Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease with symptoms similar to depression. The presence of symptoms such as generalized pain, fatigue and sleep disturbance in RA patients mimics depression [1]. In addition to depression, the state of anxiety is also prevalent in RA. Almost 30% of RA patients develop depression within 5 years of diagnosis [2] and about 20% of these patients may experience anxiety [3]. The presence of depression and anxiety contributes to disease severity and poor outcomes, because these conditions are often under-recognized due to similarities between manifestations of depression and anxiety with RA [1].
A recent systematic review and meta-analysis revealed depression in 17% of RA patients [4] and another meta-analysis of 10 cohort studies including 6,201 cases of anxiety and 139,875 participants [5] demonstrated significantly higher risk of anxiety in RA patients than individuals without RA, with OR = 1.20 (95% CI: 1.03–1.39).
In another study of RA patients, the prevalence of patient-reported anxiety or depression was 38.4%, whereas their physician found depression or anxiety in 17.7% of patients. In this study patients with anxiety or depression had significantly higher treatment dissatisfaction and impairment in work and usual activity [6].
Several factors such as chronicity, progressive characteristics of RA, lack of a definite treatment, and a possibility of future development of disability can explain higher prevalence of depression and anxiety in RA. Furthermore, systemic inflammation in itself is related to depression, because pro-inflammatory cytokines such as tumor necrosisfactor α (TNF-α), interleukin-6 (IL-6), and IL-1β are in contact with areas of the central brain, which are known to have altered brain function in depression [7]. Moreover, recent data indicate that inflammation is a feature of depression, and even in the absence of an autoimmune disease, high levels of pro-inflammatory cytokines can be detected.
The results of a meta-analysis revealed reduction of IL-4, IL-6, and IL-10 concentrations in depressive patients and treatment with selective serotonin reuptake inhibitors resulted in reduction of IL-1 level [8].
The association between RA and depression is bidirectional. This suggests higher susceptibility of RA patients to depression and similarly a greater risk of RA development in depressed individuals. The results of a longitudinal study indicated 1.69 times greater incidence of depression in RA patients, and 1.65 times greater incidence of RA development in depressed patients [9].
In another study, the risk of developing RA in depressed patients taking antidepressant drugs was 24% lower than in those who did not use antidepressants, suggesting depression as a risk factor for RA [9].
Stressful events and mental disorders can increase the risk of RA, and the association of these conditions with inflammatory arthropathy, psoriatic arthritis, as well as other autoimmune diseases such as inflammatory bowel disease and alopecia areata, has been observed [7].
Identification of depression and anxiety states in patients with RA is important as the presence of these conditions affects the efficacy of treatment and disease outcomes, because among RA patients with depression, non-adherence to the treatment and suboptimal taking of medications are frequent. This issue was illustrated in a systematic review of 12 studies in relation to depression and 13 studies related to anxiety. In this study non-compliance was 3 times higher in depressed patients than in non-depressed individuals [10].
Depression and RA seem to be interrelated and both conditions are associated with inflammation. The influence of depression and inflammation on pain perception has been reported in RA [11]. This issue has been addressed in many studies. Most studies have found an association between depression and more severe RA and poor outcome [12]. Furthermore, symptoms of depression/anxiety are associated with subjective features of disease activity and can reduce the likelihood of RA remission and consequently influence the treatment decision.
However, the prevalence of depression/anxiety in patients with RA and their association with severity of RA varies across different studies. This may be attributed to the characteristics of the study population, criteria applied for the diagnosis as well as severity of depression or anxiety, application of measures for assessment of RA activity, and distribution of the associated factors of depression or anxiety in the general population. In addition, depression and anxiety share similar symptoms with RA and thus coexistence of these conditions in RA patients is often not diagnosed or under-recognized.
The present study was designed to determine the prevalence of depression/anxiety in patients with RA to examine the correlation between depression/anxiety and RA activity.
