Introduction
Femoral neck fracture (FNF) is one of the most common orthopaedic traumas affecting the elderly population. It is one, besides the peritrochanteric fracture, of the osteoporotic fractures, which also include distal radius fractures and vertebral compression fractures. Femoral neck fractures are associated with high morbidity and mortality of patients due to the immobilization of the patients in bed, accompanying comorbidities and the advanced age of the patients most often affected by the injury.
There are a few ways of surgical treatment of the FNF. If the bone quality is high and the femoral head is not displaced, which is a favourable factor of good blood supply to the bone, it is possible to fix the fracture with a plate or screws. In elderly patients with osteoporotic bone and displaced femoral heads it is better to choose between hip hemiarthroplasty, or total hip arthroplasty if FNF is also accompanied by hip osteoarthritis. In this study, the authors’ main focus was on hip hemiarthroplasty.
The American Joint Replacement Registry (AJRR) from 2021 [1] revealed that between 2012 and 2020 there were 105,743 hip arthroplasty procedures for femoral neck fracture, of which 82,594 (78%) procedures were partial hip arthroplasties. The data from the Primary Partial Hip Replacement Supplementary Report [2] for the 2021 Australian Orthopaedic Association National Joint Replacement Registry showed that in the period from 2003 to 2020, 107,628 partial hip prostheses were made, and a femoral neck fracture was the main indication for this operation in over 90% of cases.
Although the percentage of hip hemiarthroplasty has been gradually declining year by year, according to the American Joint Replacement Registry, it is still an important treatment for femoral neck fractures.
In order to achieve a satisfactory result after hip arthroplasty, the correct relationship between anatomical structures such as acetabular offset, femoral offset (FO), acetabular anteversion and inclination, centre of rotation, and limb length must be restored. Due to the lack of interference in the acetabular structure during hip hemiprosthesis surgery, mainly the FO and length of the limbs must be reconstructed. Restoration of each of these components is essential for proper gait biomechanics and a satisfactory surgical outcome for the patient.
Neglecting these parameters may result in inefficiency of the abductor muscles stabilizing the pelvis, resulting in pelvic drop, limping due to limb shortening, abnormal gait pattern or chronic pain in the area of the hip joint and the operated limb associated with bone impingement, or increased tension in the gluteus medius and minimus attached to the greater trochanter. Inefficiency of abductor muscles, among other conditions such as gluteus medius and minimus tendinopathies, trochanteric bursitis or damage to muscles and tendons during total or partial hip arthroplasty surgery may also lead to chronic lateral hip pain, called greater trochanteric pain syndrome [3].
In the literature, it was observed that patients with coxa vara have higher FO and therefore performing total hip replacement with standard stem was associated with not restoring proper gluteus muscle tension and pelvic imbalance. High-offset stems were introduced to the market to allow such patients to restore proper biomechanics of the hip joint.
One of our observations on postoperative radiographs of patients operated on for femoral neck fracture is the difficulty in recreating the FO and appropriate muscle tension in patients with varus hips. In such patients, a better solution seems to be the use of high offset stems to better reproduce the FO and the biomechanics of the joint.
Inflammatory joint diseases such as rheumatoid arthritis lead to osteoporosis and increase the risk of fractures. For hip surgical procedures in these diseases a total hip replacement is preferred; however, partial hip replacement in some circumstances may also be considered.
Importantly, the indications for surgery are patient’s pain and disability, not age, especially in inflammatory joint diseases, which affect a younger population than osteoarthritis. Each discussion on the effectiveness of the surgical method, and in particular the discussion of less frequently used methods in some indications, provides important information that can be used by patients also with diseases other than osteoarthritis and osteoporosis.
The purpose of the study is to assess the radiological results after partial hip arthroplasty in patients who underwent procedures performed for femoral neck fracture. It also aims to evaluate the reconstruction of the FO using standard neck angle stems.
This study does not require approval by the institutional review board of the Medical University of Warsaw.
Material and methods
A consecutive series of 116 patients who were diagnosed with femoral neck fracture qualified for and treated with partial hip arthroplasty between January of 2017 and December of 2021 was identified. Patients included in the study were: aged ≥ 60 years on the day of surgery, diagnosed with femoral neck fracture, qualified for surgery with use of hip hemiarthroplasty and those who had pre- and postoperative radiological control appropriate for analysis. The exclusion criteria were: age < 60 years, concomitant hip osteoarthritis in affected limb and qualification for treatment other than hip hemiarthroplasty, non-diagnostic radiograph in forced position.
