Introduction
The COVID-19 pandemic in the years 2020–2023 (in the Republic of Poland, the state of epidemic was declared on 20 March 2020, was changed to the state of epidemic emergency on 12th of May 2022, and was revoked on 1 July 2023) has brought numerous challenges for healthcare. One such significant problem is prolonged persistence of symptoms in various organs after an infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing COVID-19 disease [1]. For this reason, disease syndromes with symptoms after the acute phase of the disease have been distinguished. There are various definitions of post-COVID syndromes, depending on the duration of symptoms; however, it is usually accepted that symptoms lasting more than 3 weeks are described as post-COVID syndrome, whereas those lasting over 3 to 6 months are described as long COVID (chronic COVID) syndrome [2–4]. In publications cited in this article as well as in many others a huge variety of symptoms has been identified in the post-COVID syndrome, encompassing practically every functioning area of the human body. This, however, poses a problem in scientific work and in clinical practice related to the lack of specificity of symptoms in the post-COVID syndrome. An important question, both for the research and the clinical treatment, is determining the intensity of symptoms to distinguish those which occur significantly more often with post-COVID syndrome than with the general population and pose a more challenging therapeutic issue. It is particularly relevant in the process of treatment, which relies predominantly on rehabilitation – identification of symptoms which pose a real problem will make it possible to focus on those areas of a patient’s functioning which actually deteriorate the quality of life. Attention is also paid to the fact that the course of the post-COVID syndrome is important in the symptomatology of rheumatic diseases and points to the role of rheumatology while attending to patients with post-COVID syndrome, which results from the nature of the symptoms [5].
In Polish conditions, rehabilitation units for post-COVID-19 patients were established, in which the “Post-COVID syndrome symptoms assessment card” (PCSAC) [6] was introduced to evaluate the effectiveness of rehabilitation. However, based on the collected data, the frequency of symptoms appearance in post-COVID syndrome and their intensity may be determined, which allows for the identification of primary therapeutic targets, but also enables the verification of hypotheses relating to the pathomechanism of post-COVID syndrome based on the actual presence of the symptoms.
The aim of this study was to determine the severity of symptoms with patients starting rehabilitation treatment after suffering from COVID-19 up to and including December 2021, on the basis of the PCSAC to compare results with the non-COVID patients referred for rehabilitation for other reasons, mainly musculoskeletal diseases resulting in chronic pain. The cut-off date of December 2021 for including patients in the study resulted from a change in the phenotype of the SARS-CoV-2 virus from the previously predominant Alpha and Delta variants to the Omicron variant, which proved more infectious but causing a milder course in comparison to the previous variants of SARS-CoV-2, which may have changed the picture of post-COVID-19 syndromes [7].
Material and methods
The study group consisted with 59 patients recruited from patients referred for treatment to the rehabilitation ward (sanatorium) after experiencing COVID-19 with a diagnosed post-COVID syndrome (post-COVID, long COVID) and started their rehabilitation up to 6 to 12 months after the treatment of the acute phase of the disease.
The regulations for admittance to the ward were specified in the regulations of the National Health Fund (NFZ) in Poland [6, 8]:
The first condition – diagnosis of COVID-19 infection confirmed with a positive PCR test for SARS-CoV-2, or hospital discharge papers with a confirmed diagnosis of COVID-19. The regulation assumed the end of home isolation, which is defined in other regulations, hospital discharge or the isolation ward discharge date, as the end of treatment for COVID-19. Rehabilitation in these units could begin up to 6 months after treatment for COVID-19 had been completed. In October 2021, this period was prolonged to up to one year after the completion of treatment.
The second condition – the presence of post-COVID syndrome symptoms as measured by a different questionnaire, including “dyspnoea, fatigue, muscle weakness, pain, memory impairment, depressive states or anxiety”. To qualify for admission to the ward patients needed to answer positively to the aforementioned symptoms.
The results were compared with questionnaires from patients referred for sanatorium treatment who formed the control group. Fifty-seven questionnaires had been filled in; patients with a history of SARS-CoV infection were excluded from this group. Patients with no history of undergoing COVID-19 had been referred to the sanatorium unit mainly with a diagnosis of musculoskeletal dysfunction; approx. 90% involved major diagnoses with ICD-10 (International Statistical Classification of Diseases and Related Health Problems 10th Revision) codes: M47 – spondylosis of the spine, M51 – other intervertebral disc disorders, G54 – nerve root disorders, M15 – poly-osteoarthritis, M16 – hip osteoarthritis. There were single diagnoses of J31 – chronic rhinitis, nasopharyngitis and pharyngitis, J44 – chronic obstructive pulmonary disease, E66 – obesity, I10 – hypertension. In conclusion, non-COVID patients were a group with predominant musculoskeletal symptoms.