Material and methods
The population of this study was selected consecutively among RA patients who presented at a rheumatology clinic for follow-up examination between March and September 2018. The diagnosis of RA was confirmed by the 2010 ACR/EULAR criteria [13] and the diagnosis of depression and anxiety was made by the Hospital Anxiety and Depression Scale (HADS) [14]. The reliability and validity of this measure, which was designed to diagnose both anxiety and depression in populations, were confirmed in Iranian patients [15].
All eligible patients were included in the study and subjects taking treatment for depression/anxiety, with a history of psychological diseases, patients with coexistent chronic conditions such as chronic low back pain, chronic non-RA musculoskeletal diseases, cardiovascular disease, cerebrovascular diseases, gastrointestinal, renal and hematological diseases were excluded. Sample size was estimated to detect a correlation between HADS and Disease Activity Score based on the 28-joint count (DAS28) by r = 0.2 [15]. A sample size of at least 194 patients was needed to detect such a correlation with a confidence interval of 95% and power of 80%.
All patients underwent complete clinical and laboratory evaluations. The RA activity was assessed by calculation of the DAS28, and a DAS28 score > 2.6 points was considered as active RA and patients with a DAS28 score less than 2.6 points were considered to be in remission.
In statistical analysis the association between RA activity and depression/anxiety state was determined by the Pearson correlation test. Subgroup analyses were also performed to determine the influence of age, sex and disease duration on the correlation between depression/anxiety and RA activity. Student’s t-test and the χ2 test were applied to compare quantitative and categorical variables respectively. Multiple regression analysis with calculation of adjusted odds ratio (OR) and 95% confidence interval (95% CI) was used to determine independent associations. SPSS software version 21 was used for analysis.
The proposal of this study was confirmed by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran (Code ethics no. IR.MUBABOL.REC.1399.499).
Results
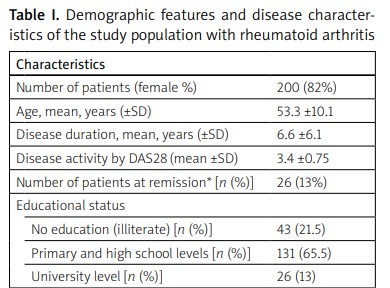
A total of 200 patients (female, 82%) with mean age of 53.5 ±10.1 years and mean disease duration of 6.6 ±6.8 years were studied. In 29 patients (14.5%) RA was in a state of remission and in the rest of the patients RA was active. Disease characteristics and demographic features of the study population are shown in Table I.
Table I
Demographic features and disease characteristics of the study population with rheumatoid arthritis
| Characteristics | |
|---|---|
| Number of patients (female %) | 200 (82%) |
| Age, mean, years (±SD) | 53.3 ±10.1 |
| Disease duration, mean, years (±SD) | 6.6 ±6.1 |
| Disease activity by DAS28 (mean ±SD) | 3.4 ±0.75 |
| Number of patients at remission* [n (%)] | 26 (13%) |
| Educational status | |
| No education (illiterate) [n (%)] | 43 (21.5) |
| Primary and high school levels [n (%)] | 131 (65.5) |
| University level [n (%)] | 26 (13) |
| Psychiatric disorders | |
| Patients with depression [n (%)] | 27 (13.5) |
| Patients with anxiety [n (%)] | 38 (19) |
Overall, depression was detected in 27 (13.5%) patients and anxiety in 38 (19%) patients. Mean depression and anxiety scores in RA patients in remission were significantly lower than in active disease (data not shown). There was a positive and weak but significant correlation between depression score and DAS28 score (r = 0.173, p = 0.014); similarly there was a weak and positive correlation between anxiety score and DAS28 (r = 0.229, p = 0.001). The impact of age, sex, and disease duration on the correlation between depression/anxiety and RA activity is shown in Table II.
