Introduction
Sjögren’s syndrome (SS) is a heterogeneous disease with different manifestations in different patients [1]. Therefore, the diagnosis is often challenging, and the condition is overdiagnosed by rheumatologists as well as by dentists. Although dry mouth, dry eye, and swollen salivary glands are the hallmark manifestations of SS, the likelihood of an alternative diagnosis should also be considered.
Parisis et al. [2] have defined a spectrum of differential diagnoses in patients with suspected SS, including use of xerogenic medications, aromatase inhibitors, checkpoint inhibitors, age-related dryness, metabolic sialoadenosis, non-SS dry eye disease, head and neck irradiation, sarcoidosis, some types of hyperlipoproteinaemia, chronic graft versus host disease, primary lymphoma, amyloidosis, viral or chronic non-specific sialadenitis, diabetes mellitus, hemochromatosis, rheumatoid arthritis, granulomatosis with polyangiitis, IgG4-related disease (Mikulicz syndrome), other connective tissue disease, anxiety, and fibromyalgia.
The diagnostic challenge is mainly encountered in patients presenting with dry eyes and/or dry mouth, who do not meet the ACR/EULAR classification criteria. Differentiation between a true SS and other conditions that may be associated with sicca syndrome is crucial for routine clinical practice. This differentiation is not difficult if anti-SSA/Ro antibodies are present; however, these antibodies are found only in two-thirds of patients with primary SS [3].
In the absence of anti-SSA/Ro antibodies, a salivary gland biopsy, which is an invasive procedure, is warranted for the diagnosis. Interpretation of the biopsy results may be not straightforward even for experienced pathologists, mainly due to the lack of an international consensus on salivary gland histopathology. Currently the diagnostic value of salivary gland ultrasonography is being evaluated in SS, and normal salivary gland ultrasonographic findings have been shown to rule out SS in anti-SSA-negative patients with sicca syndrome [4].
Material and methods
The relevant literature describing differential diagnosis of sialoadenosis and associated conditions was reviewed. We searched PubMed, ScienceDirect, and Google Scholar databases using the following combinations of words: sialoadenosis, parotid swelling. Relevant references cited in the selected papers were searched manually and included in the review.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) for Individual Patient Data (IPD) systematic reviews was used [5].
Case description
A 23-year-old female was referred to the rheumatology clinic with a 2-year history of persistent swelling of salivary glands disfiguring her face and an occasional sensation of dryness in her eyes and mouth. She had no documented diagnosis until a diagnosis of SS was established in one of the clinics 8 months before presentation. There she was treated accordingly with no effect.
On inspection, the face was disfigured (Fig. 1 A–D) due to bilateral parotid gland enlargement. The glands were soft and non-tender on palpation. The oral mucosa appeared pink and moist. Salivary gland massage resulted in discharge of moderate amounts of transparent saliva. No relevant abnormalities in other organs were noted. Complete blood count, urinalysis, and blood chemistry tests were within the normal range. The patient also had negative results for antinuclear, anti-Ro/SSA, and anti-La/SSB antibodies.
Fig. 1
A–D. Appearance of the patient at presentation. Images showing bilateral parotid enlargement disfiguring her face were taken by the patient with her phone and used with her consent.

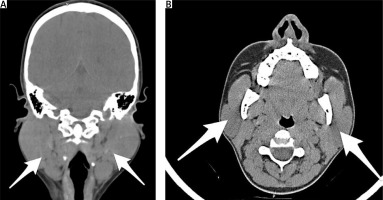
CT scan (Fig. 2 A, B) demonstrated symmetric enlargement of parotid glands.
Fig. 2
Axial (A) and coronal (B) computed tomography scans showing diffuse enlargement of both parotid glands (arrows).
Biopsy of the salivary gland parenchyma revealed seromucous acini of regular structure with localized areas of ductal involution and dilatation. The ducts were lined with cubo-cylindrical epithelium, either simple or bistratified. The interstitium was fibrotic with rare lymphocytes and plasmocytes. No focal alterations, epithelioid cell granulomas, or signs of malignant cell proliferation were detected. Overall, the biopsy findings were consistent with subnormal salivary gland parenchyma. The sialometry result was normal.
