Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by the presence of erosive synovitis resulting in progressive joint damage, impaired function, and increased morbidity and mortality. Considerable progress in early diagnosis and therapeutic strategy for RA has been made in the last few decades. The persistent remission target has become achievable through advances in disease-modifying anti-rheumatic drugs (DMARDs) (the targeted synthetics – tsDMARDs, and biologics – bDMARDs), the tight-control and treat to target strategy [1, 2].
Clinical remission is evaluated by composite indices disease activity score (DAS28), simple disease activity index (SDAI), clinical disease activity index (CDAI), or the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) Boolean criteria, which combine clinical and laboratory assessment [3].
Nevertheless, despite apparent clinical remission, relapse is reported in 30–50% of patients in the first 2 years of remission [4] and joint damage progresses in 10–30% [5]. These data suggest that composite indices may not reflect the real RA activity.
Ultrasound (US) in RA showed greater sensitivity than the clinical assessment to detect synovitis and tenosynovitis (TS) in B-mode and power Doppler (PD). Indeed, B-mode synovial hypertrophy (SH) was found in 33.3 to 100% of patients and PD signal was objectified in 14.9–93.3% of patients in clinical remission [5].
Furthermore, US synovitis with PD predicted relapse, radiographic progression, and unsuccessful treatment tapering [6, 7]. Several definitions were used for US remission, but none is consensual [8].
We aim through this article to assess US remission in patients with RA in clinical remission using different definitions.
Material and methods
Rheumatoid arthritis patients according to 2010 ACR/EULAR criteria [9] were recruited, consecutively, between January and December 2019 from the outpatient consultations or the day hospital of the Rheumatology Department. The patients were on conventional synthetic DMARDs (csDMARDs) or bDMARDs.
They were included if they met the following criteria:
RA diagnosed and patient was taken DMARD for more than 6 months,
age greater than 18 years,
clinical remission according to the DAS28 ≤ 2.6 (using erythrocyte sedimentation rate – ESR) for at least 6 months and at the day of US examination,
absence of flares in the last 6 months,
same treatment for 6 months including the DMARDs, corticosteroids, and intraarticular injections.
The study was performed in accordance with the ethical standards of the responsible committee on human experimentation and with the Declaration of Helsinki. Informed consent was obtained from all patients before study enrolment.
Clinical and laboratory assessment
We recorded the patient demographics and RA characteristics as the presence of rheumatoid factor, anti-citrullinated peptide antibodies, and radiographic damage in hands and feet (using the modified Sharp score) [10].
On the day of US examination the patients were re-evaluated for disease activity. Tender joint counts (TJC), swollen joint counts (SJC), and patients’ global assessment of disease activity and pain were rated on a numerical scale. Inflammatory markers, including C-reactive protein (CRP) and ESR, were performed during the week of evaluation. The investigator was blinded to the US findings.
Clinical remission criteria
As well as the DAS28, clinical remission was assessed according to the CDAI, the SDAI, and the ACR/EULAR Boolean criteria (TJC ≤ 1, SJC ≤ 1, CRP ≤ 10 mg/dl and patient global assessment ≤ 1) [3].
Ultrasound assessment
A longitudinal and transverse examination of 42 joints and 20 tendon compartments was made for each patient on B-mode and PD using a My Lab ESAOTE US machine with a 6–18 MHz linear transducer. The operator was a rheumatologist experienced in musculoskeletal US and blind to data. The ultrasound assessments lasted 30–60 min.
The presence of SH in B-mode and PD signal were examined in the following bilateral joints: glenohumeral (biceps sheath, posterior recess), elbow (radio-humeral and humero-ulnar joints), wrist (radiocarpal and distal radioulnar joints), dorsal side of the second to the fifth metacarpophalangeal (MCP), dorsal side of the second to fifth proximal interphalangeal of the hands, knees (anterior and parapatellar recesses), tibiotalar joint of the ankle, and dorsal side of second through fifth metatarsophalangeal joints.
The synovial hypertrophy or PD signal was attributed to the wrist when present in the radiocarpal or distal radioulnar joints. Similarly for the elbow if SH or synovial PD signal were identified in either the radio-humeral or humero-ulnar joints.
Tenosynovitis on B-mode and PD was assessed in hands, wrists, and ankles as follows: first through sixth extensor tendon compartments of the wrists, and second through fifth finger flexor digitorum superficialis and profundus tendons, tibialis posterior, and peroneal tendons.
