Introduction
Spondyloarthritis (SpA) is an umbrella term used to describe several types of inflammatory arthritis, predominantly affecting the axial skeleton and/or the peripheral joints of the arms and legs. Spondylarthritis includes psoriatic arthritis (PsA), ankylosing spondylitis (AS), peripheral SpA, SpA associated with inflammatory bowel disease (IBD), axial SpA (axSpA), and many more [1].
Axial SpA affects mainly the axial skeleton and/or to a lesser degree the peripheral joints and the periarticular tissues (i.e., the entheses) and may be accompanied by various extra-articular symptoms including uveitis, psoriasis and inflammatory bowel diseases (IBD). In this distinct arthritis entity, the human leukocyte antigen (HLA) B27 (HLA-B27) gene is almost universally expressed among patients and consists of a diagnostic criterion [2].
According to the 2009/2011 Assessment of Spondylo-Arthritis (ASAS) International Society classification criteria [3], axSpA is divided into subclasses depending on the presence of sacroiliitis in imaging studies (X-ray or magnetic resonance imaging – MRI): radiographic type (formerly called AS, characterized by features of sacro-iliitis) and a non-radiographic form.
Typically, it presents insidiously as low-back, or alternate-buttock pain before the age of 45 years, lasting for more than half an hour, in a persistent manner exceeding 3 months in duration [4].
Symptoms may improve with exercise and non-steroidal anti-inflammatory drugs (NSAIDs), but not with rest, while inflammatory markers can be elevated [5].
The temporomandibular joint (TMJ) unites the temporal bone cavity with the mandibular condyle, holding a key role in the majority of oral functions, including mastication, speech, and jaw motion [6, 7]. It consists of an articular cartilage and a fibrous capsule, a disk, a synovial cavity (membrane and fluid), and several tough adjacent ligaments [7].
When affected in axSpA, it can lead to severely disabling situations varying from facial pain to ankylosis, trismus, limited mouth opening, poor oral hygiene with devastating impact on individuals’ quality of life [8].
Temporomandibular disorders (TMD) encompass entities affecting TMJ’s anatomy and function and the associated signs and symptoms like pain of TMJ, headache, joint mobility, systemic and congenital diseases affecting TMJ and masticatory muscle disorders [8].
The diagnostic criteria for TMD (DC/TMD) comprise a set of criteria enabling prompt evaluation, homogeneity, and consistency in the assessment of TMJ complaints and symptoms, based on biopsychosocial parameters [8].
Complaints and symptoms are subdivided in 3 groups, namely:
group I – muscle disorders,
group II – disc displacements,
group III – arthralgia/arthritis/arthrosis.
It is estimated that TMDs affect more than 30% of the general population [9], with the female/male ratio being calculated at 2 [10].
Pathophysiology
In SpA, the intraarticular inflammation increases compression and shear forces that these joints need to endure [11, 12]. As a result, inappropriate reactive ossification follows, leading to limited range of movement, rendering the joints more susceptible to damage [11].
Bone marrow oedema close to the joint surfaces and subchondral oedema, destruction of the fibrocartilage along with synovitis are some of the intraarticular phenomena due to axSpA [13]. The temporomandibular joint is a ginglymoid diarthrosis with a fibrocartilaginous cartilage covered by synovium [14].
In terms of the interplay between axSpA and TMD, craniocervical postural changes and synovial inflammation appear to hold key roles. Postural changes secondary to cervical vertebrae malalignment, affect muscles and tendons surrounding TMJ. As a result, the mechanical load and pressure are increased, leading to an altered jaw position [15].
Postural changes as a contributing factor for TMD have been proposed by several investigators [16–18]. However, there are also studies arguing that the observed craniocervical alignment and unilateral disc displacement are not related to TMD [19, 20]. Although bilateral ankylosis of TMJ is not common in axSpA, in the literature there are several published cases of patients with AS and PsA and symmetric TMJ ankylosis [21–25].
Shadamarshan Rengasayee et al. [14] proposed the abnormal condylar loading as a putative mechanism elucidating simultaneous co-occurrence of TMJ and AS. It seems that the altered jaw position can initiate a self-perpetuating inflammatory milieu in genetically predisposed individuals, aggravating ossification, thus limiting the range of motion (ROM).
In addition, the articular disc itself represents a functional tendon enthesis of lateral pterygoid muscle as an embryonic remnant and can also be affected by axSpA.
