is a chronic synovial inflammatory disease, characterized by symmetric and destructive polyarthritis. Extra-articular manifestations of RA are also well known, including disorders of the cardiovascular, respiratory, nervous, and urinary systems, eyes and skin. Regarding the skin, rheumatoid nodules are the most frequent cutaneous abnormalities [1].
Patients with RA may also manifest a wide spectrum of other skin conditions, and dermatological involvement tends to occur in patients with more severe or active RA. However, in some patients, RA-related dermatoses may occur although the joint symptoms are well controlled.
Here, we present a case of rheumatoid neutrophilic dermatitis (RND), a rare neutrophilic skin condition, in a patient with RA being treated with methotrexate.
Case report
A 65-year-old man with a 10-year history of rheumatoid arthritis (RA) was admitted to the Department of Dermatology due to numerous nodules and papules located on the right lower leg that were resistant to the treatment with topical steroids and topical and systemic antibiotics.
According to the medical history, the first lesions appeared after a minor injury resulting from a bike accident two months earlier. The patient was treated for RA with methotrexate in a dose of 25 mg/week and 2 mg/day of methylprednisolone. At the first admission to the hospital, RA symptoms were well controlled with the above-mentioned treatment. In addition, the patient suffered from arterial hypertension and hypercholesterolemia for which he received 2.5 mg/day of bisoprolol with 1.5 mg/day of indapamide and 20 mg/day of atorvastatin, respectively.
On admission, grouped bluish-purple nodules and papules were present on the flexor area of the right shin (Fig. 1). The patient did not report any subjective complaints such as itching or burning sensations within the skin lesions. The laboratory examination confirmed the presence of rheumatoid factor in the serum as well as eosinophilia (8.6%, normal range 2–4%) and elevated levels of C-reactive protein (CRP) (3.5 mg/dl, normal range < 1 mg/dl), lactate dehydrogenase (LDH) (330 U/l, normal range 120–246 U/l) and β2-microglobulin (5.03 mg/l, normal range 0.81–2.19 mg/l).
Sonography revealed reactively enlarged axillary and inguinal lymph nodes with a maximum dimension of 20 mm. X-ray examination of the right lower leg demonstrated an osteochondral outgrowth in the medial part of the tibia which was also visualized with a computed tomography (CT) scan (Fig. 2).
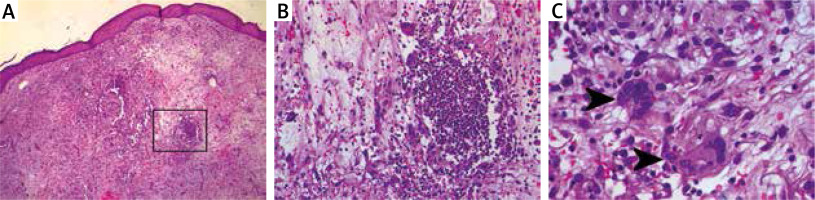
Bacteriological and fungal examinations of the smear from the lesions as well as a biopsied skin sample were negative. Histological assessment of the skin biopsy revealed edema of the papillary and reticular dermis, proliferation of small vessels, and a dense neutrophilic infiltrate with histiocytes, a few multinucleated giant cells and neutrophils forming microabscesses locally (Fig. 3).
Fig. 3
A dense neutrophilic infiltrate with histiocytes, multinucleated giant cells and neutrophils locally forming microabscesses (hematoxylin and eosin, original magnification × 4) (A). Enlarged area marked on previous image – microabscess with leukocytoclasis within the vessel wall (hematoxylin and eosin, original magnification × 20) (B). Multinucleated giant cells within the inflammatory infiltrate (arrowheads) (hematoxylin and eosin, original magnification × 40) (C).
The patient was started on methylprednisolone pulse therapy (3 × 500 mg i.v. given every month) combined with dapsone 100 mg/day and topical betamethasone ointment. The other drugs were taken at the same doses as before. One month later dapsone was stopped due to megaloblastic anemia, mild thrombocytopenia and hyperbilirubinemia and the dose of methotrexate was reduced to 15 mg/week. After another month the abnormal laboratory parameters normalized; however, the patient complained about the significant deterioration of joint symptoms related to RA, so the dose of methotrexate was increased gradually to 25 mg/week, which resulted in decrease of RA activity. In the meantime, methylprednisolone pulse therapy resulted in significant improvement of existing skin lesions (Fig. 4). The patient continues the treatment with reduced doses of steroids, being under regular follow-up.
Fig. 4
The lesions from Fig. 1 after 7 intravenous pulses of methylprednisolone – mostly postinflammatory hyperpigmentation with only a few active lesions is seen.

Discussion
Skin problems in patients with RA may be divided into RA-specific conditions, RA-related dermatoses and skin problems due to the treatment taken by a patient.
Rheumatoid arthritis-specific skin lesions are seen only in RA patients and include rheumatoid nodules, rheumatoid nodulosis, accelerated rheumatoid nodulosis, rheumatoid vasculitis and RND.
Rheumatoid arthritis-related skin diseases include dermatoses that are linked with RA but may also occur in connection with other conditions. This group of skin diseases includes Sweet’s syndrome, pyoderma gangrenosum, neutrophilic palisading granulomatous vasculitis, Raynaud’s phenomenon, livedo racemosa interstitial granulomatous dermatitis with arthritis (IGDA), and erythema elevatum diutinum (EED) [2].
Rheumatoid neutrophilic dermatitis is a rare entity, first described in 1978 by Ackerman, which belongs to the group of neutrophilic dermatitis [3]. The disease affects women more often, with a 1:2 male to female ratio [4]. It is a specific skin manifestation of RA with a prevalence of 0.9–1.8% among all RA patients [5, 6]. The pathogenesis in unknown, but it is suggested to be an immune-complex-mediated disease [1].
Rheumatoid neutrophilic dermatitis occurs more commonly in patients who have severe, long-lasting seropositive arthritis and clinically manifests as asymptomatic erythematous papules, nodules, plaques or urticaria-like lesions [5–7]. Vesicles, blisters, ulcers and annular lesions are less frequent [4, 8]. Skin lesions are usually symmetric, but sometimes, like in our case, may be distributed asymmetrically [8–10]. Extensor surfaces of extremities and joints are favored locations with a predilection to the dorsal surfaces of hands and arms [11–13]. In that sense our patient is quite unique, as eruptions were located on the lower leg, involving predominantly the flexural aspect of the shin.
The differential diagnosis of RND in our patient included sporotrichosis, cutaneous lymphoma and reaction to a foreign body (because of injury reported by the patient) [10, 11, 13]. The final diagnosis was made based on the microscopic examination showing typical histologic features of RND: primarily dense dermal infiltration consisting predominantly of neutrophils, papillary dermal microabscesses, and leukocytoclasis without vasculitis [9, 14]. Spongiosis, intraepidermal and subepidermal vesiculation, subepidermal edema and basophilic degeneration of the dermal collagen may also be seen on some occasions [9, 15, 16].
Conclusions
Rheumatoid neutrophilic dermatitis may be treated with topical or systemic corticosteroids or dapsone (50–100 mg/day) [7, 17, 18]. Antimalarials, such as hydroxychloroquine, have also been shown to be effective [19]. Sometimes, cyclophosphamide was the only drug that provided improvement [20]. On the other hand, some lesions disappear spontaneously. Skin lesions heal without scarring, though sometimes leaving skin discolorations, as in our patient [10].




