Introduction
Low back pain (LBP) is a major public health concern globally transcending ages, occupations, and socioeconomic backgrounds [1]. It is a prevalent musculoskeletal problem, with up to 84% of adults experiencing it at least once in their lives [1]. Low back pain has become a primary cause of disability and work absenteeism worldwide, leading to significant economic challenges and reduced productivity [2].
It ranks second only to the common cold as a reason for physician visits and is the fifth leading cause of hospital admissions [2]. Studies suggest that women are at a higher risk of experiencing different clinical pain conditions, including LBP [3].
The prevalence of LBP is globally estimated to be 7.5% based on age-standardization, with a lifetime prevalence ranging from 70% to 85% [2, 4]. A systematic analysis of 65 epidemiological studies conducted in Africa revealed that the pooled lifetime, annual, and point prevalence of LBP on the continent were 47%, 57%, and 39%, respectively [5].
In Nigeria, a review showed that the 12-month prevalence of LBP was between 32.5% and 73.53% [6]. Low back pain ranked among the top 10 contributors to Disability-Adjusted Life Years (DALY) in the 2019 Global Burden of Disease (GBD) Study, resulting in significant healthcare costs each year [7].
There are several contributing factors to LBP including ergonomic, sociodemographic, and psychosocial factors. Job-related factors like prolonged sitting, heavy lifting, poor posture, and bending contribute to LBP. Psychological elements such as depression and anxiety, along with obesity, physical inactivity, smoking, aging, and being female, are among multiple factors associated with LBP development [8].
There are multiple causes of LBP, encompassing mechanical factors like muscle strains, compressed nerves, herniated discs, and degenerative changes. Inflammatory conditions, infections, and tumors are non-mechanical contributors. Referred pain from internal organs like kidneys and gallbladder can contribute to LBP [9].
In certain instances, LBP may be associated with psychological conditions such as fibromyalgia and somatoform disorders or may serve as an indicator of serious medical conditions such as infections, malignancies, or other systemic diseases [2, 10].
The management of LBP varies based on its underlying cause and occurs at different healthcare levels. Treatment involves both pharmacological and non-pharmacological approaches. In Africa, rest and analgesia are the most prevalent approaches, though evidence indicates that active rehabilitation through guided physical exercise is more effective in reducing recurrence and chronicity.
The most effective strategy involves a multidisciplinary and multimodal approach, offering comprehensive therapy to alleviate pain, enhance function, and address pain-generating mechanisms to reduce the likelihood of recurrence [1, 11].
Understanding the epidemiology of LBP in various settings can improve care optimization and promote preventive strategies. In Sub-Saharan Africa, published research is scarce, particularly in rural areas. The study aimed to determine the prevalence, etiology, risk factors, and presentation patterns among patients with LBP in a Teaching Hospital in South-South Nigeria.
Material and methods
Study design, setting, and population
This was a hospital-based descriptive, retrospective study conducted over 5 years from January 2018 to December 2022 at the rheumatology outpatient clinic of the Irrua Specialist Teaching Hospital (ISTH), Irrua, Edo State in South-South Nigeria. The hospital serves as a reference facility, catering to all categories of patients in the surrounding towns and states. It is recognized as a center of excellence for the diagnosis, management, and control of viral hemorrhagic fever and emergent pathogens.
The study population consisted of patients who presented with LBP in the rheumatology clinic of the hospital during the outlined study period. However, patients with incomplete or missing data and pregnant women were excluded from the study.
Data collection
The case records of all patients with LBP between January 2018 and December 2022 were retrieved from the medical records and thoroughly examined. Extracted data included patients’ sociodemographic profiles, duration of LBP at presentation, predisposing factors, associated symptoms, comorbid conditions, body mass index (BMI), diagnosis, and Oswestry disability index (ODI) scores. Low back pain was classified based on its duration at presentation into three categories: acute (0–6 weeks), sub-acute (7–12 weeks), and chronic (> 12 weeks) [2].
The ODI is a valid, reliable, and responsive clinical tool routinely measured in the rheumatology clinic for patients with LBP. It is designed to assess a patient’s level of function or disability associated with LBP. The ODI evaluates perceived disability in 10 everyday activities: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sexual activity (if applicable), social life, and travel.
Each category contains 6 statements with scores ranging from 0 to 5, where 0 indicates the least disability and 5 indicates the most severe. The maximum possible score is 50. This total score was converted into a percentage by multiplying it by 2.