The patient was subsequently referred to an ophthalmologist, with complaints of persistent redness and dryness of both eyes for the past 2 years. For dry eye evaluation complete ophthalmologic examination included the Schirmer test, slit-lamp examination for assessment of tear break-up time (TBUT), and ocular surface fluorescein staining [6–8]. Diagnostic ophthalmological tests revealed complex myopic astigmatism and mild amblyopia with best corrected visual acuity of 20/60 in the right eye and 20/40 in the left eye. Abnormally low tear production revealed by Schirmer test, tear instability revealed by the TBUT test, and mild fluorescein staining of the paracentral cornea confirmed the presence of dry eye syndrome (DES). Because the clinical examination and serological laboratory tests did not confirm a systemic autoimmune disease, the dry eye was regarded as non-Sjögren DES.
The common shared features of SS and sialoadenosis in this case were salivary gland enlargement, and dryness in the mouth and eyes. Xerostomia appeared to be just a subjective sensation and was not by sialometry findings. The absence of immuno-specific markers and the lack of characteristic biopsy features allowed us to exclude the diagnosis of SS. The patient gave a positive answer to ocular and oral symptoms (inclusion criteria), and there was only 1 criterion of SS (Schirmer’s test ≤ 5 mm/5 minutes in at least 1 eye) giving her 1 point, and this was not enough for the patient to fit the classification criteria of primary SS [9].
The patient was diagnosed with idiopathic sialoadenosis. More in-depth history taking revealed that the patient was treated by a psychiatrist 5 years ago for bulimia. Therefore, another psychiatric consultation was arranged.
According to the psychiatrist’s report, this patient first came to their view 5 years ago (at the age of 18 years) while a first-year university student. The girl came to study from abroad, which required changes in her usual living conditions and carried a heavy load on the adaptation process. At that time, the patient showed mental disorders of the anxiety-depressive spectrum. The patient complained of anxiety, which prevented her from daily tasks and led to sleep disturbances, low mood, loss of motivation and interest in studying, and decreased attention. The girl missed classes, although she was a capable and responsible student. In a detailed interrogation, she categorically denied eating disorders, although it was clear that the patient did not fully disclose the content of her emotional experiences, which was regarded by us as a cultural secrecy.
The psychological disorder was considered a consequence of insufficient adaptive resources, because the girl had travelled hundreds of kilometres to study abroad, left her family, and had to get used to a different mentality, traditions, and peculiarities of life. According to the results of scientific research, emigrants have different degrees of severity of mental adaptation disorders, manifested in disharmonious personality structure, inadequate ways of emotional response to conflict, and violation of the system of interpersonal and microsocial interaction. Disorders in the psycho-emotional sphere of migrants are known to cover an extremely wide range of pathological manifestations, affecting the emotional, cognitive, behavioural, motivational-demanding, communicative spheres; overlapping, they can lead to global personality disorders [10].
The patient was diagnosed with adaptation disorder and anxiety-depressive reaction (F43.22), and appropriate treatment was prescribed: sertraline 20 mg once daily along with cognitive-behavioural therapy. Pharmacological therapy lasted for about 6 months. By the end of the 1st year the patient regularly attended consultations, and a considerable improvement was noted. However, later the patient started missing classes again, was not showing any activity, and eventually stopped attending psychotherapy. After that, contact with her was lost for several years.
The current visit to a psychiatrist was after the referral of a rheumatologist and a dentist due to disfiguration of her face, as this had become a priority. After many examinations and consultations, the specialists linked the change in the student’s mood with the change in her appearance causing self-doubt: the girl had to wear clothes that covered the swelling. In addition, the patient complained of dry mouth, poor sleep with early awakenings, anxiety about her health and her future, constipation, and loss of motivation and opportunities to enjoy life and the things that used to be fun.
While working with the patient it became possible to establish a relationship of trust, and only then did she openly speak about her eating disorders and their causes. We came to know that the patient periodically induced vomiting (occasionally it was repeated daily for up to 2 weeks). Vomiting turned out not to be the result of overeating, nor was it associated with dietary errors. It was not aimed to decrease body weight either (the patient did not care about her weight and was satisfied with her appearance; patient’s body mass index was 22.5, and the diagnosis of anorexia was not established). While feeling anxiety, she listened to advice of her friend, who shared the experience of her family according to which it was possible to reduce emotional pain and to get rid of anxiety by releasing stomach contents. Artificially induced vomiting brought her physical and, most importantly, situational psychological relief. Since then, in moments of anxiety, depression, and sadness, the patient made herself vomit and, in her opinion, felt better. Vomiting acted as a defence mechanism against emotional pain and helped to control the stressful situation.