Ankylosing spondylitis
Ankylosing spondylitis is the most common type of axSpA, corresponding to the radiographic type based on the latest ASAS classification [3]. The global incidence of AS varies worldwide ranging from 0.7 to 49 per 10,000 (0.007–0.49%) [26].
The mean prevalence of AS per 10,000 population ranges between 7.4–31.9, with Africa and North America exhibiting the lowest and greatest prevalence, respectively [5]. Male sex preponderance is also apparent, with the Rochester Epidemiology Project [27] suggesting an 4 times higher risk among men compared to women of the same age, and a recent meta-analysis showing that 70.4% of the pooled patient population are men [28].
In parallel, a hereditary aspect is also evident, with first degree relatives of patients with AS having a 20 times greater risk of developing an akin diagnosis [29]. As for the exact prevalence of TMD in AS, this is not yet known, however, among all rheumatic and musculoskeletal diseases (RMDs), AS has been reported to have the greatest TMD burden [30–33]. In Table I details of primary studies of patients with AS and TMD involvement are presented [30, 31, 33–49].
Table I
Primary studies of patients with ankylosing spondylitis and temporomandibular disorders involvement
| First author | Sample | Study design | Recruitment | TMD Diagnostic criteria | Results | |
|---|---|---|---|---|---|---|
| Site | Duration | |||||
| Aceves-Avila et al. [31] | n = 33 patients with AS and n = 92 patients with RA, n = 25 with SLE and n = 21 with OA | CS | Rheumatology Clinic of a Teaching Hospital in Guadalajara, México | 2010–2011 | Question-naire | A total of 39% of patients with AS exhibited TMDs, being the most frequent RMD with TMJ involvement alongside OA |
| Bilgin et al. [34] | n = 98 patients with AS | CS | Departments of Physical Medicine and Rehabilitation and Rheumatology, Hacettepe University, Ankara, Turkey | 2018–2019 | DC/TMD | TMDs were diagnosed in 59.2% of the sample. Craniocervical posture measurements and spinal mobility and were similar among groups. Smoking, bruxism (women), AS disease activity and neck disability (men) were greater in patients with TMD. Active smoking, bruxism in females, high ASDAS–CRP in males and neck disability were independent risk factors for TMD in AS. No relationships were noted between the craniocervical posture measurements and TMD |
| Canger et al. [35] | n = 63 patients with AS with no signs or symptoms of TMJ-related disease and n = 65 healthy controls | CS case-control | Department of Oral and Maxillofacial Radiology, Erinyes University, Faculty of Dentistry, Turkey | NR | Helkimo [77] | FD values were lower in patients with AS than controls (ROI1 and ROI2), but no differences were noted between groups for FD in ROI3, AEI, or KI. No differences were observed in any parameter regarding AS disease duration |
| Crum et Loiselle [36] | n = 26 patients with AS | CS | Veterans Administration Hospital, Hines, Illinois, USA | NR | NR | Four out of 26 patients had severe TMJ complaints. These were treated with acrylic interocclusal splints and the symptoms were alleviated in 3/4. It is likely that the symptoms are produced by the postural effects of the AS and not the disease itself |
| Davidson et al. [37] | n = 79 patients with AS | CS | Departments of Rheumatology, St. Bartholomew’s Hospital and the Westminster Hospital, London, UK | NR | NR | Patients with TMD were older and had mild symptoms, with the predominant clinical feature was restricted mouth opening, presenting important difficulties during emergency anesthesia |
| De-la-Llave-Rincon AI et al. [38] | n = 20 subjects with AS and n = 20 matched healthy controls | CS case-control | Department of Physical Therapy, Occupational Therapy, Physical Medicine and Rehabilitation, Universidad Rey Juan Carlos, Alcorcón, Madrid, Spain | 2004 | TrPs | Patients with AS had a greater number of TrPs than controls, including reduced mouth opening and cervical mobility. Within the AS arm, a positive association was noted between the number of active TrPs and occiput-to-wall distance, as well as between mouth opening and cervical mobility. A negative relationship was noted between mouth opening and occiput-to-wall distance, and between mouth opening and the total number of TrPs |
