Introduction
Non-communicable diseases (NCDs) have received insufficient attention from governments in sub-Saharan Africa but as infectious diseases are being overcome and as more people live longer, rheumatic and musculoskeletal diseases (RMDs) will play increasing roles in terms of morbidity and mortality. Health policies and resources have largely been channelled towards combating infections, leading to relative neglect of NCDs including RMDs.
As a result of this awareness, both the World Health Organisation (WHO) and the International League of Associations for Rheumatology (ILAR) 1981 developed a programme to determine the prevalence, risk factors, and impact of musculoskeletal (MSK) conditions in communities of developing countries [1].
This programme, called the Community Oriented Programme for Control of Rheumatic Diseases (COPCORD), also aims at the prevention of MSK diseases by educating health workers, patients, and the community as a whole. The COPCORD study model is a low infrastructure cross-sectional community survey grouped into three stages [1].
While stage 1 aims to determine the prevalence of rheumatic disorders and is divided into three phases [1–3], the objective of stage 2 is to enhance the education of health workers, patients, and the community whereas stage 3 seeks to identify risk factors for common rheumatic disorders [1].
In spite of numerous Asian and South-American reports of the prevalence of MSK conditions using the COPCORD stage 1 model [1–5], only five African countries have reported the prevalence of MSK symptoms using this model [6–11].
For example, in a semi-urban community in North-Central Nigeria, the point prevalence of MSK complaints was 33% among 2,454 respondents [7]. In Central and East Africa, a prevalence of 45.9% was documented among 1,500 rural Congolese and 12% in a pilot study of MSK pain in 3,384 subjects from Kenya, respectively [8, 9].
In North Africa, the prevalence of MSK complaints was 16.2% in the rural Egyptian population [10] and 31.1% from a mixed rural and urban Tunisian population [11]. There is an increasing burden and impact of MSK conditions in African communities and this is a cause for concern.
The 2016 Global Burden of Diseases report showed that NCDs accounted for 80.6% of years lost to disability (YLD) compared to communicable diseases and injuries (19.4%) [12]. Furthermore, the report showed that MSK disorders were one of the five leading causes of disability worldwide, with disability-adjusted life years (DALYs) increasing by 19.6% between 2006 and 2016 [11–13].
Despite evidence for the rising prevalence of MSK conditions worldwide, data from Africa are few [14]; similarly, reports on functional disability of MSK conditions are even fewer, thus, highlighting a need for studies from large African populations. Although there has been a previous COPCORD study from North Central Nigeria [7], there have not been any other such studies from the southern part of the country with its distinct and contrasting socioeconomic, cultural, and demographic differences.
Thus, this research seeks to study the prevalence and pattern of MSK diseases as well as the associated functional disability in a peri-urban population in the South-West area of Nigeria.
Material and methods
This study was a community-based cross-sectional study. The study area was Agbowa, a peri-urban coastal community, located about 30 km from Ikorodu, a major town in Lagos State. Agbowa is the headquarters of the Ikosi-Ejinrin Local Council Development Area (LCDA). Based on the 2006 National Census figures, the projected population of residents aged 15 years and above was about 3825 while that of the whole LCDA is 38,281 [15].
The World Health Organization/COPCORD stage 1 model was adopted and the study population was evaluated using the three phases of the model. A convenient sampling method was used to recruit consenting respondents for the study. The minimum sample size was 340 based on a 33% prevalence from the Nigerian COPCORD study [7], a confidence interval of 1.96, and a tolerable sampling error of 0.05 [16].
Phase 1: respondents aged 15 years and above were screened by trained field assistants using a pre-tested interview-based modified COPCORD phase 1 questionnaire, to document socio-demographic parameters. This was done in a house-to-house survey.