The assessed groups were homogeneous in terms of age; however, in terms of sex there was a predominance of women in the post-COVID group in contrast to the control group with male predominance. Nevertheless, in the control group sex showed no differentiating level of the severity of ailments apart from 2 symptoms: dizziness (p = 0.022) and sleep disorders (p = 0.012). Comparison of groups in terms of age and sex is presented in Table I.
Table I
Comparison of groups in terms of age
Questionnaire
The PCSAC consists of 31 questions relating to symptoms appearing in a post-COVID syndrome. The symptoms specified in the questionnaire have been described in numerous detailed publications and in review papers and form a typical set of symptoms for the post-COVID and long COVID syndromes [4, 5, 9–11]. The answer to the question is a rating given by the patient on whether a symptom exists and how intense it is on a scale from 0 – no symptoms, to 10 – maximum intensity of symptoms. Symptoms were divided into 11 groups that correspond to particular areas of functioning of the body. Table II shows the questions and statistical analysis of the answers provided by the post-COVID group and the control group. It needs to be highlighted that there was a question in the questionnaire formulated “Olfactory disorders – other”, which nobody answered, and therefore it was not included in the comparison.
Table II
Symptoms intensity in post-COVID and non-COVID patients
| Health problems/group | N | Average | SD | Mean | Min | Max | Q1 | Q3 | p |
|---|---|---|---|---|---|---|---|---|---|
| Medium intensity of health problems | |||||||||
| Post-COVID-19 | 59 | 2.63 | 0.95 | 2.61 | 0.74 | 4.94 | 2.06 | 3.35 | < 0.001* |
| Non-COVID-19 | 57 | 0.90 | 0.54 | 0.84 | 0.00 | 2.52 | 0.48 | 1.16 | |
| Chronic fatigue | |||||||||
| Post-COVID-19 | 59 | 5.97 | 1.55 | 6.00 | 3.00 | 10.00 | 5.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.53 | 1.21 | 0.00 | 0.00 | 4.00 | 0.00 | 0.00 | |
| Feeling unwell after physical effort | |||||||||
| Post-COVID-19 | 59 | 6.25 | 1.66 | 7.00 | 2.00 | 9.00 | 5.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.63 | 1.47 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Fever | |||||||||
| Post-COVID-19 | 59 | 0.24 | 0.93 | 0.00 | 0.00 | 5.00 | 0.00 | 0.00 | 0.19 |
| Non-COVID-19 | 57 | 0.07 | 0.53 | 0.00 | 0.00 | 4.00 | 0.00 | 0.00 | |
| Joint pain | |||||||||
| Post-COVID-19 | 59 | 4.86 | 2.75 | 5.00 | 0.00 | 10.00 | 3.00 | 7.00 | 0.369 |
| Non-COVID-19 | 57 | 4.61 | 2.25 | 5.00 | 0.00 | 10.00 | 3.00 | 6.00 | |
| Muscle pain | |||||||||
| Post-COVID-19 | 59 | 4.92 | 2.37 | 5.00 | 0.00 | 10.00 | 3.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 2.11 | 2.70 | 0.00 | 0.00 | 9.00 | 0.00 | 5.00 | |
| Resting dyspnoea | |||||||||
| Post-COVID-19 | 59 | 0.12 | 0.65 | 0.00 | 0.00 | 4.00 | 0.00 | 0.00 | 0.166 |
| Non-COVID-19 | 57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Dyspnoea on exertion | |||||||||
| Post-COVID-19 | 59 | 5.83 | 1.93 | 6.00 | 0.00 | 8.00 | 5.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.96 | 1.96 | 0.00 | 0.00 | 8.00 | 0.00 | 0.00 | |
| Cough | |||||||||
| Post-COVID-19 | 59 | 2.39 | 2.43 | 2.00 | 0.00 | 8.00 | 0.00 | 4.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.86 | 1.80 | 0.00 | 0.00 | 9.00 | 0.00 | 1.00 | |
| Secretion retention | |||||||||
| Post-COVID-19 | 59 | 1.69 | 2.08 | 0.00 | 0.00 | 7.00 | 0.00 | 3.00 | 0.003* |