| Helenius et al. [39] | n = 18 patients with AS, n = 18 patients with SpA and n = 16 patients with RA, n = 15 patients with MCTD | CS case-control | Outpatient Department of Rheumatology of Helsinki University Central Hospital, Sweden | 1996–1997 | NR | MRIs revealed reduced articular cartilage in 25% of RA, 0% of MCTD, 17% of AS and 17% of SpA patients. Identified condylar changes included osteophytes, erosion or abnormal shape, whereas disc alterations included abnormal anterior position, perforation and reduced movement. These abnormalities were more frequent in RA and least frequent in those with MCTD and SpA diagnoses. Crepitation and reduced mouth opening were related to disc and articular cartilage abnormalities. In panoramic tomograms, severe condylar erosion was associated with MRI findings of condylar erosion, abnormal condylar shape, diminished condylar cartilage thickness and abnormal temporal surface shape. Limited mandibular movement, crepitation and pain during jaw movement indicated structural TMJ damage |
| Helenius et al. [32] | n = 19 patients with AS, n = 21 with SpA and n = 24 patients with RA, n = 16 with MCTD and 80 matched healthy controls | CS case-control | Outpatient Department of Rheumatology of Helsinki University Central Hospital, Sweden | 1996–1998 | NR | Patients with RMDs reported severer TMJ symptoms than control subjects. Those with AS reported more frequent symptoms (37%). Mean maximal mouth opening was reduced in RMDs (46.3 ±8.6 mm) than in control subjects (55.0 ±7.4 mm). Marked erosions were observed in 17% of patients with RA, 19% of MCTD, 38% of SpA, 17% of AS patients and 1 control subject. Erosion was associated with condyle restricted movement and a correlation was observed between radiographic findings relating to the TMJ and clinical and subjective stomatognathic symptoms in RMDs |
| Huang et al. [40] | n = 3204 patients with AS and n = 12,816 age- and sex-matched controls | Retrospective cohort with control arm | Longitudinal Health Insurance Database, Taiwan | 2000–2010 | NR | The incidence of TMD in the AS cohort was 2.88-fold greater when compared with other patient groups (1.54 vs. 0.53 per 10,000 person-years). Adjustment for sex, age and comorbidity, revealed a 2.66-fold (95% CI: = 1.79–3.97) higher risk of TMD occurrence in the AS cohort. AS appears to impact the occurrence of TMD in a significant manner |
| Iordache et al. [33] | n = 55 patients with AS and n = 152 patients with RA and n = 33 healthy controls with signs-symptoms related to TMJ involvement | CS case-control | Grigore T. Popa University of Medicine and Pharmacy, Iași, Romania | 2005–2007 | NR | TMJ involvement is frequently reported in patients with RA and AS and account for high levels of disability and impaired health-related quality of life |
| Yıldızer Keriş et al. [41] | n = 79 patients with RMDs (39 with RA, 17 with AS, 23 with pSS), n = 79 age- and sex-matched healthy controls | CS case-control | Rheumatology Outpatient Clinic of the Department of Internal Medicine, Faculty of Medicine, Gazi University, Turkey | NR | NR | More subjective symptoms were noted in patients with RMDs (73.4%) compared to controls. The most common objective symptoms included pain at lateral TMJ palpation (29.1% patients vs. 8.9% controls) and mandibular movement (19% patients vs. 2.5% controls), and palpation muscle pain (38% patients vs. 3.8% controls) |
| Locher et al. [42] | n = 50 patients with AS | CS | Maxillofacial Surgery and Rheumatology Departments, University Hospital, Zurich, Switzerland | 1989–1991 | NR | A tendency to a reduced mouth opening was observed in older age. Mouth opening capacity was unrelated to AS duration. In 1/5 of the sample, circumscribed or diffuse erosions were observed, with the condyle being involved in 6 patients, the fossa in 1 patient and both structures in 3 patients. Assessment of the arthritic alterations using a 3-point scale showed that 2 patients had severe, two had moderate and 6 had mild radiographic arthritic signs |
| Major et al. [43] | n = 43 patients with AS and n = 16 controls | CS case-control | Department of Oral Health Sciences, University of Alberta, Edmonton, Alberta, Canada | NR | NR | TMD headache symptoms (duration and frequency), painful jaw movement and TMJ pain (duration and frequency) were more frequent in AS. Differences were observed in MRI indices for disc displacement and degenerative changes. Disc displacement was noted in 62% joints in the AS arm compared to 34% joints in the controls. Degenerative change was noted in 20% joints in the AS group compared to 6% joints in the controls |