Phase 2: respondents who completed phase 1 were screened by trained community health workers, rheumatology trainees, and medical students using the interviewer-administered modified COPCORD phase 2 questionnaires to document specific sites of MSK complaints in at least the past 1 week, the impact on functional disability, difficulty in performing specific tasks and any past treatment. Specific MSK complaint sites were indicated on the questionnaire with pain intensity assessed using the Numerical Rating Scale (NRS) [17] while functional disability was assessed using the Health Assessment Questionnaires Disability Index (HAQ-DI) [18].
Phase 3: positive responders from the phase 2 survey were further evaluated by the rheumatologists and rheumatology trainees for RMDs using modified COPCORD phase 3 questionnaires to document findings from history, general and systemic examination, rheumatologic assessment, as well as laboratory investigations. The diagnoses of RMDs were based on relevant American College of Rheumatology (ACR) criteria [19–25], Brighton criteria [26], and Southampton criteria [27].
Rheumatic conditions that could not be classified using the above criteria were diagnosed clinically by the rheumatologists among the investigators. All 3 phases were conducted concurrently and the whole survey lasted 6 months starting from October 2015 to March 2016.
Statistical analysis
Statistical software IBM SPSS version 21 was used for data analysis. Socio-demographics, the prevalence of MSK complaints, and clinically diagnosed RMDs were presented as proportions. A comparison of socio-demographic variables and MSK risk factors between respondents with and without MSK complaints was done using the χ2 test. Multivariate logistic regression was used to determine independent predictors of MSK complaints in the study subjects.
The functional disability assessed by HAQ-DI was reported as median with interquartile range (IQR). The degree of disability was categorized with a score ≥ 1 indicating significant disability; mild disability (was defined by scores > 0 but < 1), moderate disability as 1–2 and severe disability as > 2 [18]. Pain intensity was assessed using NRS and reported: no pain (NRS 0), mild (NRS 1–3), moderate (NRS 4–6), or severe (NRS 7–10) [17].
Bioethical standards
The study was approved by the Ethics Committee of the Lagos State University Teaching Hospital (LASUTH) and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Permission was also obtained from local authorities including the Community Head of Agbowa town. Verbal and written informed consents was obtained from every respondent using a signature or thumbprint.
Results
Socio-demographic characteristics of the study population
Three thousand and fifty-six respondents aged 15 years and above consented and completed the interview-based modified phase 1 questionnaire, giving a response rate of 79.8% in a target population of 3,825. The median age of the respondents was 40 years (IQR: 28–52) with the majority (51.4%) within the age group 25 to 44 years. The respondents were predominantly females (59.2%) with a comparable median age between the sexes: female 39 years (IQR: 29–52), male 40 years (IQR: 27–53); p = 0.107.
Trading (38.3%) was the most frequent occupation in our study population while the majority were Christian (55.8%) and were married (65.1%). Those with primary education comprised 43.9% while about half (54.3%) could read and write. About 22.3% had ingested different types of alcohol either in the past or currently. Fifty-four percent (54%) had however never ingested alcohol, smoked, or used recreational drugs. The socio-demographic characteristics of the study population are shown in Table I.