Table II
Factors influencing correlation coefficient* between depression/anxiety and disease activity in patients with rheumatoid arthritis**
In subgroup analysis, the positive correlation between depression and RA activity remained at a significant level only in women but not in men. However, the correlation between anxiety and RA activity remained at a significant level in both sexes, especially in men (Table II).
The association was significantly influenced by age and duration of RA. The activity of RA was strongly correlated with anxiety in men aged ≤ 40 years, as well as with depression in both women and men who had disease duration ≤ 1 year (Table II). In multiple logistic regression analysis after adjustment for all covariates such as sex, age, disease duration, and level of education, female sex and age ≤ 40 years were independently and significantly associated with RA activity in patients with depression, with adjusted OR = 4.21 (1.67–10.61, p = 0.002), and adjusted OR = 3.56 (95% CI: 1.14–11.11, p = 0.028), respectively (data not shown).
Discussion
The results of this study indicated that 13.5% of RA patients had depression and 19% had anxiety. There was a weak but a significant positive correlation between depression/anxiety and RA activity and the correlation was stronger during the first year of the disease onset. However, after adjustment for other covariates, only female gender and age ≤ 40 years were independent predictors of disease activity only in RA patients with depression. These findings are in agreement with earlier studies and provide additional data on the subject of depression and RA activity.
In a similar cross-sectional study of 414 RA patients presented by Tehran Rheumatology Research Center, 63.6% and 84.1% of the study patients had depression and anxiety respectively. In this study coexistence of anxiety and depression was detected in 60.2%. High prevalence of depression/anxiety in this study can be attributed to severity of RA, because the patients of this study presented at a research center that provides tertiary health care for patients referred with advanced RA [16]. Overall, the prevalence of depression in RA varies from 15.29% to 42.9% across various studies [16–18].
A systematic review and meta-analysis of 44 studies found that the overall prevalence of major depressive disorder was 4.1% in the Iranian population. Women were 1.95 (95% CI: 3.1–5.1) times more likely to have depression [19]. Therefore, depression in RA is more prevalent as compared to the general population, and in particular the prevalence is likely higher in RA patients who need hospital services.
In a cross-sectional study of 189 Malaysian RA patients, psychological symptoms were significantly correlated with RA activity, tender joint count (TJC), general health, pain and health assessment questionnaire (HAQ) scores. In this study there was a positive correlation between higher number of swollen joints (SJC) and depression, but not with anxiety and stress and HAQ was a predictor of stress and an independent predictor of depression and pain [18].
Another study, of Egyptian RA patients, found a positive correlation between depression and HAQ, pain assessed by visual analogue scale (VAS), DAS28 and CRP but not with ESR, SJC and TJC [17]. A similar correlation between depression and CRP and pain was observed in another study of 218 RA patients, suggesting an association between depression and inflammation [11].
At present the decision on the initiation and continuation of treatment in RA is based on calculation of the DAS28 score, which contains both objective and subjective components.
Matcham et al. [20] found an association between depression/anxiety state with objective components of RA (patients global assessment – PGA and TJC), but not with more objective components of DAS28 (ESR and SJC). In this one year-follow-up longitudinal study of 58 RA patients, baseline depression was significantly associated with TJC and GPA at 1-year follow-up even after adjustment for other clinical covariates. These findings indicate a contribution of depressive/anxiety symptoms in calculation of RA activity by DAS28 [20].
In another study of patients with early RA by Boer et al. [21], depression/anxiety at baseline was detected in 20% of patients according to the SF-36MCS ≤ 38, and in 23% of patients according to the SF-36MH ≤ 56. The presence of depression/anxiety was negatively correlated with DAS28 remission after one year. The findings indicated that baseline association of depression/anxiety state with the subjective components of DAS28 will reduce RA remission as measured by DAS28. This highlights that improving psychological factors at an early stage of RA may reduce DAS scores at later stages and thus may prevent application of intensified treatment strategies and medical costs [21].