| Ramos-Remus et al. [44] | n = 65 patients with AS and n = 22 controls | CS case-control | Two secondary care outpatient Rheumatology Clinics, Guadalajara, Mexico | 1993 | NR | Patients with AS exhibited greater variability in TMJ mobility than controls and showed increased frequency of condylar erosions, sclerosis, flattening and temporal flattening. Condylar erosions were associated with longer AS duration, neck complaints, and atlantoaxial subluxation |
| Resnick [45] | n = 25 patients with AS | CS | Department of Radiology Veterans Administration Hospital, San Diego, California, USA | NR | NR | A total of 32% of the sample exhibited TMDs. The most common radiographic features include joint space narrowing, followed by erosions, reduced mobility, osteophytosis and beaking, extensive sclerosis, demineralization, and widening of the joint space |
| Shim et al. [30] | n = 15 patients with axSpA and n = 18 with peripheral SpA and n = 19 healthy controls, n = 21 patients with RA and n = 56 patients with OA | CS | University Ansan Hospital, Korea | 2016–2018 | NR | Patients with axSpA, peripheral SpA, and RA showed higher scintigraphic uptake at the TMJ compared with those in the control and OA arms. Compared with patients without axial involvement, those with axial involvement also exhibited greater TMJ scintigraphic uptake with elevated symptomatic rates in TMD |
| Souza et al. [46] | n = 30 patients with AS | CS | Rheumatology Department, Oswaldo Cruz University Hospital (HUOC), Recife-PE, Brazil | 2017–2018 | DC/TMD | Most patients (80%) were HLA-B27 positive, with elevated disease activity (mean BASDAI 7.70 ±2.30) and functional disability (mean BASFI 7.00 ±2.63, HAQ-S 1.79 ±0.62). More than half (57%) of the patients shared the 3 TMD groups, and 30% shared two TMD groups (I and III). Over 73% of the patients scored high in the chronic pain scale (Grade III–IV), associated with high depression |
| Tegelberg and Kopp [47] | n = 19 individuals with AS and n = 16 patients with RA | Case-control (3-yr follow-up, following a 3-wk stomatognathic physical training program) | Department of Stomatognathic Physiology, Central County Hospital, Västerås, Sweden | NR | Helkimo [77] | The clinical dysfunction score was lower in RA, and the mouth opening capacity was larger than before training. Among patients with AS, no long-term changes in the CDS were noted, except for an increase in mouth opening capacity. In RA, a higher disease activity was noted at the follow-up period (3 years), as assessed by the ESR. The results suggest that local physical training of the stomatognathic system may induce a positive effect in individuals with RA |
| Wenneberg et al. [48] | n = 100 patients with AS and n = 57 controls without joint symptoms or disease | CS case-control | Department of Stomatognathic Physiology, University of Gothenburg, Sweden | NR | Helkimo [77] | A correlation was noted between radiographic findings in the TMJ and subjective and clinical symptoms from the stomatognathic system in AS. Thus, strong indications appear to exist that the subjective symptoms, the clinical signs, and radiographic findings in the TMJ of the patients with AS were the result of this joint disease |
[i] ADD – anterior disc displacement, AEI – articular eminence inclination, ASDAS–CRP – Ankylosing Spondylitis Disease Activity Score-C-reactive protein, BASDAI – Bath Ankylosing Spondylitis Disease Activity Index, BASFI – Bath Ankylosing Spondylitis Functional Index, CDS – Clinical Dysfunction Score, CI – confidence intervals, CS – cross-sectional, DC/TMD – Diagnostic Criteria for Temporomandibular Disorders, ESR – erythrocyte sedimentation rate, FD – fractal dimension, HAQ-S – Health Assessment Questionnaire – Spondylitis, HLA-B27 – human leukocyte antigen B27, KI – Klemetti index, MCTD – mixed connective tissue disease, MRI – magnetic resonance imaging, NR – not reported, OA – osteoarthritis, pSS – primary Sjögren’s syndrome, RA – rheumatoid arthritis, RMDs – rheumatic and musculoskeletal diseases, SLE – systemic lupus erythematosus, TMD – temporomandibular disorders, TMJ – temporomandibular joint, TrPs – trigger points.
Based largely on the radiographic findings of small patient cohorts, the prevalence of TMD in AS is ranging between 30–37% [41, 44]. Temporomandibular disorders are frequent comorbidities in AS [34], in particular among older patients and those with more extensive spinal and peripheral joint disease [36].