| Non-COVID-19 | 57 | 0.72 | 1.54 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Tightness in the chest | |||||||||
| Post-COVID-19 | 59 | 1.83 | 2.01 | 2.00 | 0.00 | 6.00 | 0.00 | 3.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.56 | 1.18 | 0.00 | 0.00 | 5.00 | 0.00 | 0.00 | |
| Chest pain | |||||||||
| Post-COVID-19 | 59 | 1.71 | 1.99 | 1.00 | 0.00 | 6.00 | 0.00 | 3.00 | 0.004* |
| Non-COVID-19 | 57 | 0.72 | 1.39 | 0.00 | 0.00 | 6.00 | 0.00 | 1.00 | |
| Palpitations | |||||||||
| Post-COVID-19 | 59 | 3.17 | 2.65 | 4.00 | 0.00 | 8.00 | 0.00 | 5.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.88 | 1.62 | 0.00 | 0.00 | 6.00 | 0.00 | 1.00 | |
| Rapid heartbeat | |||||||||
| Post-COVID-19 | 59 | 3.15 | 2.62 | 4.00 | 0.00 | 8.00 | 0.00 | 5.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.75 | 1.47 | 0.00 | 0.00 | 6.00 | 0.00 | 1.00 | |
| Abdominal pain | |||||||||
| Post-COVID-19 | 59 | 0.85 | 1.99 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | 0.09 |
| Non-COVID-19 | 57 | 0.28 | 1.11 | 0.00 | 0.00 | 6.00 | 0.00 | 0.00 | |
| Nausea | |||||||||
| Post-COVID-19 | 59 | 0.47 | 1.49 | 0.00 | 0.00 | 6.00 | 0.00 | 0.00 | 0.014* |
| Non-COVID-19 | 57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Diarrhoea | |||||||||
| Post-COVID-19 | 59 | 0.51 | 1.60 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | 0.32 |
| Non-COVID-19 | 57 | 0.23 | 1.07 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Decreased appetite | |||||||||
| Post-COVID-19 | 59 | 0.75 | 1.69 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | 0.001* |
| Non-COVID-19 | 57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Concentration disorders | |||||||||
| Post-COVID-19 | 59 | 4.93 | 2.50 | 5.00 | 0.00 | 9.00 | 3.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.82 | 1.67 | 0.00 | 0.00 | 8.00 | 0.00 | 1.00 | |
| Memory disorders | |||||||||
| Post-COVID-19 | 59 | 4.81 | 2.50 | 5.00 | 0.00 | 9.00 | 3.00 | 7.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.86 | 1.63 | 0.00 | 0.00 | 8.00 | 0.00 | 2.00 | |
| Headache | |||||||||
| Post-COVID-19 | 59 | 2.25 | 2.61 | 2.00 | 0.00 | 9.00 | 0.00 | 4.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.79 | 1.71 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Dizziness | |||||||||
| Post-COVID-19 | 59 | 2.61 | 2.55 | 2.00 | 0.00 | 8.00 | 0.00 | 4.50 | < 0.001* |
| Non-COVID-19 | 57 | 0.47 | 1.30 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Sleep disorders | |||||||||
| Post-COVID-19 | 59 | 4.05 | 3.08 | 5.00 | 0.00 | 9.00 | 0.00 | 7.00 | 0.001* |
| Non-COVID-19 | 57 | 2.18 | 2.38 | 2.00 | 0.00 | 8.00 | 0.00 | 4.00 | |
| Tingling | |||||||||
| Post-COVID-19 | 59 | 3.68 | 3.05 | 4.00 | 0.00 | 9.00 | 0.00 | 6.00 | 0.124 |
| Non-COVID-19 | 57 | 2.84 | 2.37 | 3.00 | 0.00 | 8.00 | 0.00 | 4.00 | |
| Numbness in the limbs | |||||||||
| Post-COVID-19 | 59 | 3.73 | 2.96 | 4.00 | 0.00 | 9.00 | 0.00 | 6.00 | 0.088 |
| Non-COVID-19 | 57 | 2.79 | 2.40 | 3.00 | 0.00 | 8.00 | 0.00 | 4.00 | |
| Depression | |||||||||
| Post-COVID-19 | 59 | 2.93 | 2.57 | 3.00 | 0.00 | 8.00 | 0.00 | 5.00 | < 0.001* |
| Non-COVID-19 | 57 | 0.70 | 1.31 | 0.00 | 0.00 | 5.00 | 0.00 | 1.00 | |
| Anxiety | |||||||||
| Post-COVID-19 | 59 | 2.76 | 2.60 | 3.00 | 0.00 | 8.00 | 0.00 | 4.50 | < 0.001* |
| Non-COVID-19 | 57 | 0.70 | 1.44 | 0.00 | 0.00 | 5.00 | 0.00 | 0.00 | |
| Ringing in the ears | |||||||||
| Post-COVID-19 | 59 | 2.08 | 2.68 | 0.00 | 0.00 | 8.00 | 0.00 | 5.00 | 0.001* |