An association between baseline depression/anxiety with subjective components of DAS28 was also found in the NOR-DMARD study that included 1,326 patients with RA and 728 patients with psoriatic arthritis (PsA) [22].
These observations can also explain the high DAS28 score and persistence of joint pain in RA patients with apparently normal clinical findings and a low level of acute phase proteins. The high DAS28 value may be partly due to depressive symptoms which are strongly associated with subjective markers of DAS28.
A meta-analysis of 25 trials demonstrated that psychological interventions provide important adjunctive therapies in the medical management of RA [23]. A systematic review and meta-analysis of 6 randomized controlled trials that included 2,540 patients with RA, PsA and ankylosing spondylitis revealed a small but significant effect of anti-TNF therapy on depression/anxiety in chronic diseases, and thus suggested involvement of inflammation in the depressive syndrome [24]. Again, treatment of RA with disease-modifying antirheumatic drugs (DMARDs) may benefit depressive symptoms. This was shown in a study of RA, in which administration of sulfasalazine and tocilizumab reduced depressive symptoms by 30% [25].
Although the physical manifestations of depression are not similar to anxiety, some people experience depression, anxiety and RA all at the same time. Depressive disorder is thought to be an independent risk factor for both work disability and mortality in RA, and may involve 13% to 17% of these patients [12]. An association between persistence of depression and RA activity as well as RA flare has been found [26, 27].
In some patients with persistent musculoskeletal pain such as RA, OA, or fibromyalgia, the association of pain with disease severity as determined by objective indices such as radiography or serology is marginal, whereas the association of pain with emotional and psychological factors is high. This suggests an important contribution of psychological factors in pain perception. Depression and catastrophizing are always associated with severity of pain, sensitivity to pain, physical disability, poor outcomes, early mortality and activity of the inflammatory disease. Both conditions can increase the level of pain perception by patients. Therefore, in rheumatological diseases, these two conditions should also be therapeutic targets [28].
There is a biologic link between substrates responsible for inflammatory conditions and mood disorders. Proinflammatory cytokines have a direct effect on the serotonergic system, which contributes to the pathophysiology of mood. Again, serotoninergic pathways are thought to mediate both inflammation and mood [12]. A complete response with sustained remission has been reported after treatment of depression in a case of RA with coexistent depression. This patient was unresponsive to standard treatment of RA by using multiple DMARDs, but treatment of depression with a specific serotonin reuptake inhibitor resulted in complete remission of arthritis symptoms and sustained remission [29].
A meta-analysis of seven randomized controlled trials involving 2,370 participants showed a significant anti-depressant effect of anti-cytokine treatment compared with placebo. All anti-TNF drugs such as adalimumab, etanercept, infliximab and tocilizumab result in a significant improvement of depressive symptoms, suggesting a possible causal role of cytokines in the development of depression. These findings indicate that in chronic depression with inflammation, cytokine modulators may provide therapeutic benefits [30] supporting the concept of a link between the inflammatory process and both RA and depression and emphasizing the need for more focus in identification of depression in RA patients and simultaneous treatment of both conditions.
Study limitations
This study has several limitations. The study design is cross-sectional and thus the results do not indicate causality. The diagnosis of depression and anxiety was made at the time of patient selection; therefore, the correlation between RA activity and depression/anxiety cannot be extrapolated to the whole course of RA. In patients with RA, factors other than RA, such as coexistent medical conditions, drug complications, and economical problems may also contribute to the development of depression/anxiety. However, distribution of these factors in patients with and without depression/anxiety is expected to be similar, and so the results are less confounded.
Conclusions
The results of this study indicate a high prevalence of depression/anxiety in RA and a positive correlation of these conditions with disease activity, particularly in women and in patients aged 40 years and less. Regarding the important contribution of psychological factors, in particular depression, in perception of pain, identification of individuals with depression and its appropriate treatment are expected to reduce RA activity. This issue needs further studies.