They also multiply AS-associated disability levels, impairing the health-related quality of life of patients with AS [33]. Most patients with AS share all three TMD groups, and approximately one third of the patients share two TMD groups [46]. Chronic TMJ pain is also a distinct characteristic for the majority of patients with AS, associated with high depression rates [46].
Restricted mouth opening is the most commonly reported clinical feature of TMDs in AS [37, 38]. According to Helenius et al. [39], reduced mouth opening, and crepitation are both related to disc and articular cartilage abnormalities. The most common radiographic features involve joint space narrowing, erosions, reduced mobility, demineralization, osteophytosis and beaking, extensive sclerosis, and widening of the joint space [45].
Condylar erosions have also been related to longer AS duration, neck complaints, and atlantoaxial subluxation [50]. Disc displacement is also very common [39, 43]. According to Bilgin et al. [34], in men, AS disease activity is closely related to the incidence of TMD, although no other study has verified this association. Independent predisposing factors for TMD in AS include active smoking, bruxism in females, elevated disease activity in males, and neck disability [34].
The interplay between the two entities was investigated in a retrospective cohort study by Huang et al. [40], aiming to understand which condition propels the development of the next one. The investigators assessed two hypotheses, namely what is the prevalence of TMD in AS and what is the prevalence of AS in TMD.
The results showed that in AS, patients had a 2.66-fold greater risk for developing TMD, and in particular, younger patient groups (under 30 years of age and between 30 and 44 years old) exhibited 4.37 and 3.02-fold higher risk for TMD.
On the other hand, TMD alone was not identified as a risk factor for developing AS. Nonetheless, AS was a more frequent diagnosis among patients with TMD patients and comorbidities including parapsoriasis, rheumatoid arthritis (RA), osteoporosis (OA), climacteric arthritis, or Cushing’s syndrome (3.66-fold greater risk), implying a possible synergistic effect [40].
Psoriatic arthritis
Psoriatic arthritis is another form of seronegative inflammatory arthritis, sharing common features with axSpA. No difference is noted in the incidence between sex, with 6 cases per 100,000 people on a yearly basis, and a prevalence of approximately 0.1–0.2% [49, 50].
Psoriatic arthritis usually accompanies plaque psoriasis (PsO), with the estimated prevalence of PsA among psoriatic cases ranging between 14–31% [51, 52]. A recent systematic review [53] pooled all primary studies of patients with PsA and TMJ involvement, including 10 case reports, 13 case series and a total of 4 case-control studies. A total of 151 cases of PsA and concomitant TMD were identified, with great discrepancy in the diagnostic criteria applied both for PsA and the assessment of TMD [53].
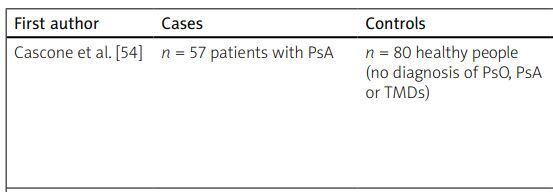
Table II describes the existing case-control studies of patients with PsA and TDM [54–59]. Compared to healthy controls, the radiological findings of TMJ positive patients with a PsA diagnosis reveal impressive bone erosion and remodeling of the mandibular condyle [54].