Severity was categorized as follows: 0–20%, minimal disability; 21–40%, moderate disability; 41–60%, severe disability; 61–80%, crippling back pain; and 81–100%, bed-bound patients or those exaggerating their symptoms. For results to be considered clinically significant, there must be a change of 10% or more in a patient’s score [12].
Statistical analysis
Data entry and analysis were performed using the IBM Statistical Package for the Social Sciences (SPSS®) version 25 for Windows. Continuous variables were presented as means and standard deviations, while categorical variables were summarized as frequencies and percentages. The association between variables was assessed using Pearson’s χ2 and/or Fisher’s exact test. A p-value of less than 0.05 was considered statistically significant.
Results
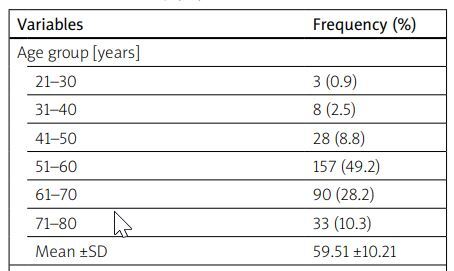
During the study’s timeframe, 1,580 patients visited the rheumatology clinic, with 319 reporting LBP, resulting in a frequency of 20.2%. The study group had a mean age of 59.51 ±10.21 years, with 196 (61.4%) females and 123 (38.6%) males, resulting in a 1.5 : 1 female-to-male ratio.
The 51–60 years age group was the most affected, comprising 49.2% of LBP patients. Among these patients, 105 (32.9%) were farmers, 91 (28.5%) were traders and 74 (23.2%) were civil servants. In terms of BMI, 126 (39.5%) were overweight, and 54 (16.9%) were classified as obese. Detailed sociodemographic and anthropometric characteristics are represented in Table I.
Table I
Sociodemographic and anthropometric characteristics of the study population
The most prevalent risk factors for LBP in this study were primarily work-related, constituting 47.3% of cases. Within this category, heavy lifting contributed to 26.3%, prolonged sitting to 19.4%, and poor posture to 27.9%. Additional risk factors included obesity (16.9%), previous back injury (12.2%), and sedentary behavior (11.55%).
The risk remained undefined in 14.4% of patients. Notable symptoms encompassed difficulty standing or bending (73.0%), walking difficulties (67.7%), sleep disruptions (51.4%), and radicular pain (45.8%). Table II shows the risk factors and clinical manifestations of the study patients.
Table II
Risk factors and clinical features of the study population
The mean duration of LBP at presentation was 3.38 ±4.33 years. The cases of LBP were categorized as acute in 39 (12.2%) patients, subacute in 25 (7.8%) patients, and chronic in 255 (79.9%) patients. In this study, 293 (91.8%) had some form of imaging, with 226 (70.8%) and 67 (21%) having spine radiographs and magnetic resonance imaging (MRI) scans, respectively.
The ODI assessment revealed that 91 (33.5%) patients had minimal disability, 121 (44.5%) had moderate disability, 42 (15.4%) had severe disability, and 18 (6.6%) were categorized as crippled. Table III shows the clinical characteristics of the study patients.
Table III
Clinical characteristics of the study population
Various causes of LBP were observed, with spondylosis being the most prevalent, affecting 212 (66.5%) patients. Other contributing etiologies included spondylolisthesis (22.3%), disc prolapse (19.4%), spinal canal stenosis (15.4%), muscle spasm (12.2%), and tuberculous spondylitis (9.7%).
A significant sex disparity was noted, favoring males, in the incidence of spondylolisthesis (p < 0.001), disc prolapse (p < 0.001), muscle spasms (p = 0.002), tuberculous spondylitis (p = 0.019), and metastatic spine tumors (p < 0.001).
While conditions like spondylosis (p = 0.950), spinal canal stenosis (p = 0.356), and back strain (p = 0.800) were more common in females, these differences did not reach statistical significance. Table IV shows the etiology of LBP in the study patients.