For each joint, B-mode SH and PD signal was defined and scored separately, semiquantitively according to the outcome measures in rheumatology clinical trials (OMERACT) on a scale of 0–3 (grade 0 = none, grade 1 = minimal, grade 2 = moderate, grade 3 = severe) [11].
The final score at each joint represented the maximal score for the SH and PD signal, respectively, obtained from any one of the joint recesses or from any joint evaluated in the elbow or the wrist.
Tenosynovitis on B-mode and PD signal was defined and scored separately, semiquantitively according to the OMERACT on a scale of 0–3 (grade 0 = none, grade 1 = minimal, grade 2 = moderate, grade 3 = severe) [12].
Definition of ultrasound remission
Several definitions of US remission were examined: the strictest were defined as the absence of SH, TS, and PD signal (B-mode = 0 and PD = 0) and as the absence of SH and PD signal (SH = 0 and PD = 0). Less strict criteria were used (SH ≤ 1 and PD = 0 or SH ≤ 1 and PD ≤ 1). Others were based solely on synovial PD (absent [PD = 0] or low level [PD ≤ 1]).
Results
Demographic and clinical characteristics
Thirty-seven patients were enrolled in the study. The demographic and clinical features are presented in Table I. The mean age was 54.2 years, and 73% were females. The mean disease duration was 8.1 years, and the mean remission duration was 36.5 months. The rate of remission according to the different composite indices was 70.2% for the SDAI, 64.8% for the CDAI, and 54% for the ACR/EULAR Boolean criteria.
Table I
Characteristics of patients with rheumatoid arthritis in clinical remission
[i] ACPA – anti-citrullinated peptide antibodies, ACR/EULAR – American College of Rheumatology/European League Against Rheumatism, bDMARD – biologic disease-modifying anti-rheumatic drugs, CDAI – clinical disease activity index, CRP – C-reactive protein, DAS28 – disease activity score, ESR – erythrocyte sedimentation, RF – rheumatoid factor, SD – standard deviation, SDAI – simple disease activity index. ACR/EULAR Boolean remission criteria – tender and swollen joint counts ≤ 1, CRP ≤ 10 mg/dl and patient global assessment ≤ 1.
Ultrasound synovitis and tenosynovitis
Synovial hypertrophy was detected in 94.6% of patients. The grades of SH were as follows: 1 in 89.1%, 2 in 64.8%, and 3 in 16.2% of patients. The wrist, MTP2, MCP3, MCP2, and knee (78.3, 45.9, 43.2, 40.5, and 37.8%, respectively) were predominantly involved.
Power Doppler signal was objectified in 59.5% of patients. The grades of PD were: 1 in 37.8%, 2 in 35.1%, and 3 in 5.4% of patients. The wrist, MCP2, MCP3, and MTP2 joints (40.5, 18.9, 10.8, and 8.5%, respectively) were frequently involved.
On B-mode, TS was detected in 40.5% of patients. It was most commonly grade 1 in 32.4%, 2 in 10.8%, and 3 in 2.7% of patients. B-mode TS was observed in the extensor carpi ulnaris, tibialis posterior, peroneal, flexor digitorum, and extensor digitorum carpi (21.6, 10, 8.1, 5.4, and 2.7%, respectively).
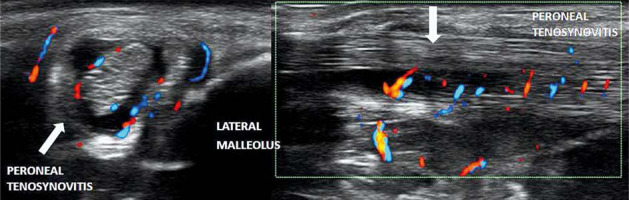
Tenosynovitis with PD was evident in 13.5% of patients. Grade 2 (10.8%) was more common than grade 1 (5.4%). It affected predominantly the extensor carpi ulnaris in 8.1% and in 2.7% the tibialis posterior, peroneal (Fig. 1), and extensor digitorum carpi.
Ultrasound remission
Among our patients, US remission was rare in 5.4% (n = 2) of patients when the strict criteria were used at the joint and tendon level. Ultrasound remission was recorded in 32.4% of patients if the grade of SH and PD was ≤ 1 at the joint level, in 40.5% of patients in the absence of PD, and in 62.2% of patients if the PD grade was ≤ 1 at the joint level. At the tendons level, US remission varied from 51.4 to 85% of patients.
For the other clinical remission criteria, US remission at joints and tendons was found in 7.7–60% of patients. Globally, the percentage of US remission varied according to the clinical and US remission criteria, as illustrated in Table II.