Table II
Case-control studies of patients with psoriatic arthritis and temporomandibular disorders involvement
| First author | Cases | Controls | Results |
|---|---|---|---|
| Cascone et al. [54] | n = 57 patients with PsA | n = 80 healthy people (no diagnosis of PsO, PsA or TMDs) | The number of TMJ positive patients paired with the radiological results revealed impressive bone erosion and remodeling of the mandibular condyle among those with PsA. The systemic treatment for TMDs should be considered not only to limit the local progress of the pathology, but also for halting PsA’s typical progression |
| Crincoli et al. [55] | n = 25 patients with PsA | n = 87 patients with PsO and n = 112 subjects without PsO/PsA | Patients with PsO, and to an even greater extent those with PsA, were more frequently affected by TMD symptoms and signs, including an internal TMJ opening derangement than healthy subjects. An increase in TMD symptoms, opening derangement, bruxism and sounds of TMJ was observed in those with PsA as compared with patients with PsO and controls |
| Dervis and Dervis [56] | n = 20 patients with PsA n = 68 patients with PsO | n = 100 healthy participants | No difference was observed between TMD signs among patients with PsO and healthy subjects. However, those with PsA did report more frequent TMD signs compared with those with PsO only and healthy controls. In PsA, muscle tenderness on palpation, TMJ sounds and stiffness/tiredness in jaws in the morning were the most frequent findings. The signs and symptoms of TMD in PsA are mainly caused by related joint involvement directly affecting the masticatory system |
| Eriksen [57] | n = 79 consecutive patients with clinical TMD or diagnosed inflammatory arthritis | n = 26 healthy volunteers | Those with clinical TMD complaints had more ADD, disc deformation, surface destructions, osteophytes, caput flattening, and edema diagnosed by MRI, compared to the controls. Among patients with arthritis, ADD, osteophytes, effusion, caput flattening and edema, as well as surface destructions were more prevalent compared to the controls. In the control arm, both the presence of osteophytes and disc deformation increased with age, and a relationship was observed for ADD and surface destructions on the condylar head |
| Giancristoforo [58] | n = 33 patients with PsA | n = 61 patients with PsO and n = 80 healthy people (no diagnosis of PsO, PsA or TMDs) | Among those with PsO, 65.4% showed signs and symptoms of TMJ involvement, without signs/symptoms of PsA in the joints. All patients with a PsA diagnosis demonstrated some TMJ involvement |
| Könönen [59] | n = 61 with PsA | n = 61 patients with RA, n = 61 with AS and n = 61 healthy controls | Greater frequencies of most subjective and clinical variables were noted in all three disease groups compared to the healthy controls. Patients with RA and PsA showed more frequent and severer TMD signs and symptoms compared to those with AS |
On the other hand, it has been reported that when panoramic radiography and transpharyngeal radiographs are used, bone disruption is not apparent in PsA [57].
Compared to patients with PsO without joint involvement, those with PsA, are more frequently affected by symptoms and signs of TMD, including an internal TMJ opening derangement [55]. The prevalence of TMD in PsO has been reported to vary between 64% [55] and 65.4% [58], whereas in PsA, the respective prevalence ranges between 80% [55] and 100% [58].
On the other hand, 24.1% of healthy controls exhibit TMD [60]. In parallel, distinct TMD symptoms are apparent, with pain (headache, neck pain, brachialgia) being more common in the PsO only patients, while tinnitus, vertigo, disc displacement with reduction and without reduction and crepitus being more prevalent in PsA.
Limited ROM is often observed in PsA, but not among patients with PsO psoriasis only, without arthritis involvement [58]. Tenderness, stiffness in the neck and shoulders, muscle pain on chewing and sensation of immobilized jaw are among the most documented complaints [55]. Psoriatic arthritis cases with TMD tend to be younger, have oligoarthritis (1–2 joints 70%), with a more recent PsO diagnosis and more advanced skin disease compared to PsO only cases [57].
When imaging techniques are applied (MRI and orthopantomography), disc displacement is observed in more than half (57%) of the PsA cases [58], 25% also report jaw morning stiffness/tiredness [57], tenderness in muscle palpation, crepitation and joint dysfunction, all in a greater proportion compared to healthy people and patients with PsO.
The most common findings in TMJ in terms of imaging in patients with PsA include disc alterations, condyle destruction (erosions, osteophytes) and effusion [60]. However, this finding does not appear to differ among patients with PsA compared to other cases of TMD [61].
Generally, TMJ pathologic sounds – including clicking and crepitus – are reported in 62.7% of the PsA cases, compared to 28% of patients with PsO and a mere 20% among healthy controls [55]. On the other hand, when patients with PsO are compared to healthy participants, differences in the TMD pathology become less apparent [57].
Clinical assessment of the temporomandibular joint
Clinical history
Questions should be directed towards symptoms related to TMD, such as pain in the region and its characteristics, as well as factors that worsen or mitigate the symptoms, restricted mandibular movements, sounds during the movement of the mandible (clicking or crepitus), episodes where the patient is unable to close their mouth (locking, which is usually associated with dislocation of the mandible) and trismus [62, 63].
In cases of trismus in particular, symptoms that include opening that is less than 15 mm, progressively worsening trismus, absence of history of clicking, pain of non-myofascial origin (such as neuralgia etc.), lymphadenopathy or a suspicious intra-oral soft tissue lesion, require an urgent referral to a specialist [63, 64].