For the present analysis, demographic data such as gender and age at surgery (years) were collected. A total of 97 patients treated with a cemented Taperloc (Zimmer Biomet, Warsaw, IN, USA) stem with bipolar head met the inclusion criteria. All operations were performed in a level III academic hospital. All patients were operated on in the lateral decubitus position. Surgical technique using the natural interval in gluteal muscles and dissecting only one third of its attachment was used. An incision in line with the axis of the femoral shaft was performed with ⅓ distally and ⅔ proximally to the tip of the greater trochanter.
Further blunt dissection of connective and fat tissue was done to visualize the iliotibial tract. The latter structure was then incised in a slightly curved way to stay in line with fibres of the tensor fascia lata. After moving the fascia aside, visualization of the gluteus medius was done. The natural interval of the anterior third of the gluteus medius was found and carefully dissected from the bone. Then the femoral neck was easily palpable and the joint capsule was opened with a longitudinal dissection above the femoral neck.
After completing the approach the hip joint was dislocated and the femoral neck was cut accordingly to manufacturer’s technique. Then, after head and neck resection, the medullary canal was prepared for the appropriate stem size using rasps and a correct-sized stem was placed using bone cement. The acetabulum was revised to confirm the absence of unnecessary tissue, then a bipolar head was attached and the prosthesis was repositioned. Proper prosthesis placement was confirmed on X-ray images taken on the following day.
Radiographic evaluation
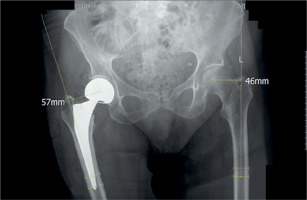
Pre- and postoperative radiographic examination of the pelvis including both hip joints in the anterior-posterior projection in the supine position was performed during patients’ hospitalisations. Retrospective analysis of radiographic images was performed. On preoperative images, the neck angle and the FO on the healthy limb were measured, and the femoral neck fracture was classified using the Pauwels and Garden scales. The FO of the operated limb was measured on the postoperative X-rays (Figs. 1–3).
Fig. 2
Postoperative femoral offset reconstructed with less than –5 mm compared to the contralateral hip in a patient with a neck-shaft angle < 130 degrees.

Fig. 3
Postoperative femoral offset reconstructed with more than 5 mm compared to the contralateral hip in a patient with a neck-shaft angle > 130 degrees.
Finally, 97 patients were included in the study, 3 patients were excluded from further measurements and analyses due to excessive forced rotation of the lower limbs on radiographs due to severe pain.
Statistical analysis
Statistical analysis of the obtained results was performed. Pearson’s correlation coefficient was used to measure the association between neck-shaft angles and FO changes. For categorical variables Fisher’s exact test was used. An α-value of 0.05 was used to determine the statistical significance of all the analyses. All statistical analyses were conducted using SAS software, Version 9.4 for Windows (SAS Institute Inc., NC, USA).
Results
There was a significant positive moderate correlation between neck-shaft angle value and FO change (r = 0.568, p < 0.0001). There was a statistically significant difference between FO change and neck-shaft angle value (24 : 52 vs. 14 : 7, p = 0.005). This means that in patients with a neck-shaft angle less than 130 degrees, that is, patients with coxa vara, the change in FO was less than –5 mm more often (14 out of 21 patients) than in patients with a neck-shaft angle equal to or higher than 130 degrees (24 out of 76 patients).
It also means that in patients with a neck-shaft angle equal to or higher than 130 degrees, the change in FO was more often greater than –5 mm (52 vs. 24 patients). Forty-two out of 97 patients had the FO restored within a safe range (between –5 mm and 5 mm), 38 patients had a FO change less than –5 mm and 17 patients had a FO change greater than 5 mm.
The patients’ characteristic and the information about patients’ age, FO change and neck-shaft angle value are presented in Tables I–III.
