While earlier studies among coronavirus disease 2019 (COVID-19) positive children were linked with lower odds of death, several reports of severe systemic inflammatory disease among children with a close resemblance to features of Kawasaki disease were reported during the pandemic [1, 2]. The term multisystem inflammatory syndrome in children (MIS-C) was coined. While the criteria varied slightly based on different organizations, the presence of fever (≥ 38°C/100.4°F) for 24 hours or more, involvement of several organ systems, and the presence of elevated inflammatory markers with no alternative plausible causes are common among them [2, 3]. The presence of either a recent or current COVID-19 infection or exposure to a closed contact is also one of the criteria listed by the Centers for Disease Control and Prevention (CDC) [3]. Since most studies of MIS-C among COVID-19-positive patients involved smaller samples, we performed a retrospective study using one of the biggest in-patient records from the United States.
Our study followed the age criteria set by the CDC and included patients between 0 and 20 years of age from the 2021 National Inpatient Sample (NIS) [3]. The NIS is part of the Healthcare Cost and Utilization Project (HCUP), which is designed to collect inpatient records in a de-identified fashion. Cases of COVID-19 were identified using the ICD-10 code U07.1 and MIS-C via the code M35.81. We estimated the presence of MIS-C in COVID-19 cases per 100,000 COVID cases for age groups, race, and sex using the following formula: MIS-C patients in that group/total COVID-19 cases in that group × 100,000. The number of MIS-C cases meeting the criteria for Kawasaki disease was also estimated. Discharge weights (DISCWT) were used for our analysis, allowing us to confirm national estimates of the condition [4, 5].
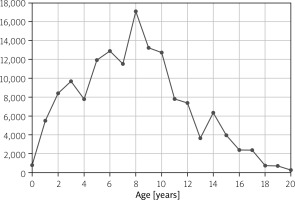
Our study identified 69,440 COVID-19 cases among children aged 0–20 (inclusive) in 2021, with 2,790 patients reporting MIS-C (4,018 MIS-C cases per 100,000 COVID-19 patients, 4.0%; Table I). Multisystem inflammatory syndrome in children incidence followed an incremental pattern with age; the highest incidence was noted in children aged 8 years (17,130 MIS-C cases per 100,000 COVID-19 patients). The incidence then gradually dropped from age 8 years to 20 years (Fig. 1). The median age of MIS-C in COVID-19-positive children was 9 years (interquartile range 4–13 years).
Table I
Incidence of MIS-C per 100,000 COVID-19 children aged 0–20 in the United States
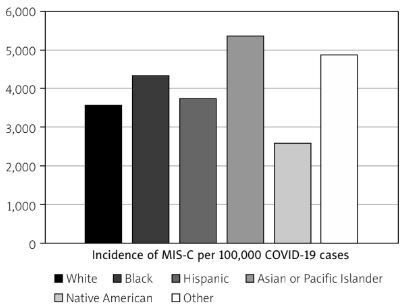
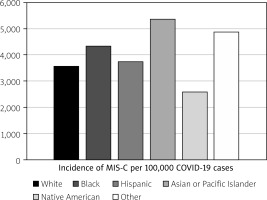
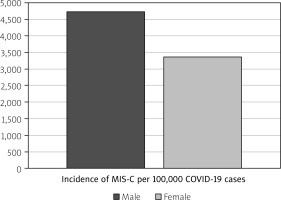
We also noted racial disparities as MIS-C was more common among Asian or Pacific Islanders (API) (5,346 MIS-C per 100,000 COVID-19 cases), with the lowest incidence noted among Native Americans (2,581 MIS-C per 100,000 COVID-19 cases) (p < 0.01; Fig. 2). In addition, a sex-based difference was observed as males had a higher rate of MIS-C (4,734 cases per 100,000 COVID-19 cases) than females (3,373 MIS-C cases per 100,000 COVID-19 cases) (p < 0.01; Fig. 3). Around 220 MIS-C cases met the criteria for Kawasaki disease (7.9%) and they were younger (mean age 5.18 years vs. 9.07 years in other MIS-C cases, p < 0.01).
To date, this is the biggest retrospective study investigating events of MIS-C among COVID-19-positive children from the United States. Among the 131 MIS-C cases with a positive COVID-19 test in a study conducted by Feldstein et al. [6], the majority were Hispanics (or Latino) (40%), which was different from our study. However, the overall median age of 9.1 years of MIS-C COVID-19 cases was similar to our study (9.1 years vs. 9.0 years) [6]. Various studies with smaller samples of MIS-C cases in COVID-19 patients included more males than females; for example, in their study of 268 cases, Flood et al. [7] had 60.1% classified as males. Studies investigating only MIS-C cases (irrespective of COVID-19 status) also found a higher proportion of males (54% in the study by Dufort et al. [8]). As there is a lack of additional data on the prevalence of MIS-C among COVID-19 children from different countries, we encourage physicians across different countries to pursue a similar investigation. Furthermore, the higher incidence among Asian/Pacific Islanders in our study also corresponds to the racial disparities previously seen in that particular group for Kawasaki disease [9]. We also noted a high incidence among Black people and agree with Middelburg et al. [10] that additional studies are necessary and awareness should be increased among physicians of such racially associated risk factors [9, 10].
To conclude, our study of MIS-C among COVID-19- positive children found the highest incidence in those aged 8, along with a higher incidence among males and APIs, and the lowest incidence among Native Americans. As MIS-C is a new condition and has a close resemblance to Kawasaki disease, it is vital for the affected children to have a close follow-up, and any presence of short-term and long-term cardiac anomalies should be treated early [11]. Similar studies across different countries with diverse backgrounds should be encouraged.