Physical examination
The physical examination includes three domains, namely, inspection, palpation and auscultation [62, 65, 66], detailed in Table III.
Table III
Physical examination in temporomandibular disorders
Imaging
In the assessment of TMJ, imaging techniques that can be used are plain radiographs panoramic radiography, computed tomography (CT), cone-beam computed tomography (CBCT), MRI and ultrasonography (US).
Panoramic radiography can only be applied for assessing the mandibular condyle. According to Wenneberg [67], destruction of the mandibular condyles is observed in 25% of patients with AS compared to 11% of the controls. Condylar flattening, osteophyte formation, and periarticular calcification were more common in the AS cases [48].
Corrected lateral linear tomograms revealed intraarticular alterations with (20.4%) and without (48.9%) erosive changes in patients with AS [42]. In hypocycloidal tomography limitation in mobility, articular both erosive and sclerotic changes and flattening were more common in AS [50]. At this point, it is important to underline that cervical spine lateral imaging is usually requested by clinicians and it can be useful in the assessment of vertebrae alignment.
Magnetic resonance imaging application was evaluated in two studies using patients with AS [68]. In the first study, disc displacement (62%) and degeneration of articular surfaces (20%) were more common in AS compared to healthy controls (34% and 6%, respectively) [43]. In the second [39], disc subluxation was detected in 11% of AS cases, joint space narrowing in 94%, osteophytes in 67%, disc perforation in 44%, erosion or cyst of the condyle in 28% and cartilage destruction in 17%.
The same imaging modalities have also been applied in PsA. Disc displacement and thinning, condylar destruction (erosions, osteophytes, sclerosis) and joint effusions are the most common pathological findings [53, 60, 61]. It is important to mention that rheumatic involvement of TMJ can have similar findings with non-rheumatic TMD. Disc pathology though, seems to be more obvious is inflammatory arthritis [53].
Ultrasonography proves to be a quite efficient modality in the assessment of TMJ since its results are comparable to MRI (88% concordance, sensitivity 72.2% and specificity 60% comparing to MRI) [61]. Although it is believed to be particularly useful in the detection of joint effusion (synovitis), it is not the best option for the assessment of condyle morphology [60].
Panoramic radiographs can offer limited information but can be of use for screening patients [69]. Cone-beam computed tomography has a lower cost and radiation exposure compared to the CT, while it is more appropriate in the detection of bony abnormalities [70]. Soft tissue pathology including pathology of the muscles, tendons or disc can be better assessed using MRI [69, 70].
Finally, there is recent evidence that bone scintigraphy can provide evidence of inflammatory process in TMJ. As individuals with axial SpA presented a significantly higher TMJ uptake ratio on bone scintigraphy than the control group [30].
Treatment – surgery
The initial treatment of a TMD, regardless of its underlying cause is usually conservative, including a combination of factors such as jaw rest, soft diet, topical NSAIDs or DMARDs. Adjunct measures such as targeted physiotherapy and, more importantly, a soft bite splint, that can be constructed by the patient’s dentist can also be of help [22, 64].
For the treatment of TMJ in PsA, topical and systemic medication has been reported in most studies, although some also highlight the need for surgical procedures when TMJ ankylosis is apparent [53]. Patients with a PsA diagnosis, it has been suggested that a systemic TMD treatment should be considered first, not only to limit the local progress of the pathology, but also for halting PsA’s typical progression [54].
If these measures are not successful in alleviating the patient’s symptoms, a referral to a specialist in oral and maxillofacial surgery is warranted. Depending on the type and localization of the symptoms, second line treatment measures can potentially be implemented.
Thus, in the presence of pain affecting the muscles of mastication, topical measures, including the injection of these muscles with botulinum toxin, or long-acting local anaesthetic agents can be attempted [22, 71]. A low-dose antidepressant of 10 mg amitriptyline once daily may also help [22, 71].
When the pain is mostly localised in the joint and/or symptoms like locking are present, the joint can be injected with long-acting local anaesthetic agents. Injection of the joint with glucocorticosteroids can be also attempted, but only when there is evidence of active inflammation of the joint (seen in an MRI scan or during a diagnostic arthroscopy).
The injection of glucocorticosteroids should be undertaken with caution and should ideally be limited to only one or two attempts as there are cases where significant bone resorption and alteration of the condylar anatomy have been described following such a treatment [22].