| Non-COVID-19 | 57 | 0.74 | 1.79 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Tinnitus | |||||||||
| Post-COVID-19 | 59 | 2.17 | 2.65 | 0.00 | 0.00 | 8.00 | 0.00 | 5.00 | 0.003* |
| Non-COVID-19 | 57 | 0.95 | 1.99 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | |
| Loss or impairment of taste | |||||||||
| Post-COVID-19 | 59 | 0.42 | 1.35 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | 0.014* |
| Non-COVID-19 | 57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Loss or impairment of smell | |||||||||
| Post-COVID-19 | 59 | 0.36 | 1.27 | 0.00 | 0.00 | 7.00 | 0.00 | 0.00 | 0.026* |
| Non-COVID-19 | 57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
Statistical analysis
Comparison of the values of quantitative variables was performed in 2 groups using the Mann-Whitney test, and the comparison of the qualitative variables was performed using the χ2 test. The calculations were performed using R software, version 4.2.2. (R Core Team [2022]. R: A language and environment for statistical computing. R: Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Data availability
The materials (completed questionnaires) are available from the authors of the study.
Bioethical standards
The questionnaire was part of the routine management of post-COVID patients. In the case of the control group, the questionnaire was part of a physical examination and an interview regarding the symptoms reported by the patient. The questionnaire was given to the patient (regardless of the group) by the doctor ordering the rehabilitation treatment. Each patient gave informed consent to the use of the questionnaire for research purposes, provided that the data were anonymized.
Results
The complete results are shown in Table II. The following parameters are significantly higher in post-COVID-19 patients than in non-COVID-19 patients: chronic fatigue, feeling unwell after physical effort, muscle pain, dyspnoea on exertion, cough, secretion retention, tightness in the chest, chest pain, palpitations, rapid heartbeat, nausea, decreased appetite, concentration disorders, memory disorders, headache, dizziness, sleep disorders, depression, anxiety, ringing in the ears, tinnitus, loss or impairment of taste, loss or impairment of smell, and the overall parameter of average severity of health problems calculated on the basis of the answers given, not appearing as a separate question in the questionnaire. “Olfactory disorders – other” from the last question of the questionnaire was a parameter that was not taken into consideration due to the fact that all interviewees indicated no such symptoms.
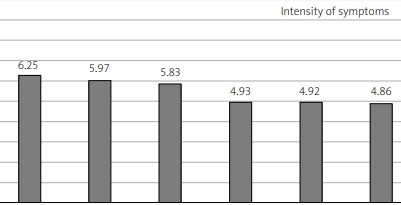
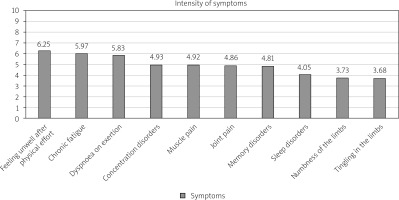
Of the symptoms listed in the questionnaire, those of the highest intensity in post-COVID patients, in order, including the statistical average, are shawn in Figure 1.
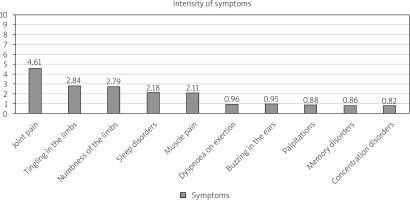
The highest intensity of symptoms in non-COVID patients (including the statistical average) is presented in Figure 2.
Discussion
The main goal of this study was identification of characteristic post-COVID symptoms among adult patients beginning their rehabilitation treatment. Symptoms of the highest severity were identified and presented in Figure 1. Owing to this, out of the multitude of symptoms related to post-COVID syndrome, the ones which pose a significant therapeutic problem can be distinguished.