Table II
Ultrasound remission in clinical remission according to disease activity score, clinical disease activity index, simple disease activity index, and American College of Rheumatology/European League Against Rheumatism Boolean criteria in rheumatoid arthritis
[i] ACR/EULAR – American College of Rheumatology/European League Against Rheumatism, CDAI – clinical disease activity index, DAS28 – disease activity score, ESR – erythrocyte sedimentation rate, PD – power Doppler, SDAI – simple disease activity index. ACR/EULAR Boolean remission criteria – tender and swollen joint counts ≤ 1, CRP ≤ 10 mg/dl and patient global assessment ≤ 1, B-mode + PD = 0 – the absence of signal on B-mode and PD, B-mode ≤ 1 and PD = 0 – a grade ≤ 1 on B-mode and a PD = 0, B-mode ≤ 1 and PD ≤ 1 – a grade ≤ 1 on B-mode and PD, PD = 0 – the absence of PD, PD ≤ 1 – a grade ≤ 1 of PD.
Discussion
This study investigated US remission in many joints and tendons using different definitions of clinical and US remission. We have shown that a significant number of RA patients in clinical remission had synovitis (94.6%) and TS (40.5%) in B-mode with PD signal (59.5 and 13.5%, respectively). Ultrasound remission at joints and tendons was confirmed in 5.4–62.2% of patients. In addition to DAS28–ESR, all the other remission criteria showed US inflammatory activity. According to the literature and our study, clinical remission, even classified by strict composite indices, does not seem to reflect the “true” remission.
Indeed, SH was detected in 20–100% of patients, and 12.8–93.3% had at least one synovitis with PD, in the literature [5, 13–16]. B-mode TS was found in 9.6–52.3% of patients and PD mode in 2.1–26% of patients [15, 17–20]. In sustained remission, TS with PD was absent in 2 studies, suggesting its importance in US evaluation during remission [21, 22]. Filippou et al. [20] showed that 80.9% of patients with RA in remission had at least one synovitis or TS in B-mode, with PD in 51% of patients.
Moreover, SH and PD were predictive of flare in patients with clinical remission [6]. Progressive bone erosion was associated mainly with PD and severe grades of SH as demonstrated by some studies [23]. Likewise, TS with PD predicts the risk of flare, unstable remission [18, 21], and radiographic damage progression [24]. However, US remission is still not consensual throughout the different definitions available (Table III).
Table III
Ultrasound remission in included studies
| Author, year | Number of patients RA | Clinical definitions of remission | Ultrasound definitions of remission (%) | |||||
|---|---|---|---|---|---|---|---|---|
| SH + PD = 0 | SH ≤ 1 and PD = 0 | SH ≤ 1 and PD ≤ 1 | PD = 0 | PD ≤ 1 | SH + tenosynovitis on B-mode and PD = 0 | |||
| Saleem et al., 2011 [25] | 128 | DAS28 < 2.6 ≥ 6 months | 17 | – | 56 | 49 | 78 | – |
| Balsa et al., 2010 [26] | 97 | Clinician | – | – | – | 57.7 | – | – |
| Cruces et al., 2019 [29] | 58 | DAS28 < 2.6 ≥ 6 months | 25.9 | – | – | – | – | – |
| Peluso et al., 2011 [30] | 94 Early RA: 48 Longstanding RA: 46 | DAS < 1.6 ≥ 6 months | 30.8 Early RA: 43.7 Longstanding RA: 17.4 | – | – | – | – | – |
| Chung et al., 2020 [31] | 97 | DAS28 < 2.6 | 51.1 | – | – | – | – | – |
| Saleem et al., 2009 [32] | 100 | DAS28 < 2.6 ≥ 6 months | TNFi + MTX: 10 DMARDs: 16 | – | – | – | – | – |
| Horton et al., 2016 [33] | 45 | DAS28–CRP < 2.6 | – | – | – | 42 | 62 | – |
| Harman et al., 2015 [34] | 64 | ACR/EULAR Boolean ≥ 6 months | – | – | – | – | – | bDMARD: 49.6 csDMARD: 43.9 |
| Spinella et al., 2012 [35] | 54 | ACR criteria or DAS28 < 2.6 ≥ 6 months | 35 | – | – | – | – | – |
| Terslev et al., 2021 [36] | 87 | DAS28–CRP < 2.6 ≥ 1 year and no radiographic progression | 7 bDMARD: 14 csDMARD: 0 | 37 40 33 | – | 56 55 58 | – | – |
| Van der Ven et al., 2017 [37] | 89 | DAS44 ≤ 2.4 et NAG ≤ 1 | – | Visit 1: 39 Visit 2: 32 | – | – | – | – |
| Our study | 37 | DAS28 < 2.6 ≥ 6 months | 5.4 | 32.4 | 32.4 | 40.5 | 62.2 | 5.4 |
[i] ACR/EULAR – American College of Rheumatology/European League Against Rheumatism, CRP – C-reactive protein, DAS28 – disease activity score, DMARD – disease-modifying anti-rheumatic drugs, bDMARD – biologics, csDMARD – conventional treatment, MTX – methotrexate, PD – power Doppler, RA – rheumatoid arthritis, SH – synovial hypertrophy, TNFi – TNF inhibitor. SH + PD = 0 – the absence of synovitis on B-mode and PD, B-mode ≤ 1 and PD = 0 – a grade ≤ 1 on B-mode and a PD = 0, SH ≤ 1 and PD ≤ 1 – synovitis grade ≤ 1 on B-mode and PD, PD = 0 – the absenceof synovitis PD, PD ≤ 1 – a grade ≤ 1 of synovitis PD, SH + tenosynovitis on B-mode and PD = 0 – the absence of synovitis and tenosynovitis on B-mode and PD.
