Introduction
Systemic lupus erythematosus (SLE) is a relapsing-remitting autoimmune disorder, mainly seen in women of reproductive age and has a female to male ratio of 9 : 1 [1, 2]. The prevalence of SLE is on the rise and estimated to be 52.2 per 100,000 in the US, which has been attributed to increased survival as well as detection of milder diseases [2]. Systemic lupus erythematosus is more common in African-American and African Caribbean ethnic groups [2].
The most common manifestation of SLE is arthritis which is seen in almost half the patients with SLE, followed by malar rash [2]. Of note, SLE is a multisystem disorder that affects multiple organs and can have varying presentations such as pericarditis, central nervous system disturbances, nephropathy, retinopathy and gastrointestinal symptoms [2–5]. Moreover, psychiatric manifestations including depression and anxiety are commonly seen in SLE patients [6]. As such, depression is almost twice more common in patients with SLE compared to the general population [7]. Anxiety is also reported to be two times more common in patients with SLE as compared to controls [7]. The impact of depression and anxiety is beyond the disease itself and is associated with higher cardiovascular events, myocardial infarction, premature mortality, and suicidal ideation, among many other conditions [7]. Depression is associated with non-compliance with medication which in turn increases service utilization, in particular, visits to the emergency department [8].
With the increase in life expectancy of patients with SLE, there has been more emphasis on quality of life [1]. The reduction in quality of life in patients with SLE is more prominent than other chronic diseases such as diabetes mellitus and myocardial infarction [9]. Systemic lupus erythematosus is likely to affect psychological, social, and physical aspects of patient’s life. Therefore, it is important to evaluate the patient’s perspective and quality of life in addition to disease activity [10].
The reported prevalence of neuropsychiatric manifestations in SLE ranges from 12% to 94% across different studies [7, 11]. The current literature is widely heterogeneous regarding the prevalence of psychosocial disturbances in patients with SLE. Therefore, the primary aim of this study was to evaluate the prevalence of depression, anxiety, stress and general health, and also quality of life in patients with SLE and assess the associated demographic factors.
We hypothesize patients with SLE have higher levels of depression, anxiety and stress per the Depression Anxiety and Stress Scale-42 (DAS-42) questionnaire, worse general health based on GHQ-28 questionnaire as well as lower quality of life per WHO-QOL BREF questionnaire.
Material and methods
This is a cross-sectional study conducted at Shahid Sadoughi Medical Center in Yazd, Iran, from 2017 to 2019. This study was approved by our institutional review board (IRB).
The SLE data registry at our institution was searched for qualified patients. Exclusion criteria were patients younger than 18 or older than 80 years and those diagnosed with overlap disease. We included patients who were diagnosed with SLE based on The Systemic Lupus International Collaborating Clinics (SLICC) criteria. The diagnosis of SLE was re-evaluated and confirmed by a second rheumatologist. Qualified candidates were subsequently contacted and asked to participate in the study. After explaining the methods and objectives of the study in detail, informed consent was obtained from those interested in participating.
Clinical presentation and demographic data were collected from the data registry by a trained physician using prepared forms. The following parameters were collected: age, marital status (single, married, divorced, widowed), and education level (lower than high school, high school diploma, associate degree, bachelor’s degree, higher than bachelor’s degree). Patients were asked to complete the three following questionnaires: 1) general health questionnaire (GHQ-28), 2) DASS-42, 3) World Health Organization quality of life instrument short form(WHO-QOL-BREF). We used the Farsi version for all of the questionnaires.
The GHQ was created in 1970 by Goldberg et al. [12], and is a widely used self-administered questionnaire that aims to evaluate subjective emotional stress and to investigate the wellbeing of patients during the last four weeks [12, 13]. The GHQ-28 consists of 28 questions in total with the following four subscales: 1) somatic symptoms, 2) anxiety and insomnia, 3) social dysfunction, 4) severe depression [12, 13]. This tool explores the frequency of symptoms during the past few weeks, with scores ranging from 0 to 3 [12]. The overall score ranges from 0 to 84, and higher scores represent more distress [12, 13]. Patients were classified as having distress if they had scores of 24 or above [12, 13].