Table IV
Etiology of low back pain in the study patients
| Etiology | Sex | Total n (%) | p-valueϖ | |
|---|---|---|---|---|
| Male n (%) | Female n (%) | |||
| Nonspecific | ||||
| Spondylosis | 82 (66.7) | 130 (66.3) | 212 (66.5) | 0.950 |
| Spondylolisthesis | 43 (35.0) | 28 (14.3) | 71 (22.3) | < 0.001 |
| Muscle spasm | 24 (19.5) | 15 (7.7) | 39 (12.2) | 0.002 |
| Back strain | 13 (10.6) | 19 (9.7) | 32 (10.0) | 0.800 |
| Specific | ||||
| Tuberculous spondylitis | 18 (14.6) | 13 (6.6) | 31 (9.7) | 0.019 |
| Metastatic spine tumor | 9 (7.3) | 0 (0.0) | 9 (2.8) | < 0.001# |
| Fibromyalgia | 0 (0.0) | 5 (2.6) | 5 (1.6) | 0.161# |
| Ankylosing spondylitis | 2 (1.6) | 1 (0.5) | 3 (0.9) | 0.561# |
| Back pain with neurologic dysfunction | ||||
| Disc prolapse | 43 (35.0) | 19 (9.7) | 62 (19.4) | < 0.001 |
| Spinal canal stenoses | 16 (13.0) | 33 (16.8) | 49 (15.4) | 0.356 |
Discussion
The prevalence of LBP is rising in Africa, becoming a significant public health concern. While the understanding of the epidemiology of LBP in Sub-Saharan Africa is advancing, research in rural regions remains limited. The prevalence of LBP in Sub-Saharan Africa varies across studies, possibly due to factors such as social dynamics, economic disparities, study populations, and methodologies [6].
In this study, LBP frequency was 20.2%, notably higher than other reported rates in previous studies [13, 14]. Variations were observed, with a family practice clinic in Ibadan reporting a frequency of 46.4% [15]. The global occupational prevalence of LBP as reported by Punnett et al. [16] is 37%.
The mean age of the study patients was 59.5 years, and LBP was more prevalent among individuals aged 51–60 years. This aligns with the 2019 GBD estimate, which indicated a higher occurrence of LBP cases between the ages of 50–55 years [7]. Similar findings were observed in the research conducted by Katembo et al. [17] in Tanzania and Eromon et al. [14] in Nigeria.
Previous studies by Eyichukwu and Ogugua [18] and Omoke and Amaraegbulam [19] noted a peak age incidence of LBP in the 31–40-year and 42–50-year age groups, respectively.
Conversely, Edomwonyi and Ogbue [13] reported the highest incidence of LBP in the 61–70-year-old age group. The impact of LBP on social and occupational activities is significant for individuals under 60 years old, who are actively engaged in work and daily activities [20].
Previous studies have shown diverse patterns of sex distribution in LBP, likely influenced by socioeconomic factors, study demographics, occupations, and research methods. In this study, LBP was more prevalent among females (61.4%) than males (38.6%), consistent with some previous research [14, 18].
However, contrasting findings of male predominance have also been reported [15, 17]. The suggested reason for this is that men often engage in occupations involving intense physical exertion and whole-body vibration, in contrast to women [16]. In rural agricultural settings, economic conditions drive women to engage in physically demanding tasks, either to support men or due to entrenched sociocultural norms designating them as primary family providers [21].
The link between LBP and female sex might relate to pregnancy and childbirth, though this association remains obscured. Recent studies suggest childbirth could influence later-life LBP risk due to hormonal changes and lumbar posture alterations during pregnancy [22].
Research suggests that women who have given birth when compared to those who are yet to give birth may face a higher risk of chronic LBP as they age, contributing to the observed higher prevalence of LBP among females in the study [22].
Globally, back pain constitutes 37% of DALY, affecting work productivity and economies [23]. Physical factors like manual labor and exposure to vibrations contribute to LBP [24]. This study echoes the findings of earlier studies, identifying job-related factors as the primary contributor to LBP [17, 18].
Most of the study patients engaged in farming, civil service, or trading, consistent with earlier studies [13, 19]. Common factors such as heavy lifting, prolonged sitting, and poor posture were identified in this series. Studies by Ogunbode et al. [15] and Omokhodion et al. [25] also associated LBP with occupational activities, bending, and poor posture. In Thailand, rice farmers experienced increased LBP from slouched sitting, forward bending, and lifting [26].
Sedentary habits contribute to LBP development in this study, aligning with previous research [13, 18]. Certain sedentary occupations, such as office jobs and long-distance travel, can contribute to LBP from prolonged sitting [27].
Sedentary behavior, known for its well-documented health implications like cardiovascular problems and premature mortality, is equally acknowledged as an independent risk for experiencing musculoskeletal discomfort [27]. Balancing job demands and spinal health is crucial for those with work-related LBP, and in resource-limited settings, measures like ergonomic structures, back health education, and assistive equipment can help mitigate occupational hazards.