Table I
Baseline characteristics in both groups of patients
| Variable | Neck-shaft angle equal to or higher than 130 degrees | Neck-shaft angle less than 130 degrees | p-value |
|---|---|---|---|
| Gender (males, females) | 15 : 61 | 5 : 16 | > 0.05 |
| Operated side (left, right) | 32 : 44 | 6 : 15 | > 0.05 |
Table II
Information about patients’ age, femoral offset change and neck-shaft angle value
| Parameter | Mean value | Minimum value | Maximum value |
|---|---|---|---|
| Age [years] | 83.14 (SD = 7.83) | 60.00 | 95.00 |
| Femoral offset change [mm] | –3.19 (SD = 9.23) | –28.00 | 16.00 |
| Neck-shaft angle value [degrees] | 134.16 (SD = 6.00) | 118.00 | 149.00 |
Table III
Number of patients in individual groups (p = 0.005 in two-sided probability test)
Discussion
The available databases lack studies which evaluate the reproduction of the FO according to the neck-shaft angle using a standard prosthesis stem in partial hip arthroplasty. One of the most important reasons for addressing the topic is the lack of knowledge in this area of orthopaedics.
Femoral offset represents the simplified length of the biomechanical lever arm of the abductor muscles. Inadequate FO reconstruction after total hip arthroplasty (THA) is associated with an increased risk of postoperative dislocation, limping, leg-length discrepancy and component wear, as well as impingement-free range of motion [4].
There are some recent papers describing FO restoration in patients treated with bipolar hip arthroplasty (BHA) due to displaced femoral neck fracture and its influence on clinical outcome [4–7].
Ji et al. [5] stated that when performing partial hip arthroplasty with a Smith & Nephew standard angle stem (neck-shaft angle 131 degrees), 23% of patients whose FO changed by more than 20% of the preoperative value did not have a properly restored FO which significantly worsens the outcomes of the Harris Hip Score (HHS) and Modified Barthel Index (MBI).
Kim et al. [6] retrospectively analysed a group of 77 patients who underwent BHA due to FNF. As a result of the surgery, both FO and leg length were increased. The researchers revealed a negative relationship between FO restoration and HHS during the entire follow-up period.
In the study by Buecking et al. [4] the authors focused on clinical outcomes such as HHS, timed up and go (TUG) and Lawton Instrumental Activities of Daily Living (IADL) and found a significant positive correlation between FO and HHS and IADL. The authors noted a linear relationship and excellent correlation between postoperative FO and the contralateral FO. It is worth noting that most likely the perfect correlation is the result of preoperative planning resulting in more frequent use of a lateral stem rather than a standard one.
With regard to the clinical outcome after bipolar hip arthroplasty, Kizkapan et al. [7] evaluated factors affecting the risk of dislocation after BHA. According to the authors, decreased FO on the operated side and larger neck-shaft angle (more valgus hip) on the non-operative side significantly raise the risk of dislocation.
It is noteworthy that the survey was conducted among patients burdened with a very high risk of dislocation (8.6%). This may be a result of the selected surgical access – all patients were operated on from a posterior approach. It is stated that the mentioned approach is associated with an increased risk of dislocation [8, 9].
In our study, all patients were operated on from an anterolateral approach. However, unfortunately, due to the lack of follow-up, we do not have data on the occurrence of prosthetic dislocations in the study group.
Unfortunately, none of the articles checked the correlation between stem neck-shaft angle and preoperative patients’ neck-shaft angle. The present study focused precisely on the values of angles and the possibility of the most accurate restoration of FO, but it is not a typical clinical study with an assessment of the functioning of patients. There was no follow-up and the outcomes were not checked with the questionnaires used in the above studies [4–7]; therefore the authors cannot refer to the mentioned studies in these matters.
Thus, taking into account the results of articles mentioned above [4–7], it seems that restoring FO with meticulous templating in patients undergoing bipolar hip arthroplasty due to femoral neck fracture is essential.
There are several articles that have focused on the assessment of abductor muscle strength depending on the reconstructed FO after total hip arthroplasty [10, 11]. Tezuka et al. [10] examined changes in the hip joint centre (HJC) and FO during THA and their influence on the strength of abductor muscles. They concluded that the infero-medial cup position and hence the medial shift of the HJC and the compensating FO increase optimized hip abductor muscle strength. Such positioning and selection of implants also have a positive effect on the functioning of the patient [12].
In the study by Mahmood et al. [11], the authors divided 222 patients after THA in terms of reconstructed FO into those with reduced offset (shortening of more than 5 mm), with correct offset (within 5 mm restoration) and with increased offset (over 5 mm). Analysis of the results showed that patients with reduced offset had worse patient reported outcome measures and had statistically significantly lower abductor muscle strength.