The DASS-42 is a self-report questionnaire with 42 questions that is used to evaluate the severity of depression, anxiety, and stress. Each question is measured on a 4-point scale (0 to 3) that corresponds to the magnitude of the symptom during the last week [14]. Higher scores indicate more severe symptoms [14]. Depression scores of 0–9 are considered normal, while those with scores of 10–13 have mild depression, 14–20 moderate depression, 21–28 severe depression, and more than 28 extremely severe depression. Anxiety scores of 0–7 are considered normal, while patients with anxiety scores of 8–9 have mild anxiety, 10–14 have moderate anxiety, 15–19 have severe anxiety, and more than 20 have extremely severe anxiety. Stress scores of 10–14 are considered normal, while those with stress scores of 15–18 have mild stress, 19–25 have moderate stress, 26–33 have severe stress, and more than 34 have extremely severe stress.
The WHO-QOL-BREF was created to assess the quality of life in a cross-cultural setting [15]. It evaluates the patient’s view on their situation in life while considering cultural values [10]. This questionnaire attempts to evaluate the quality of life in four domains of psychological and physical health, social relationships, and environmental health [15]. This questionnaire is scored on a Likert scale of 1 to 5 with a highest possible score of 20.
Statistical analysis
Statistical analysis was done with IBM SPSS Statistics for windows version 23. Categorical variables are presented as frequency and percentage. Categorical variables were compared with Chi-square. Multiple linear regression was used to evaluate the association of general health scores with depression, anxiety, and stress. Pearson’s correlation coefficient was used to evaluate the association of general health scores with various continuous variables. For continuous variables, t-test was used to compare two groups and ANOVA to compare variables with more than two groups. P-value of less than 0.05 was considered significant.
Bioethical standards
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences (IR.SSU.MEDICINE.REC.1398.202). After taking written consent from patients, we collected data. In addition, this study was done according to the Declaration of Helsinki. All interventions were performed with the aim of treating the patients and no additional interventions were done. In addition, no additional cost was imposed on patients. Additionally, in case of unwillingness, patients were excluded from the study.
Results
A total of 222 participants were included in the study. Patients had a mean age of 35.6 ±9.5 years; 203 patients (91%) were females, while 19 (9%) were male. Baseline characteristics are presented in Table I.
Table I
Baseline characteristics
Depression Anxiety and Stress Scale-42 questionnaire
Depression
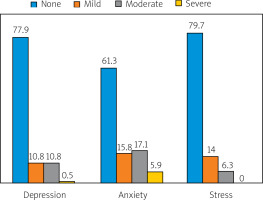
According to DASS-42 questionnaire, 173 patients did not have depression (77.9%), 24 (10.8%) patients had mild, 24 (10.8%) had moderate, and 1 (0.5%) had severe depression. The overall mean depression score was 5.14. Depression score was significantly higher in women compared to men (p = 0.014). Depression was not significantly associated with age, education, or marital status. The DASS-42 scores are summarized in Table II.
Stress
The overall mean stress score was 8.95. One hundreed and seventy-seven patients did not report any stress, and 45 reported some degree of stress. The mean stress score was not significantly different between men and women. Stress was significantly higher in divorced patients compared to those who were single, married, or widowed (p = 0.037). Stress was not significantly associated with age and education level.
Anxiety
The mean anxiety score was 6.3 overall. One hundred thirty-six patients did not report any anxiety, and 86 reported some degree of anxiety. Anxiety was not significantly different between men and women. Anxiety score did not show a significant association with age, marital status, and education level.
Quality of life (WHO-QOL BREF)
Physical health
Quality of life score in the physical health domain was 12.87 overall. Physical health showed a significant negative association with age, while it did not show a significant association with marital status, education level and sex.
Quality of life subscale scores based on WHO-QOL BREF questionnaire are summarized in Table III.
Table III
Quality of life subscale scores based on WHO-QOL BREF questionnaire
Psychological health
The overall quality of life score in the psychological health domain was 13. This score was significantly different between men and women who had a score of 14.14 and 12.9, respectively (p = 0.034). Psychological health was also significantly higher in patients with a higher level of education (p = 0.035); however, it was not associated with marital status.
General Health Questionnaire
Mean score of general health based on GHQ-28 questionnaire was 27.25, overall. The 85 patients (38%) did not report any distress, while 137 (62%) reported some degree of distress.
General health score was not significantly different between men and women. Moreover, the GHQ-28 score was not significantly associated with education level and marital status; however, it was negatively correlated with DASS-42 scores of depression (p = 0.001), anxiety (p = 0.001), and stress (p = 0.001).
