Introduction
Often, during the therapeutic process of musculoskeletal system pathologies, including the spine, various medical procedures are performed to eliminate the cause.
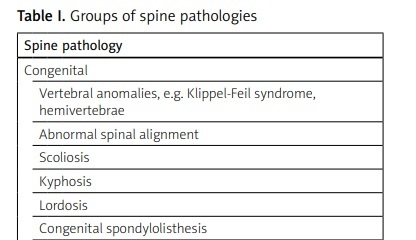
Targeted treatment to remove the cause of the disease or dysfunction should be the main goal of management. The success of such treatment is possible if it is directed at the pathology that is the cause of the symptoms, especially in the case of acquired spine pathologies such as discopathy or spondylosis [1]. The main groups of spine pathologies are presented in Table I.
Table I
Groups of spine pathologies
Sometimes only symptomatic treatment is used. In most cases, conservative treatment is applied, but in some cases surgical treatment is implemented. However, attention is not always paid to the risk factors of the development of a given disease. Isolated treatment of musculoskeletal disorders may be insufficient. Taking into account the fact that spine diseases are nowadays becoming civilization diseases, they require a comprehensive approach, starting with the risk factors causing frequent spine pain, malfunctioning, depression, social withdrawal or work absence [2]. Their reduction, or at least modification, makes it possible to maintain effective medical treatment based on both conservative and surgical approaches. Then, the implementation of physiotherapy, in the broad sense, aimed at a specific pathology allows the good treatment effect to be maintained, paying particular attention to an individual approach to each patient [3]. The proposed three-stage treatment concept is presented below. The regime discussed in this paper takes into account three stages: The first is reduction/modification of the risk factor(s) for musculoskeletal system disorders, including the spine. The second stage involves the inclusion of medical therapy in the broad sense. Then the third stage is based on the implementation of targeted rehabilitation, especially kinesiotherapy, importantly, introduced when appropriate, depending on the type of pathology and the medical therapy used. It should be emphasized that in the process of treating spine disorders (SD), apart from doctors and physiotherapists, nurses, psychologists, social workers and other specialists also play an important role.
The aim of this paper is to discuss the question of comprehensive treatment of acquired noninflammatory SD focusing on a three-stage treatment concept.
Stage 1
Assessment of risk factors
Lack of regular physical activity, sports and a sedentary lifestyle are very important risk factors for spine pathologies, including frequently diagnosed discopathy. Already in the early years of life, atrophy of blood vessels in the intervertebral discs occurs and the region is nourished by the diffusion of surrounding tissues. The more physically active the child is, the better is the process of nourishing the intervertebral discs. If children do not exercise or play sports, they spend many hours at school and then using the computer. In consequence, these factors provide a basis for the development of discosis – i.e. the formation of degenerative lesions within the intervertebral discs. Subsequently, degenerative changes in the spine may occur due to discopathy [4]. We can influence many risk factors, known as modifiable factors. These include, among others: physical activity, sedentary and overloading lifestyle, smoking, a non-ergonomic workstation where we spend many hours during the day or throughout our lives. Fixing the monitor at an incorrect height, or incorrect use of a mobile phone at flexion, causes overload of the cervical spine [5, 6]. The overload level vs. flexion angle is presented in Table II.
Table II
| Flexion angle between chin and sternum | 0º | 15º | 30º | 45º | 60 º |
| Cervical spine overload | 4–5 kg | Approx. 12 kg | Approx. 18 kg | Approx. 22 kg | Approx. 27 kg |
Unfortunately, nowadays, when the use of electronic devices is so common, it is practically impossible to eliminate these factors, but it is possible to modify them to some extent. For example, if a doctor recommends an accountant to quit the use of a computer, it is practically impossible. Therefore, this stage should be based on the adjustment of modifiable factors. Table III presents examples of modifications of risk factors for back pain syndromes.
Table III
Examples of risk factors causing spine overload and their modifications
The case is a bit more difficult for non-modifiable factors. We cannot significantly influence these factors, so any adjustments of modifiable factors may partially support this stage. The non-modifiable factors include mainly: age, patient’s predispositions (e.g. immune disorders – higher risk of infection, hematological disorders – higher risk of bleeding, hematoma) and genetic factors.
Stage 2
Pharmacotherapy
Medical therapy in the broad sense is an almost fixed element of SD treatment. Very often, analgesics, anti-inflammatory drugs, myorelaxants and vitamin pharmacotherapy are used. However, it should be clearly stated that the use of analgesia alone, i.e. only symptomatic treatment, is insufficient. In consequence, it may have a negative impact on the patient by pain attenuation and delay diagnosis and targeted treatment implementation. According to the latest literature, rest and pharmacotherapy do not play a key role in the treatment of back pain syndromes. Physical activity and multidirectional treatment are recommended [9]. During exacerbations, it is difficult to talk about exercise therapy or kinesiotherapy in the broad sense. In such circumstances, the patient reports severe pain and limited spine mobility, which prevents them from working or performing basic everyday activities. Due to the fact that myofascial pain syndrome (MPS) is frequently diagnosed, one of the newer minimally invasive therapy alternatives that can interrupt this pathological process is the use of a microinjection technique, a peri-spinal therapy called local intradermal therapy, or more commonly, spinal mesotherapy. This method can be used with drugs to relieve pain and inflammation (e.g. ketoprofen), anesthetics (e.g. lignocaine, bupivacaine), myorelaxants (e.g. diazepam), and regenerative drugs (e.g. tropocollagen I) [10, 11]. Due to its safety and low risk of complications, this therapy is used more and more often as one of the treatment stages with the aim, among others, of interrupting the process of chronic disease exacerbation, reducing pain, improving mobility and creating conditions for the effective use of the third stage – rehabilitation.