Thus, the vicious circle closed: the source of stress-internal tension-vomiting-relief. Unfortunately, the patient was afraid and ashamed to talk about vomiting, and as a result, she felt guilty and imperfect. Periods of well-being, when the patient managed to live without vomiting, were alternating with exacerbations.
The patient was diagnosed with an obsessive-compulsive disorder. She was prescribed fluoxetine 20 mg once daily and pregabalin 75 mg at night-time. In addition, the patient started rational psychotherapy and cognitive-behavioural therapy. The patient’s condition improved significantly as a result of treatment for 2 weeks: vomiting was not observed, the gland decreased in size by day 8 of treatment (Fig. 3. a–c), and the patient noted improvement in her mood and sleep.
Results
The search retrieved 46 results (Fig. 4). Of them, 19 publications were found eligible for inclusion and were subsequently discussed. The reasons for exclusion were as follows: non-clinical studies (n = 6), i.e. studies discussing exclusively morphology, physiology and sialochemistry in sialoadenosis; reports of congenital malformations (n = 2), in particular, agenesis of parotid gland with contralateral swelling and sialoadenosis; studies limited exclusively to discussion of diagnostic and treatment techniques (n = 6); reports of sialoadenosis resulting from alcohol abuse (n = 2), nicotine use (n = 1), diagnosed systemic disease or endocrine disorders (n = 3), cases of sialoadenosis attributed to pharmacological side-effects (n = 5), mostly related to clozapine and valproic acid; and literature reviews (n = 2).
Discussion
Sialoadenosis is defined as non-inflammatory, non-neoplastic swelling of the salivary glands. It may be related with endocrine and metabolic disorders (e.g. diabetes mellitus, gonadal dysfunction, pituitary and thyroid pathology). It has also been associated with dystrophic processes seen in malnutrition, hypovitaminoses, alcohol abuse, chronic liver disease, and autonomic nervous system dysfunction [11]. Over 40 years ago data regarding bilateral parotid enlargement in subjects form developing countries consuming high amounts of carbohydrates were reported [12]. In contrast, in the Western world this condition is predominantly associated with eating disorders [13]. The first case demonstrating an association between vomiting and parotid enlargement was described by Lavender [14] in a 17-year-old apprentice carpenter with surreptitious vomiting and hypokalaemic alkalosis. This association has been confirmed in further studies [15, 16].
Although the exact underlying mechanisms remain obscure and await further studies, 2 hypotheses exist to explain the interrelationship between vomiting and parotid swelling. According to one of them, repeated cholinergic stimulation of the parotid resulting from frequent vomiting leads to parotid enlargement due to increased saliva flow [17, 18]. The second hypothesis explains parotid swelling as the result of the action of pancreatic enzymes on oral mucosa [19].
Taking into account the growing number of publications on the combination of DES with psychiatric conditions, as well as the presence of obsessive-compulsive disorder in the described patient, it could be assumed that the latter induced her DES [20–22]. In particular, the mechanisms of DES development could also be influenced by stress-induced suppression of lacrimal gland function [23]. There is also research showing that decreased serotonin levels, often found in psychiatric disorders, may also be associated with autonomic nervous dysregulation of lacrimal gland function and with atrophy and autophagy of the lacrimal gland [6]. Frequent episodes of vomiting in patients may also be an important factor in the development of subjective symptoms of DES because, according to current data, gastro-oesophageal reflux disease may be associated with the development of ocular surface diseases and, in particular, with the development of dry eye [24–26].
However, despite the evidence listed above, the pathophysiological mechanisms of the association of DES with psychiatric disorders still require more detailed investigation.
The reported patient’s symptoms were related to repeated vomiting in the setting of obsessive-compulsive disorder. Although bulimia is considered to be a common cause of sialoadenosis [17, 27, 28] and eating disorders and obsessive-compulsive personality traits frequently coexist [29], parotid enlargement, to the best of our knowledge, has not been previously described in association with obsessive-compulsive disorder. Recurrent vomiting may well be a common pathophysiological link in all these cases.
Conclusions
Diagnosing sialoadenosis and establishing its underlying cause is important for successful treatment. General practitioners and rheumatologists may be the first contact physicians of patients with this rare condition due to parotid swelling and associated sicca syndrome. Therefore, raising awareness among rheumatologists about sialoadenosis is crucial for the avoidance of misdiagnoses and for successful management of these patients.