Some authors defined it as an absence of joints with PD signal [7, 25–28]. Others accepted a more stringent definition, which requires the absence of SH and PD [18, 25, 29–32].
Saleem et al. [25] accepted a minimal amount of synovitis and defined US remission as a grade of SH and PD ≤ 1 for each scanned joint, and several authors accepted a minimal residual PD signal (total PD activity score ≤ 1) [25, 33]. However, these studies assessed synovitis only.
Other studies were focused on joint sites as a whole, including the joints and adjacent tendons most affected in RA [20, 34]. However, these studies are infrequent. In the Italian STARTER study, including 361 patients, synovitis and TS were considered in the presence of grade ≥ 1 in B-mode or PD [20]. This study demonstrated that tendon and joint US can be useful in assessing the variation of the inflammatory activity in RA in clinical remission [20]. The study by Harman et al. [34], involving 64 patients, also assessed US remission in the joints and tendons.
Our study population showed less US remission than in the literature (Table III) except for the definition grade ≤ 1 of PD. These results can be related to the number of joints and tendons included, the clinical definitions of remission used, stringently treatment strategies, differences in the applied scoring systems, and the existence of factors influencing US remission like duration of RA and remission or erosive RA.
In the literature, US remission varied between 0 and 78% in clinical remission (DAS28–ESR) (Table III). The synovial hypertrophy and PD was absent in 0–51.1% of patients [18, 25, 29–32, 34–36]. Ultrasound remission defined by grade ≤ 1 of SH and the absence of PD was seen in 33–58% of patients [36, 37], and in 56% if the PD had a grade ≤ 1 [25]. Joint PD was absent in 42 to 58% [25, 26, 33, 36]. A grade ≤ 1 of PD was reported in 62 to 78% [33].
In these studies, US remission was sought only in the joints. Vlad et al. [22] reported that all tendons showed US remission. In another study, SH, B-mode TS, and PD were absent in 43.9–49.6% of patients [34]. A second study did not find B-mode synovitis and TS in 19.1% of patients and PD mode in 49% of patients [20].
This study underlines the role of US in clinical practice because even the stringent clinical remission criteria could not totally reflect the “true” remission in a large number of joints and tendons. Moreover, its role in RA remission management has been a subject of debate in recent years [28, 38]. Recently, US was recommended during follow-up in some situations or during treatment tapering in clinical remission by the GEISPER French group [39]. The therapeutic decision was considered in the presence of synovitis or TS with Doppler signal.
Study limitations
The present study has several limitations. The first was the small number of patients. However, this is a convenience sampling of patients in remission over a period of one year. Secondly, we aimed to explore the maximum number of joints, but some sites such as the hip are difficult to assess with a US probe whose frequency is above 6 MHz. Thirdly, US is an operator-dependent imaging technique. However, it was improved by a standardized imaging acquisition technique and performed by an experienced rheumatologist. Finally, a subsequent follow-up to detect relapses and radiographic progression, and correlate them to the results of US data would be of interest in defining US remission.
Conclusions
The present study confirms data from previous studies on the persistence and frequency of synovitis and TS in B-mode and PD in RA in clinical remission. All the remission criteria, even when classified as strict, showed inflammatory activity. The frequency of US remission varies from 5.4 to 62.2% depending on the US definitions and activity indices used.
Further studies are needed to assess whether these findings are also associated with clinically and radiographically significant outcomes.