Introduction
Nailfold capillaroscopy is a non-invasive method for visualising the nailfold capillaries under a stereomicroscope or videocapillaroscope. The examination is used for differential diagnosis of Raynaud`s phenomenon and microcirculation disorders in secondary Raynaud’s phenomenon associated with systemic connective tissue diseases [1].
Capillaroscopy is particularly important for early diagnosis of systemic sclerosis (SSc) for assessing the disease activity and the extent of internal organ involvement as well as for monitoring and evaluating the effectiveness of the therapy applied. In SSc, the capillaroscopic examination shows characteristic microcirculation disturbance called microangiopathy typical of SSc “scleroderma pattern”. The term microangiopathy includes the following pathological changes: dilated capillary loops leading to formation of megacapillaries, decreased numbers of vessels, the areas of avascularisation, and the presence of ramified loops and microhaemorrhages [2].
Nailfold capillaroscopy in scleroderma-spectrum disorders
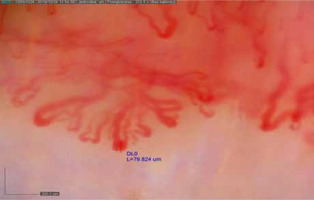
Nailfold capillaroscopy is useful not only for the diagnosis of SSc but also for the diagnosis and monitoring of scleroderma-spectrum diseases, including dermatomyositis (DM), polymyositis (PM), mixed connective tissue disease (MCTD) and undifferentiated connective tissue disease (UCTD) [3]. According to Cutolo et al. [2], the capillaroscopic abnormalities characteristic of SSc occurring in other “scleroderma-spectrum” diseases should be defined as “scleroderma-like pattern” microangiopathy, which affects about 20–40% of patients with idiopathic inflammatory myopathies, more often in DM than in PM. The predominant capillaroscopic changes in DM include increased neoangiogenesis (bushy, dendriform vessels) and moderate derangement of the vascular architecture with a relatively low number of avascular areas. Another characteristic feature is the presence of giant ramified vessels (Fig. 1).
In many cases, the lesions found in different fingers of one patient vary [4]. Considering significant differences in capillaroscopic pictures in SSc patients, as compared to DM patients, some authors suggest that in DM the term microangiopathy in the course of DM should be used instead of scleroderma-like microangiopathy [5].
There are many literature reports evaluating the relation between capillaroscopic microcirculation abnormalities vs. disease activity, extent of internal organ involvement and severity of skin lesions in inflammatory myopathies [6, 7]. Muggi et al. [6] found a significant correlation between capillaroscopic changes and DM activity. According to their findings, the concentrations of creatinine kinase in patients with scleroderma-like microangiopathies were higher than in patients without microangiopathies. Moreover, during the 9-month observation, capillaroscopic findings were found to improve (reduced numbers of megacapillaries and microhaemorrhages, increased density of capillaries), which correlated with the clinical stability. The authors suggest that microcirculation improvement might result from the immunosuppressive therapy applied in the group studied, which speaks in favour of the dynamics of capillaroscopic changes affected by the therapy.
Furthermore, Barth et al. [7] observed a correlation between the number of vessels and lung involvement in patients with juvenile DM. Lower percentages of increased vital capacity, total lung capacity and CO2 diffusion capacity were observed in the group of patients with reduced density of capillaries, as compared to patients with normal numbers of vessels [7]. Thus, evaluation of capillary density is an important tool for monitoring inflammatory myopathies, particularly juvenile DM, and a rapid loss of capillaries is associated with increased severity of the disease.
In 2017, the consensus-based recommendations for monitoring patients with juvenile DM and for evaluating the disease activity as well as therapy responses were prepared. The recommended examinations included nailfold capillaroscopy [8].
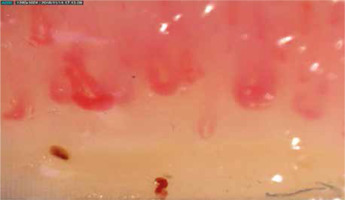
Scleroderma-like microangiopathy capillaroscopic abnormalities were also observed in about 50–60% of patients with MCTD (Fig. 2). Some articles have reported a correlation between scleroderma-like microangiopathy vs. interstitial lung disease and pulmonary arterial hypertension in patients with MCTD; moreover, reduced density of capillaries has been found to correlate with more severe course of the disease [9].
In cases of UCTD, most patients have normal capillaroscopic pictures. About 40–50% of patients demonstrate nonspecific changes in the form of tortuous, crossed and dilated loops, which however do not meet the criteria of megacapillaries, with mild disorientation of vascular architecture. About 10% of patients fulfil the criteria of scleroderma-like microangiopathy, and this group requires systematic monitoring and observation for a given systemic connective tissue disease, especially SSc.
In a study whose findings were presented during this year’s conference of the European League Against Rheumatism, Pizzorni et al. [10] analysed retrospectively the capillaroscopic pictures in a group of patients with MCTD, UCTD and primary Raynaud phenomenon. Scleroderma-like microangiopathy capillaroscopic changes were observed statistically significantly more often in patients with MCTD, as compared to UCTD. Furthermore, neoangiogenesis, giant capillaries and a reduction of capillaries were more pronounced in MCTD than in UCTD. The authors concluded that capillaroscopic changes in the course of UCTD resemble the picture found in primary Raynaud phenomenon (non-specific changes), as opposed to MCTD, in which scleroderma-like microangiopathic changes and reduced numbers of capillaries predominate [10].
Conclusions
Nailfold capillaroscopy is used not only for the diagnosis and evaluation of SSc activity but also for evaluation of scleroderma spectrum diseases, especially inflammatory myopathies. Long-term evaluation of capillaroscopic abnormalities may be significant for making therapeutic decisions, changes in treatment and monitoring patients with scleroderma spectrum diseases.