Obesity is a recognized factor contributing to LBP, often linked to a sedentary lifestyle. This study found that 16.9% of patients were obese and 39.5% were overweight. Research has shown a correlation between obesity and LBP incidence [28]. Substantial weight gain can intensify pressure on the lower back, potentially causing lumbar disc herniation and LBP.
Non-specific LBP accounted for most cases of LBP in our series consistent to the findings of earlier studies [13, 18]. Spondylosis, a non-specific LBP stands out as the most prevalent etiology of LBP in this study, similar to the findings of previous studies [13, 18]. It’s important to highlight that a majority of LBP cases, surpassing 80%, were associated with mechanical factors. Among these mechanical causes, spondylosis remained the most prevalent, aligning with the findings of previous studies [10, 13, 18].
However, in the United States, lumbar strain or sprain accounts for around 70% of mechanical LBP cases [29]. This divergence could be attributed to the referral pattern of our patient cohort. A significant proportion of our patients are referred from primary and secondary healthcare facilities. Consequently, individuals with mild lower back strain may have already experienced favorable responses to treatment during these earlier stages, potentially resulting in fewer cases presenting at the rheumatology clinic. Tuberculous spondylitis, occurring in 9.7% of cases, was more common in males, similar to earlier reports [19].
The primary manifestations observed among the study patients were difficulty with walking, standing, or bending. Over 50% of LBP patients experienced sleep disturbances. Research links LBP to insufficient sleep duration and quality. Consequently, integrating sleep improvement into LBP management offers valuable benefits [30].
Around 50% of the study patients had radicular pain. Varied rates of radicular pain have been reported in previous studies [18, 19]. Notably, Katembo et al. [17] reported a rate as high as 84.2%. Radicular pain may arise from mechanical pressure, nerve compression, or inflammatory mediators due to damaged discs [31].
In primary care, most acute LBP cases respond well to treatment, resolving completely [32]. The transition to chronic LBP varies (2–34%) [32, 33], but this study recorded a high rate of chronic LBP (79.9%), akin to findings of 73.1% in South-East Nigeria [18].
The high rates of chronicity in this study may be due to delayed hospital visits, linked to self-treatment, use of unorthodox healthcare, financial constraints, and poor accessibility to healthcare facilities [18]. Educating the public about timely medical attention and proper LBP treatment to prevent recurrence and chronicity is crucial.
Plain radiography is the most common imaging method in resource-limited settings, due to its affordability and accessibility. Most patients (70.5%) had spine X-rays, while 21% had MRI scans for more comprehensive neural elements, spinal cord, and discs. A few (8.2%) had no imaging and relied solely on clinical diagnosis due to high costs and limited MRI availability. These trends align with findings from Edomwonyi and Ogbue [13, 18].
Low back pain can lead to significant functional disability. In this study, 85.3% of patients had some disability, consistent with the findings of Katembo et al. [17] and Kortor et al. [34]. Salvetti et al. [35] reported a disability rate of 65%, while Barry et al. [36] and Webb et al. [37] reported 40% and 56% disability rates, respectively. The higher disability rate in this study emphasizes the impact of LBP on individuals and society.
Differences in disability rates across studies could be due to varying definitions and assessment tools for disability assessment. In this study, most patients (78%) had moderate to severe disability, consistent with prior research [17, 34, 35]. Individuals with disabilities may often manifest psychological symptoms including depression. It has been shown that patients with chronic LBP commonly exhibit high rates of depressive symptoms [38].
Hypertension is the main comorbidity in this study. Chronic painful conditions like LBP have been linked to higher hypertension risk [39]. This study found that 29.8% of LBP patients had hypertension, comparable to a previous report [14].
Another comorbidity is peptic ulcer disease, and this may significantly affect analgesic choice. Caution is therefore needed with the use of non-steroidal anti-inflammatory drugs in LBP patients with peptic ulcer disease and hypertension. As age increases, chronic conditions like hypertension, diabetes, and obesity have been shown to impact the development of tendon and ligament injuries, contributing to LBP occurrence [28].
Study limitations
Given the descriptive nature of this study, it’s not possible to eliminate the influence of cofounders. Furthermore, because it is conducted within a hospital setting, the applicability of the data to the broader population may be limited. Incomplete documentation and occasional absence of files and records may present issues.
Conclusions
Low back pain is a frequent catalyst for work absenteeism and functional disability, posing a significant public health concern. Mechanical and non-specific causes underlie a larger portion of LBP cases in our environment.
Work-related aspects, such as heavy lifting, poor posture, and prolonged sitting, increase LBP risk. Individuals prone to LBP at work should prioritize posture adjustments to minimize excessive bending and stretching movements.