Table I
Socio-demographics and co-morbidities of study population
| Variables | All respondents N = 3,056 n (%) | Respondents with MSK complaints (n = 1,773) | Respondents without MSK complaints (n = 1,283) | p-value |
|---|---|---|---|---|
| Male | 1,248 (40.8) | 659 (37.2) | 589 (45.9) | 0.001 |
| Female | 1,808 (59.2) | 1,114 (62.8) | 694 (54.1) | |
| Positive family history of MSK conditions | 923 (30.2%) | 740 (41.7) | 183 (14.2%) | 0.001 |
| Age range | ||||
| Young (≤ 45 years) | 1,018 (33.3) | 460 (25.9) | 558 (43.5) | 0.001 |
| Middle age (46–64 years) | 1,341 (43.9) | 811 (45.7) | 530 (41.3) | |
| Elderly (≥ 65 years) | 697 (22.8) | 502 (28.3) | 195 (15.2) | |
| Occupation | ||||
| Student | 276 (9) | 134 (7.6) | 142 (11.1) | 0.001 |
| Farm work | 556 (18.2) | 329 (18.6) | 227 (7.7) | |
| Public servant | 439 (14.4) | 272 (15.3) | 167 (13) | |
| Others* | 614 (20.1) | 369 (20.8) | 245 (19.1) | |
| Trading/business | 1,172 (38.3) | 669 (37.7) | 502 (39.1) | |
| Religion | ||||
| Christianity | 1,705 (55.8) | 990 (55.8) | 715 (55.7) | 0.392 |
| Islam | 1,270 (41.6) | 742 (41.8) | 528 (41.2) | |
| Traditional religion | 55 (1.8) | 30 (1.7) | 25 (1.9) | |
| Others | 26 (9) | 11 (0.6) | 15 (1.2) | |
| Marital status | ||||
| Single | 799 (26.1) | 379 (21.4) | 420 (32.7) | 0.001 |
| Married | 1,988 (65.1) | 1,211 (68.3) | 777 (60.6) | |
| Widowed | 226 (7.4) | 160 (9) | 66 (5.1) | |
| Separated/divorced | 43 (1.4) | 23 (1.3) | 20 (1.6) | |
| Education | ||||
| Primary | 1,343 (43.9) | 791 (44.6) | 552 (44) | 0.88 |
| Secondary | 734 (24) | 423 (23.9) | 311 (24.2) | |
| Tertiary | 183 (6.0) | 105 (5.9) | 78 (6.1) | |
| Informal | 244 (8.0) | 143 (8.1) | 101 (7.9) | |
| None | 552 (18.1) | 311 (17.5) | 241 (18.8) | |
| Literacy | ||||
| Read only | 932 (30.5) | 511 (28.8) | 421 (32.8) | 0.060 |
| Read and write | 1,658 (54.3) | 987 (55.7) | 671 (52.3) | |
| None | 466 (15.2) | 275 (15.5) | 191 (14.9) | |
| Habit | ||||
| Ever smoked | 184 (6.0) | 105 (5.9) | 79 (6.2) | 0.893 |
| Ever drink alcohol | 683 (22.3) | 410 (23.1) | 273 (21.3) | |
| Current smoker | 122 (4.0) | 72 (4.1) | 50 (3.9) | |
| Current alcohol drinker | 308 (10.1) | 175 (9.9) | 133 (10.4) | |
| Recreational drugs | 109 (3.6) | 62 (3.5) | 47 (3.7) | |
| Co-morbidities | 1,978 (64.7) | 1,012 (57.1) | 966 (75.3) | 0.001 |
| History of hypertension | 918 (30.0) | 572 (32.3) | 346 (27) | 0.002 |
| History of diabetes | 167 (5.5%) | 107 (6.0%) | 50 (3.9%) | 0.008 |
| Obesity (BMI ≥ 30 kg/m2) | 303 (9.9%) | 197 (11.1%) | 106 (8.3%) | 0.009 |
| History of PUD | 892 (29.2%) | 682 (38.5%) | 210 (16.4%) | 0.001 |
| History of trauma | 545 (17.8%) | 414 (23.4%) | 131 (10.2%) | 0.001 |
| History of sickle cell disease | 42 (1.37) | 23 (13) | 19 (1.5) | 0.667 |
| History of asthma | 69 (2.3) | 27 (1.5) | 42 (3.3) | 0.001 |
Prevalence of musculoskeletal conditions in the study population
Musculoskeletal pain
As shown in Tables I and II, the period prevalence of MSK pain among the 3056 respondents recruited in phase 1 for the phase 2 study was 58% (n = 1,773 CI: 56.3–59.8%).