Surgical treatment
In some patients, despite the implementation of conservative treatment, spinal surgical treatment should be considered, which is used primarily in the case of neurological symptoms, such as paresis or sphincter disorders. Obviously it is targeted at its cause. Unfortunately, very often the surgical treatment is delayed for various reasons. Then, the pathological lesion progresses, the patient gets older, and new diseases develop with age. All this may have a significant impact on the final effect of surgical treatment.
Unfortunately, some patients still report pain despite spinal surgery. In such cases failed back surgery syndrome is diagnosed [12]. Failed back surgery syndrome is a generalized medical term that is often used to describe the condition where back pain persists or appears after spine surgery. Important risk factors include instability after surgery, tissue scarring after surgery, and the patient’s predispositions [12, 13].
However, a very important aspect is a thorough assessment of whether the symptoms originate from the spine or whether they are caused by paraspinal pathologies, such as greater trochanteric pain syndrome, which require different treatment [14]. In consequence, it turns out that the patient, apart from SD, may also suffer from other disorders of organs of the musculoskeletal system, which, e.g., develop as a result of SD or constitute their complications.
Stage 3
Rehabilitation
Spinal rehabilitation plays an essential role in treatment of musculoskeletal disorders. Eagerly used are movement therapy and kinesiotherapy, both allowing one, among other benefits, to relax tense tissues, stretch them and, as a result, strengthen the entire musculoskeletal system. This has a significant impact on the stabilization of the spinal motor unit [15, 16]. Additionally, physical therapy is used, having local anti-inflammatory, anti-swelling and analgesic effects, improving circulation and, consequently, promoting regeneration of pathologically changed tissues [15–17]. Many studies have reported the effectiveness and safety of various therapies. However, attention is not always paid to the time needed to implement a specific physiotherapeutic procedure for a specific spine pathology. Therefore, for this purpose, various studies are carried out to determine at what stage, after medical therapy, to implement the specialized rehabilitation: whether to use it simultaneously or immediately after the second stage – medical therapy – or sometimes after the discontinuation of medical therapy. This is important for the effective maintenance of previously administered medical therapy [18].
Soon after introducing conservative therapy (pharmacotherapy) as well as after surgical therapy the use of exercise therapy is recommended after a short time but under some conditions especially after surgical procedures.
However, starting exercise therapy too quickly in patients after spinal surgery may lead to health deterioration and expose the patient to complications requiring reoperations. This applies to both less and more invasive surgical techniques. After the endoscopic removal of an intervertebral disc herniation, i.e. a minimally invasive surgical technique that should cause little tissue trauma, the healing period of the annulus fibrosus is consistent with the biological process of soft tissue healing, i.e. a standard period of 6 weeks. Spinal rehabilitation introduced too soon may lead to the development of recurrent hernia [19].
The same applies to patients with spinal stenosis after extensive open spine surgery with spinal canal decompression and posterior lumbar interbody fusion, i.e. screw implantation. Typically, rehabilitation aimed at the spine is not implemented earlier than after 2–3 months due to the risk of implant loosening and exposing the patient to another surgical procedure [20, 21]. In some patients, the rehabilitation process can be started earlier; therefore the treatment in this matter should be individualized. Table IV shows the implementation time of targeted rehabilitation for the operated basic pathology for selected spine surgery methods.
Table IV
Therefore, each spinal pathology has its own different treatment regimen. Early postoperative physiotherapeutic treatment is justified, but it should first concern other issues, e.g. anticoagulation, breathing improvement, learning and controlling walking with the use of orthopedic equipment. Attention should also be paid to the patient’s education, especially regarding spinal load reduction in everyday life.
Discussion
The issues related to SD treatment constitute an enormous discipline. This is not only a health problem, but also a social one. In addition, other specialists play an important role. A psychologist or psychiatrist is often necessary in comprehensive management. Sometimes a social worker needs to be involved. Therefore, the treatment of spine pathology is multidirectional [24]. Many articles published in the world of medicine present the issue of risk factors for back pain syndrome separately. Medical and physiotherapeutic procedures are often discussed separately. However, papers promoting a disciplinary approach to the treatment of musculoskeletal system pathologies, including the spine, are increasingly published [25, 26].
Additionally, it is worth paying attention to a paper by the UEMS-PRM Section Professional Practice Committee, which describes the role of physical and rehabilitation medicine physicians in the management of spinal pain, focusing particularly on low back pain and neck pain [27].
Therefore, the aim of this paper is to address the issue of comprehensive treatment of spine pathologies, focusing on a three-stage treatment concept, especially taking into account the aspect of risk factors. Their reduction is often impossible for various reasons. A doctor’s recommendation of changing job is not always possible to implement due to various factors, including economics or the patient’s education. Very often, our patients work many hours in front of a computer in a sitting position. The probability that they will give up their profession is faint. Therefore, it is worth considering the modification of risk factors discussed above. Multidirectional treatment provides a chance for effective therapy.
Timely implemented targeted rehabilitation maintains its effectiveness. Based on the available literature, it is difficult to find papers taking into account the so-called three-step concept for treatment of spine pathologies. Moreover, the term “three-step concept” has not been used in medical nomenclature until now. This paper also aims to take a different look at the treatment of musculoskeletal pathologies, involving not only medical staff – doctors, physiotherapists or psychologists – but especially the patients themselves, who will make certain modifications in their everyday activities, including professional work.
Conclusions
Based on theoretical considerations, implementing a three-stage approach in the treatment of non-inflammatory SD, especially arising as a result of spine overload or degenerative processes of the spine (e.g. osteoarthritis), can significantly improve the effectiveness of the therapies used. Rehabilitation should be viewed as continuing the management of the healing process.