The comparison of the COVID group with the non-COVID group allowed for the identification of symptoms which have no significant importance for both groups. These are: diarrhoea and abdominal pains and resting dyspnoea as well as olfactory disorders. Another symptom whose intensity does not statistically significantly differ between these two groups is fever perceived as a typical symptom of post-COVID syndrome. In the classic sense, this symptom refers to body temperature higher than or equal to 37.6°C [12]. Observation of post-COVID syndrome documented a fever > 100.4 F, i.e. 38°C, which occurred in approx. 30% of patients, but also an increased temperature to approximately 38°C, which occurred in almost 60% of patients, as well as temperature instability, low temperature, a feeling of coldness, and other temperature-related problems. Post-COVID syndrome, thus, included not only fever but also various issues related to body temperature regulation. With that said, the important observation is that the risk of fever, defined as a body temperature of 38°C or more, significantly decreases within 28 days of the onset of COVID symptoms [12, 13]. The problem, therefore, is the lack of a clear criterion in the questionnaire. The symptom was reported by a total of 5 patients and its maximum intensity was 5 on the scale used in the questionnaire. This observation may indicate that fever-related symptoms do not constitute a significant problem in post-COVID syndrome.
An important element in the discussion of the results is the lack of significant difference found in the case of joint pain. In both groups, those of post-COVID-19 and non-COVID patients, the problem of joint pain was strongly expressed. The average response was 4.86 points for post-COVID and 4.61 points for non-COVID patients. Joint pain is, therefore, a significant problem in both groups. The non-COVID group was recruited from among sanatorium patients with predominant diagnoses of osteoarthritis (OA). The questionnaire did not include a question that would differentiate between peripheral joint pain and spinal pain, and thus it was assumed that spinal pain would be assigned to the question concerning joint pain. Spinal pain, or low back pain, is one of the most common causes of acute and chronic pain, and occurs in more than 70% of people over the age of 30 [14]. Due to the nature of the control group, i.e. sanatorium patients who in approximately 90% of cases were referred for treatment with a primary diagnosis of OA including spine OA and other lesions causing musculoskeletal pain, it is, therefore, impossible to determine statistically significant differences in the incidence of joint/spinal pain symptoms between the control and post-COVID group.
The same proved true in the case of the symptoms of tingling in and numbness of the limbs. Once again, the study did not show significant differences in the occurrence of these symptoms between the groups. In the post-COVID group, the average score for tingling in the limbs was 3.68 points and for numbness 3.73 points, whereas in non-COVID patients the average score for tingling was 2.84 points and for numbness 2.79 points. Tingling in and numbness of the limbs are among the typical symptoms of neuropathic pain, the spread of which in a group of patients with chronic pain can reach up to 25% [15].
The method utilised here which consisted in a comparison of the study group with the control group made it possible to identify the symptoms with the highest intensity among adult sanatorium patients, as shown in Figure 2. Due to the characteristics of the control group, which was described before, one could expect dominant symptoms from the musculoskeletal system [16]. An important observation from the practical point of view is the intensity of symptoms typical for neuropathic pain, i.e. tingling and numbness of limbs, which has practical significance – diagnostic and therapeutic.
It was also found that patients with post-COVID and long COVID syndrome characterize their health as considerably worse compared to the non-COVID group referred to sanatorium treatment despite referred complaints in this group.
Study limitations
The main limitation may be that the control group consisted of patients referred to the sanatorium or for rehabilitation due to different musculoskeletal diseases, mainly OA with chronic pain and low back pain, including neuropathic pain. Therefore some symptoms were more pronounced than in the general population and were comparably often as in patients after COVID-19.
The weakness of the study may also be its strength, i.e. it indicates that some of the symptoms are not so characteristic of post-COVID syndrome if we take into account ailments resulting from civilization diseases such as OA, which are increasingly observed in different age groups (not only older ones) and the effects of overload and degenerative changes in the skeleton, especially the axial part.
It should be highlighted that the aim of the present study was not to assess the results of rehabilitation, but it was limited to identifying the actual symptoms that constitute a problem in post-COVID syndrome, which allowed the rigor of the research to be maintained.
Conclusions
The study has shown that among 31 symptoms identified as post-COVID-19 syndrome symptoms that were included in the PCSAC, 23 differed significantly from the control group in terms of symptoms intensity.
Three of the eight remaining symptoms, namely joint pain, tingling in the limbs, and numbness of the limbs, occur in high intensity; however, in the control group with a predominant diagnosis of OA they were also were present. Five symptoms, i.e. fever, abdominal pain, diarrhoea, resting dyspnoea, and olfactory disorders (categorized as “other”), did not show a significant difference between the groups. In addition, this study identified symptoms with the highest intensity in post-COVID-19 patients. It also listed the main issues in non-COVID sanatorium patients treated predominantly due to musculoskeletal dysfunction.