Table II
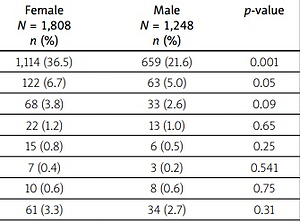
Prevalence and gender distribution of rheumatic and musculoskeletal diseases in 3,056 respondents
| RMDs | All respondents N = 3,056 n (%) | Female N = 1,808 n (%) | Male N = 1,248 n (%) | p-value |
|---|---|---|---|---|
| MSK pain | 1,773 (58) | 1,114 (36.5) | 659 (21.6) | 0.001 |
| Osteoarthritis (OA) | 185 (6.1) | 122 (6.7) | 63 (5.0) | 0.05 |
| Knee OA | 101 (3.3) | 68 (3.8) | 33 (2.6) | 0.09 |
| Hip OA | 35 (1.1) | 22 (1.2) | 13 (1.0) | 0.65 |
| Shoulder OA | 21 (0.7) | 15 (0.8) | 6 (0.5) | 0.25 |
| Hand OA | 10 (0.3) | 7 (0.4) | 3 (0.2) | 0.541 |
| Generalised OA | 18 (0.6) | 10 (0.6) | 8 (0.6) | 0.75 |
| Chronic low back pain | 95 (3.1) | 61 (3.3) | 34 (2.7) | 0.31 |
| Soft tissue rheumatism | 52 (1.7) | 37 (2.0) | 15 (1.2) | 0.08 |
| Adhesive capsulitis | 8 (0.3) | 6 (0.3) | 2 (0.2) | 0.48* |
| Rotator cuff tendinitis | 6 (0.2) | 5 (0.3) | 1 (0.08) | 0.41* |
| De Quervain’s tendinitis | 7 (0.20) | 5 (0.5) | 2 (0.2) | 0.71* |
| Trigger finger | 6 (0.2) | 4 (0.2) | 2 (0.2) | 1.00* |
| Carpal tunnel syndrome | 4 (0.13) | 3 (0.2) | 1 (0.08) | 0.65* |
| Others** | 21 (0.69) | 17 (0.9) | 5 (0.4) | 0.85 |
| Joint hypermobility syndrome | 20 (0.7) | 14 (0.8) | 6 (0.5) | 0.32 |
| Fibromyalgia | 17 (0.6) | 15 (0.8) | 2 (0.2) | 0.01* |
| Gout | 9 ( 0.3) | 8 (0.4) | 1 (0.08) | 0.09* |
| Rheumatoid arthritis | 1 (0.03) | 1 (0.06) | 0 (0) | 1.00* |
| Systemic sclerosis | 1 (0.03) | 1 (0.06) | 0 (0) | 1.00* |
The current history of MSK pain was documented in 62.5% (n = 1,109) of the respondents. Monoarticular involvement was noted in 40.8% (n = 723) of the study respondents with the knee being the most frequently affected joint (Table III).
Table III
Sites of musculoskeletal pain in the study population
The percentage of female subjects with MSK pain was significantly higher than in males (62.8% vs. 37.2%, p = 0.001). Subjects with MSK pain were significantly older than subjects without MSK pain (p = 0.001) and most (26.3%) were within the age group 35 to 44 years.
Respondents with MSK pain were predominantly traders and farmers and more than half could read and write. Family history of RMDs was reported in 30.5% (n = 540) of the subjects with MSK pain and past history of musculoskeletal trauma was observed in 17.9% (n = 317).
About one-tenth of the respondents with MSK pain smoked cigarettes while up to one-fifth drank alcohol. In addition, 9.5% (n = 168) were obese and at the same time 5.3% (n = 94) were known to be diabetic. Twenty-three percent of the respondents used over-the-counter drugs with more than two-thirds having self-administered NSAIDs while 1 in 10 had self-medicated oral steroid tablets. A history of peptic ulcer diseases was reported in 28.5% (n = 506).
The reported intensity of MSK pain as assessed by NRS was mild, moderate, severe, and very severe in 106 (16%), 269 (40.5%), 249 (36.9%), and 38 (5.7%) respectively. The median HAQ-DI was 0.6 (IQR 0.1–1.8), indicating mild disability from MSK pain but significant disability (HAQ-DI ≥ 1 was found in 39.5%) of the subjects. Severe, moderate, and mild disability was recorded in 18%, 21.5%, and 54.9% respectively.
