Dear Editor,
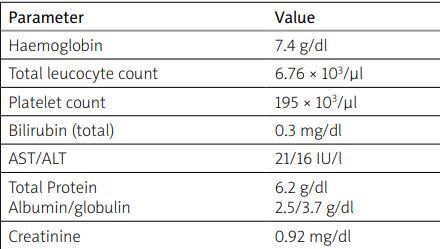
We present the case of a 26-year-old female patient, who came to us with complaints of generalized swelling in the legs and a malar rash on her face, during the 17th week of gestation. The patient’s complaints had begun only 1 month before prior to which she was fine. On general examination mild pallor and pedal edema were observed. The initial vital state was stable. Investigation showed mild anemia with a hemoglobin level of 7.4 mg/dl. Initial investigations are presented in Table I. Serum albumin levels were low (2.5 g/dl) and urine examination showed presence of proteinuria. 24-hour urine protein estimation was 8 g/day. Other significant results: ANA positivity (1 : 2560, homogenous) and raised anti-dsDNA levels (450 IU/ml) as well as positive direct Coombs test. The ENA was positive for anti-Sm, anti-SSA and anti-SSB antibodies and C3 (31 mg/dl) and C4 levels (8 mg/dl) were also low, suggestive of lupus flare. Echocardiography showed mild pericardial effusion.
Table I
Initial investigations of the patient
The patient was diagnosed with lupus nephritis with autoimmune hemolytic anemia and serositis. Ultrasound abdomen assessment done at baseline showed a normal healthy fetus appropriate for gestational age. The patient was counselled regarding the implication of lupus and its treatment for the mother and her baby’s health. Patient decided to continue with the pregnancy. Kidney biopsy could not be done due to her pregnancy. Absence of granular casts and RBC casts in urine hinted towards a possible class V lupus nephritis, so she was started on a high dose of glucocorticosteroids (1 mg/kg) along with tacrolimus, hydroxychloroquine and low-dose of acetylsalicylic acid (aspirin).
During the described treatment the disease stabilized and went into partial remission, but proteinuria (1.5 g per day) persisted. In other laboratory tests C3 and C4 levels were normal and anti-dsDNA levels had come down. Routine ultrasound abdomen done at the 21st week revealed severe oligohydramnios (amniotic fluid index, AFI: 3–4) with normal fetus. Uterine artery Doppler was normal. Screening for antiphospholipid syndrome was negative as well as for infections such as cytomegalovirus, rubella, syphilis, toxoplasmosis, hepatitis B, hepatitis C and HIV. There was no history of substance abuse and screening for hypertension and gestational diabetes was also normal. Oligohydramnios was seen as a lupus associated complication.
After a literature review, it was decided to start treatment with tadalafil (phosphodiesterase-5 – PDE5 inhibitor) 20 mg daily. The patient was followed up with weekly ultrasounds, thereafter. Repeat abdominal ultrasound after a week showed mild improvement in AFI. By week 26, amniotic fluid had returned to normal (AFI: 9–10) with a fetus appropriate for gestational age. The patient went into preterm labor at 29 weeks of pregnancy. Abdominal ultrasound showed a fetus with asymmetric intra uterine growth retardation (IUGR) and small for gestational age. Normal vaginal delivery was performed: new born baby girl weight 1.2 kg was born. Apgar score at 1 min was 8 and at 5 mins was 9. The newborn after staying in a neonatal intensive care unit for 2 weeks, due to low birth weight, did well.
The patient, after giving informed consent and giving up breastfeeding was started on monthly cyclophosphamide infusions. This drug was chosen due to financial reasons. Glucocorticosteroids were gradually tapered. Patient finally went into remission with 24-hour urine protein in the range of 350 mg/day. After completion of 6 monthly doses of cyclophosphamide (total dose 4.5 gms) azathioprine was introduced as a maintenance therapy. Presently, the described patient continues to be in follow-up and is doing well.
Discussion
Oligohydramnios occurs in < 1% of preterm pregnancies and 5% of term pregnancies [1]. Incidence is increased to about 12% in patients with systemic lupus erythematosus (SLE) [2]. Oligohydramnios in the second trimester mostly occurs secondary to preeclampsia, diabetes, intrauterine infections, foetal anomalies, maternal drug abuse, SLE or antiphospholipid syndrome. However, some cases remain idiopathic [3].
Management of oligohydramnios in pregnancy mostly relies on treating the underlying cause. The approach to treatment in patients with idiopathic oligohydramnios remains undefined. Several case reports have described improved AFI and other foetal parameters with sildenafil and tadalafil in non-lupus pregnant patients with IUGR and oligohydramnios [4, 5]. Phosphodiesterase type 5 inhibitors have been reported to increase uteroplacental perfusion and improved uterine artery Doppler parameters [6].
However, large population based studies are lacking, partly due to the lack of data on the safety of these drugs in pregnancy. Our patient had a dramatic response to tadalafil and AFI improved to normal within a few weeks.