Failure of the second line treatment measures in patients with refractory pain localized in the joint and/or limited mouth opening, can be followed by third line treatment measures such as arthrocentesis and arthroscopy [22, 71].
Arthrocentesis is the least invasive of the two and involves the placement of two needles in the joint space, via which lavage of the joint can be performed. In the end of the procedure injection of the joint with local anaesthetic agents (or, if appropriate glucocorticosteroids) can also be performed. Arthrocentesis removes debris and inflammatory factors from the joint and can passively loosen adhesions that might be present. It has been found that it can help a significant proportion of patients with their symptoms [22, 71].
Arthroscopy involves the insertion of an arthroscope in the joint, via which lavage can be performed under direct vision. Arthroscopy has an added diagnostic benefit and can help with diagnosing a number of TMD conditions. Few surgeons are trained to perform interventional arthroscopy, where debris can be removed, the disc can be plicated, or adhesions actively loosened and even less evidence exists as to the efficiency of such procedures [22, 71].
Arthroscopy and arthrocentesis can be performed repeatedly and can help controlling TMD symptoms of the patients for long. A select cohort of patients that have symptoms refractory to minimally invasive procedures may require open joint surgery that includes procedures such as eminoplasty (the remodelling of the anterior articular eminence), eminectomy (the removal of the anterior articular eminence), disc plication to address disc displacement, discectomy to remove a damaged, perforated disc, and adhesiolysis.
Although initially having good results, all these procedures have been associated with secondary degeneration of the joint elements and should only be employed after careful consideration [22, 71].
The last step in the management of chronic TMD problems is total joint replacement. Significant evidence now shows that this is a procedure that, when indicated, can help patients deal with their long-standing problems. In the UK [72] the guidelines dictate that a person is a candidate for TMJ replacement if they experience TMJ pain, locking, reduced mouth opening, decreased dietary intake because of their TMD, radiographic evidence of disc derangement, and all conservative or surgical treatment has failed.
There are several joint systems available nowadays, with the main distinction being between off-the-self and custom-made prosthesis, with the latter being bound to dominate the future market [73]. The general trend at the moment is towards custom-made, patient-specific prostheses [22, 74–79].
Conclusive remarks
The aim of the current narrative review is to address the involvement of TMJ in SpA. In this group of arthritis, accumulating evidence suggests that TMJ is frequently affected in the process of inflammation.
However, it is often underestimated and overlooked by clinicians, unless complains are made by the patients, or severe disability affecting quality of life is noticed. Chronic pain in other joints, impaired mobility, other organ involvement and depression are some of the reasons that patients often underestimate TMJ symptoms [71].
It is becoming obvious that proper clinical assessment, including careful history taking around TMD, TMJ examination and appropriate imaging depending on the available modalities can enable a prompt diagnosis of inflammation in TMJ.
Temporomandibular disorders diagnostic criteria provide useful guidance for thorough evaluation of TMJ by rheumatologists in outpatient clinics or private practice. They are easy to follow and do not require special training or long-lasting experience.
Basic clinical examination, testing basic compartments of the joint and its mobility is not time consuming and can be easily included in the assessment of the patient along with other joints. Finally, pain and impact on quality of life should be separately and carefully addressed. The Visual Analogue Scale score for pain and HAQ score for quality of life could be useful tools.
As mentioned above, panoramic radiographs can be used for screening as well as ultrasound when available in routine practice. For symptomatic patients MRI is believed to be the best technique, as it allows assessment of enthesitis, US and CBCT in some cases.
Plain radiographs are not of particular value except the assessment of cervical vertebrae alignment, craniocervical distance and profound ossification. However, a baseline X-ray has a place in the assessment which can be repeated during the general assessment of the patient depending on the symptoms.
Conservative management and early pharmacological treatment can prevent permanent joint impairment and its debilitating consequences for patients’ daily life. For refractory cases, early OMF referral and assessment should not be delayed as surgical management can release ankylosis.
Conclusions
Temporomandibular joint shares some common anatomic features with other joints dominantly affected by spondylarthritis, like sacroiliac joints and pubis ramus. In this context, it is not surprising that there is evidence of high prevalence of TMD in patients with spondylarthritis.
Moreover, this finding generates questions whether TMJ should be part of initial screening with imaging especially in cases of non-radiographic axial spondylarthritis or peripheral arthritis where there are other features of the disease and evidence of joint inflammation is required to enable/potentiate the diagnosis for proper initiation of treatment.