Restrictions were documented in family relations (n = 432, 24.3%), marital relations (n = 529, 29.8%), socio-religious (n = 439, 24.8%), financial (n = 518, 29.2%), household chores (n = 759, 42.8%) and occupation/school activities (n = 784, 44.2%).
The results of the χ2 analysis showed that female gender, family history of MSK conditions, history of previous trauma, diabetes, hypertension, peptic ulcer disease, asthma, and obesity were significantly associated with the presence of MSK pain (Table I).
However, further tests of these independent variables using logistic regression with the presence of MSK pain as an outcome did not show any significant independent predictors of MSK pain.
Clinically diagnosed rheumatic and musculoskeletal conditions
In phase 3, three hundred and eighty subjects from the 1,773 subjects with MSK complaints in phase 2 had clinically diagnosed RMDs, giving a period prevalence of 12.4% (CI: 11.3–13.7%).
Up to two-thirds of subjects with RMDs were female (62.4%, n = 237, p = 0.019) and 46.1% (p = 0.001) had a family history of RMDs. The majority of the subjects (33.4%, n = 127) were between 35 and 44 years of age with a median age of 38 years (IQR 30–53).
As shown in Table II, osteoarthritis (n = 185, 6.1% CI: 5.2–6.9%) was the most frequent condition documented in our study population. This was followed in decreasing order by chronic low back pain (n = 95, 3.1% CI: 2.5–3.7%), soft tissue rheumatism (n = 52, 1.7% CI: 1.2–2.1%), benign joint hypermobility syndrome (n = 20, 0.7% CI: 0.3–0.9%), fibromyalgia (n = 17, 0.6% CI: 0.3–0.8%) and gout (n = 9, 0.3% CI: 0.1–0.5%). While the prevalence of rheumatoid arthritis (n = 1, 0.03% CI: 0.03–0.10) and systemic sclerosis was similar, there was no case of vasculitis, lupus, or any other connective tissue disease.
The median duration of RMDs was 8 years (IQR 3.1–13). Farm work (19.7%, n = 75) and trading (19.7%, n = 75) were the predominant occupation. Among phase 3 subjects with diagnosed RMDs, anaemia was documented in 34.5% (n = 131), hyperuricemia in 27.4% (n = 104), elevated serum creatinine in 23.4% (n = 89), elevated serum CRP in 4.2% (n = 16) and elevated rheumatoid factor in 2.4% (n = 9).
Discussion
Our study has shown a 58% prevalence of MSK pain, which is higher than previous prevalence reports from other African COPCORD studies [2, 6–11]. The first COPCORD study in West Africa found a prevalence rate of 33% among the 2454 study population from a semi-urban community in Jos, Nigeria [7].
The COPCORD studies from Kenya and Egypt reported much lower prevalence rates of 12% and 16.2% respectively [2, 9], with Tunisia recording a prevalence of 33% while almost half of a Congolese study population had MSK pain [8, 11], as shown in Table IV.