Discussion
In this study, we aimed to evaluate the prevalence of anxiety, depression, and stress in patients with SLE and also assess self-reported quality of life in these patients. In our study, 61.7% of participants reported some degree of psychological distress assessed through the GHQ-28 questionnaire. We found the prevalence of self-reported depression, anxiety, and stress to be 22.1%, 28.7%, 20.3% based on the DASS-42 questionnaire. We also evaluated the quality of life using the WHO-QOL BREF questionnaire.
The risk factors contributing to mood disorders in SLE patients are not entirely understood [16]. Mood disorders in SLE may happen as a direct result of disease activity or secondary to other conditions such as glucocorticosteroid therapy, disease symptoms, or psychological pressure of living with a chronic disease [17–19]. Autoantibodies such as antiphospholipid, anti-endothelial, anti-neuronal, and anti-ribosomal P antibodies may also play a role in depression in patients with SLE. Depression in SLE is also associated with cytokines such as tumor necrosis factor α (TNF-α) [20]. Environmental and genetic elements may also contribute to the neuropsychiatric manifestation of SLE [17–20]. The study of Montazeri et al. [13] presented the validation of 12-item GHQ questionnaire for Iranian population, which is quite simple and easy to complete. However 28-item GHQ was also validated by studies conducted in Iran [21–23].
In our study, 62% of participants reported some degree of psychological distress, as assessed by GHQ-28 questionnaire. A meta-analysis reported the prevalence of anxiety and depression in patients with SLE to be 40% and 30%, respectively which is higher than that in the general population [7, 20]. Another study reported the prevalence of anxiety (40%) to be higher than depression (15%) in patients with SLE [16]. Similarly, in our study, the prevalence of anxiety (28.7%) was higher than depression (22.1%). A previous study reported depression, anxiety, and stress to be associated with age, sex, education, and marital status in the general population [17]. Conversely, we did not find a significant association between anxiety with age, sex, education, and marital status.
Literature is inconsistent about the impact of marital status, age, sex, and education level on anxiety and mood disorders in patients with SLE. A study of 285 Chinese patients with SLE reported higher suicidal ideation in divorced and widowed patients [24]. In this study, we found that stress was significantly higher in divorced patients and depression was significantly more prevalent in women compared to men.
Quality of life scored according to the WHO-QOL BREF self-questionnaire was 12.87 in physical activity, 13.0 in psychological health, 14.35 in social relationships, and 13.96 in the environmental domain. A previous meta-analysis evaluated the quality of life in patients with SLE and reported lower quality of life compared to the general population, with physical health more affected than mental health [19]. Consistently, in this study, the quality of life score was lowest in the physical activity domain. Moreover, the QOL score in physical activity was 12.87, lower than 16.2 previously reported in the general population [20]. The social relationship score (14.3) was similar to the previously reported 14.3, in a study in general population [19].
We also explored the association of age, marital status, level of education, and sex with quality of life in patients in our study. Similar to previous studies, there was a negative correlation between social relationships and age [19]. Similarly, environmental health was also negatively associated with age. There was no association between environmental health, physical health, and social relationships with sex, age, marital status, and education level. Psychological health was significantly higher in more educated patients. Of note, psychological health scores were also higher in men compared to women.
Quality of life is substantially reduced in patients with SLE, therefore evaluating QOL in these patients provides information on their mental and physical status and helps to improve management and treatment [25].
Non-pharmacological interventions may be considered for the management of psychological symptoms in patients with SLE [2]. Treating depression and managing stress and insomnia can improve fatigue, which is commonly seen in patients with SLE [2]. Moreover, depression and ineffective coping mechanisms can negatively affect the management of chronic diseases [2, 7]. Of note, depression and anxiety can lower quality of life and increase the rate of cardiovascular diseases and mortality [7]. Therefore, it is important to screen for depression in patients with SLE and consider medical management and psychological referral if necessary [2]. Depression and anxiety symptoms are also associated with lack of knowledge about the treatment and disease itself. Linking patients with available support groups could help reduce the frustration of gathering information through unreliable resources [2, 26, 27].
In Figure 1 the numbers represent percentage of affected by depression, anxiety and stress patients were presented.
Study limitations
Our study has some limitations. First it is single center study. Second, we did not include a control group. Third, as with all cross-sectional studies, we could not draw causal inferences.
Conclusions
In the study of 222 patients, we found that depression, anxiety, and stress are common in patients with SLE, and quality of life is significantly affected. Moreover, a high percentage of patients with SLE deal with some degree of distress. Routine evaluation of the quality of life and psychological disturbances, including depression and anxiety, is recommended in patients with SLE. Non-pharmacological interventions and specialist referral, should be considered in patients with anxiety, depression, or stress.