In total hip arthroplasty, selecting the right FO in order to ensure good hip abductors tension depends on the position of the acetabulum, especially its depth in the medial lateral axis.
In the case of BHA where the HJC is not changed, it is important to recreate the FO as close as possible to the baseline to maintain proper abductor muscle strength and avoid patient’s limping and dissatisfaction with the procedure.
Incorrect reconstruction of the FO, especially increasing its value, may adversely affect the patient’s functioning [13, 14]. Although in the study by Weber et al. [13] the usage or simulation of the use of high offset stem increased the range of motion (ROM) in each case, increasing ROM in the hip joint improved the patient’s functioning in activities of daily living only in less than 10% of patients. Therefore, the authors emphasize that each patient should have the FO reconstructed individually.
Liebs et al. [14] divided patients after THA into three cohorts as in the study by Mahmood et al. [11] They revealed that the greater the postoperative FO, the worse the patient’s score on the pain subscale from the Western Ontario and McMaster Universities Arthritis Index (WOMAC) questionnaire.
However, another study by Foy et al. [15] analysed 157 patients in the context of lateral hip pain depending on the change in FO after THA. In contrast to the previous study, the authors did not detect a statistically significant correlation between the occurrence of lateral hip pain and the change in FO.
A condition that is worth mentioning in the discussion is called greater trochanteric pain syndrome. The most common manifestation of this disorder is chronic lateral hip pain, which is aggravated by weight bearing activities and side lying at night. In more developed and advanced stages it can present as weakness and Trendelenburg’s gait.
Onset of symptoms is related to, among other factors, the pathology of gluteus medius and/or gluteus minimus muscles and their tendons. Inflammation of bursae surrounding the greater trochanter is responsible for the minority of all cases of posterolateral hip pain. Soft tissue damage resulting from the surgical approach causes the majority of them. It seems that type of surgical approach has a greater impact on the occurrence of posterolateral hip pain than increased FO [3, 16, 17].
The present study analysed patients after BHA, unfortunately only with the use of standard neck-shaft angle stems. One question that may arise is whether lateralised stems could be used during BHA due to femoral neck fracture and what the survival of high offset stems would be in such patients. Some studies analysing the survivorship of high offset stems suggest that lateralized stems have shorter survival periods than standard stems [18, 19] or that high offset stems have a high risk of loosening and surgery failure [20].
Conversely, there are studies which indicate a very good survival time or predicted survivorship of high offset stems [21–24]. It seems to be a more complex and multifactorial issue, and it cannot be said with certainty that patients with a high offset stem during bipolar hip arthroplasty will require revision surgery in a shorter period of time.
Also positive for the topic discussed are the recent results presented by members of the Hip Fracture Evaluation with Alternatives of Total Hip Arthroplasty versus HemiArthroplasty (HEALTH) Investigators.
Namely, cooperating researchers presented the results of their international study which showed that the incidence of secondary procedures after total and partial hip arthroplasty (hemi-hip replacement) did not differ between the two group [25].
In this study the patients after THA presented modestly better function at 24 months, but as can be expected with a slightly higher incidence of serious adverse events than hemiarthroplasty patients with displaced femoral neck fractures.
Study limitations
The authors of this article admit that the study has some weaknesses. Firstly, no rotational correction was used during the measurements of the offsets. However, patients whose pelvis/lower limbs were too rotated, which prevented performing proper measurements, were excluded from further X-ray evaluation.
Secondly, it is a study that analyses only the radiological results of the performed operations, without taking into account the follow-up of patients or the patient reported outcome measurements.
Third, the operations were performed by several different surgeons, so there is a risk that the results will vary by operating surgeon.
This study, however, also has strengths. To the best of our knowledge, this is the first study, which aims to accurately check the correlation between the patients’ native neck-shaft angle and the postoperative change in FO.
Conclusions
Our study proved that it is sometimes hard to achieve FO within a safe range while performing partial hip arthroplasty in patients with coxa vara. The topic of using high offset stems in partial hip arthroplasty has not been thoroughly researched worldwide.
However, taking into account the results of our study, during a hip hemiprosthesis procedure due to femoral neck fracture, the neck-shaft angle of the healthy hip should be measured and the use of a high offset stem for varus hips should be considered in order to improve the clinical outcome of the treatment and improve the quality of life and functioning of the patient.
For these reasons, we hope that this publication will become an incentive for other orthopaedic clinical centres to conduct similar measurements and analyses among their own patient cohorts.