Table IV
Comparison of African COPCORD studies
| Variables | Nigeria Lagos (this study) | Nigeria Jos 2017 [7] | Egypt 2020 [6] | Tunisia 2005 [11] | Congo 2017 [8] | Kenya 2013 [9] |
|---|---|---|---|---|---|---|
| Location | Peri-urban | Semi-urban | Rural | Rural and urban | Rural | Urban |
| Sample size | 3,056 | 2,454 | 3,988 | 1,582 | 1,500 | 3,384 |
| Prevalence of MSK symptoms | 58% | 33% | 16.2% | 31.1% | 49.5% | 12 % |
| Sex | ||||||
| Female | 62.8% | 57% | 10.4% | 43.2% | 57.1% | NA |
| Male | 37.2% | 43% | 5.8% | 29.1% | 42.9 % | |
| Commonest sites of pain | Knee 54.6% | Low back 19.5% | Knee | Knee 19.3% | Knee | NA |
| Osteoarthritis | 6.1% | 22.1% | 8.5% | NA | 36.8% | NA |
| Chronic lower back pain | 3.1% | NA | 6.6% | NA | NA | NA |
| STR | 1.7% | 15.5% | 6.6% | NA | 5.8% | NA |
| JHS | 0.7% | NA | NA | NA | NA | NA |
| Fibromyalgia | 0.6% | 1.5% | 0.6% | NA | NA | NA |
| Gout | 0.3% | 0.1% | 0.6% | NA | 0.6% | NA |
| Rheumatoid arthritis | 0.03% | 0.4% | 0.3% | NA | 1.4% | NA |
| Systemic sclerosis | 0.03% | NA | NA | NA | NA | NA |
| Functional disability | 39.5% | 14.7% | 66.7% | 60% | NA | NA |
Although similar to this study, COPCORD studies from Iran and Argentina reported a high prevalence of MSK complaints in more than half of their study population [28–30]. Most COPCORD studies outside Africa reported a prevalence rate below 50% [1–5]. The conflicting prevalence figures may be attributable to variations in methodology and case definitions for MSK symptoms adopted in various studies.
It could also mean that the reported prevalence may be higher, possibly because of occupational factors. The distribution of MSK pain across socio-demographic lines in our study showed that it was more prevalent in females, young subjects, farmers, and traders.
The possible explanation for this socio-demographic distribution may be the over-representation of young active persons in our study population. While previous COPCORD studies showed a consistent female predominance in the gender distribution of MSK symptoms, there were disparities in other socio-demographic parameters [1, 3–5].
In the study by Courage et al. [7], the prevalence of MSK symptoms in Nigerian subjects was higher with increasing age and decreased with increasing literacy rate and educational attainment, whereas in Australian Aboriginals, MSK symptoms were frequently documented in young subjects and labourers [31].
Unlike in the first Nigerian COPCORD study, which documented the back as the most frequent site of MSK pain, most of our respondents reported the knee as the commonest site of their MSK symptoms. Notably, there have been conflicting reports on the commonest site of MSK symptoms reported in most COPCORD studies; while some reported the knee as the most frequent site [8, 11], others documented the back as the most affected site [1, 4, 5].
While osteoarthritis was generally the most diagnosed condition, we observed that low back pain was most frequently diagnosed, especially in studies that included LBP as part of clinically diagnosed rheumatic and MSK disorders [1, 4, 5].
As in previous African studies, osteoarthritis was the most prevalent RMD observed in our study population whereas chronic back pain and soft tissue rheumatism (STR) were the second and third frequently diagnosed conditions respectively [1, 6–11].
In a meta-analysis conducted in Iran, osteoarthritis (16.9%), chronic low back pain (15.7%), and STR (4.6%) were observed in decreasing order as the commonest MSK conditions among 19,786 respondents [5]. Similarly, the 2004–2010 India Bone and Joint Decades, after excluding nonspecific MSK symptoms, found osteoarthritis (4.39%) and STR as the first and second most prevalent MSK conditions respectively, among 55,000 subjects surveyed in their study population [6].
Despite an increase in hospital-based reports of systemic autoimmune rheumatic diseases (SARDs) in Africa, the rural community prevalence seems low [13, 32–35]. This has been attributable to inadequate diagnostic capacity and lack of access to rheumatologists [32].
However, a recent systematic review on rheumatic disease in Africa observed a substantial increase in publications on rheumatic disease from African authors, althought the review studies were entirely hospital-based [33].
A prospective cross-sectional survey of 268 staff and patients’ relatives at Lagos Tertiary Hospital by two authors from the present study found RMDs in 22% and MSK pain in 60.4% of the respondents, with comparable patterns of rheumatic musculoskeletal conditions [34].
The latter was a follow-up study done in 2021 and the outcomes were not much different from this study done in 2016, since population movement in Nigeria is usually minimal. The low prevalence of rheumatoid arthritis and systemic sclerosis in this study lends credence to previous reports of the low prevalence of SARDs in rural African settings in comparison with urban populations [6, 13, 35].
The bivariate data analysis in our study showed that female sex, family history of MSK conditions, history of previous trauma, diabetes, hypertension, obesity, peptic ulcer disease (PUD), and asthma were associated with MSK pain. Further analysis using a multivariate logistic regression model did not identify any independent predictors of MSK pain.
This finding contrasts with the previous Nigerian COPCORD study which showed that family history of MSK symptoms and male sex were independently associated with MSK diseases among Nigerian subjects. Elsewhere, in Mexico, older age, physically demanding work, and female sex were documented predictors of MSK symptoms [36].
Although the predictors of MSK diseases identified in various COPCORD studies vary, most have not shown a consistent association with MSK diseases [1]. Rheumatic and MSK diseases are among the leading causes of disability worldwide and COPCORD studies from South America and Asia showed a high burden of disability due to MSK conditions [12, 13, 37].
In this study, the median HAQ-DI was 0.6. This is less than 0.8 recorded in India and Cuba but more than 0.2 documented in Ecuador and Spain [38]. In Africa, there is a paucity of reports on physical disability in subjects with MSK diseases.
Despite the high disability (significant HAQ-DI = 39.5%) reported in this study and by Laatar et al. [11] in Tunisia (significant HAQ-DI = 60%), the report from Jos, Nigeria was significantly different from our finding as the significant functional disability in the latter report was only 14.7% [7].
This difference in functional disability in various studies may be attributable to the non-uniformity of disability assessment tools used in various studies and differences in understanding and cultural interpretations of HAQ questions by the subjects.
In a review by Duffield et al. [37], they opined that MSK conditions form a central part of co-morbidity clusters due to their high prevalence, shared risk factors, and pathogenesis with other long-term chronic medical conditions. The presence of MSK conditions in the study was shown to increase work disability, reduce the quality of life and increase the cost and burden of healthcare.
The high rate of usage of over-the-counter pain drugs, which are mostly NSAIDs, and steroids in this study may possibly explain the high frequency of history of peptic ulcer diseases identified in our respondents. It is well recognized that in spite of regulations guiding the dispensation of drugs, often healthcare workers in rural and semi-urban populations manage patients, prescribing all types of drugs.
Access to rheumatic-musculoskeletal services should be improved in Africa, where there is a dearth of rheumatology manpower and a lack of diagnostic and management tools [32, 39]. A possible temporary solution may be the use of nurses and healthcare workers for such care. They may be trained to identify and manage common RMDs [40]. Nigeria with a population of about 200 million has just 50 rheumatologists practising in urban centres, which means there is about 1 rheumatologist per 4 million people [33].
Study limitations
Our prevalence may not be an accurate representation of the community due to the low sample size. The observed associations and predictors of MSK pain in our subjects need further testing with a prospective cohort study. A national grant will be required to carry out large-scale nationwide epidemiology of RMDs in Nigeria. This would reveal the true prevalence in Africa’s most populous nation.
Conclusions
Musculoskeletal pain is common in the studied Lagos peri-urban community, and the knee was the most frequently affected joint. Musculoskeletal pain was common in females and young to middle-aged persons (aged 35–44 years). Osteoarthritis was the commonest diagnosed MSK condition, with female sex and co-morbid medical conditions having a significant association with the presence of MSK pain. High physical disability and restrictions in family, social, marital, and financial relations were noted in subjects with MSK pain. Systemic autoimmune diseases are rarely reported, as elsewhere
There is thus a need to increase awareness at all levels of the burden and impact of MSK diseases in Africa, a continent already grappling with the twin menace of infectious diseases and poverty.
Government investments in rheumatic and musculoskeletal education at the level of the populace, health workers, nurses, and doctors are paramount in reducing the MSK burden.