Introduction
Psoriatic arthritis (PsA) is a chronic, immune-mediated disease characterized by musculoskeletal involvement, including arthritis, enthesitis, spondylitis, and dactylitis, which is commonly associated with psoriasis (PsO) [1]. Persistent inflammation may lead to joint destruction and disability, which might be prevented with early diagnosis and treatment [2]. Individuals with PsO who visit general practitioners or dermatologists may report joint-related symptoms. However, diagnosing PsA can be challenging for non-rheumatologists. This underscores the importance of having a reliable screening tool to identify patients who may require further evaluation by a rheumatologist. To facilitate earlier detection of PsA, several simple screening tools have been created.
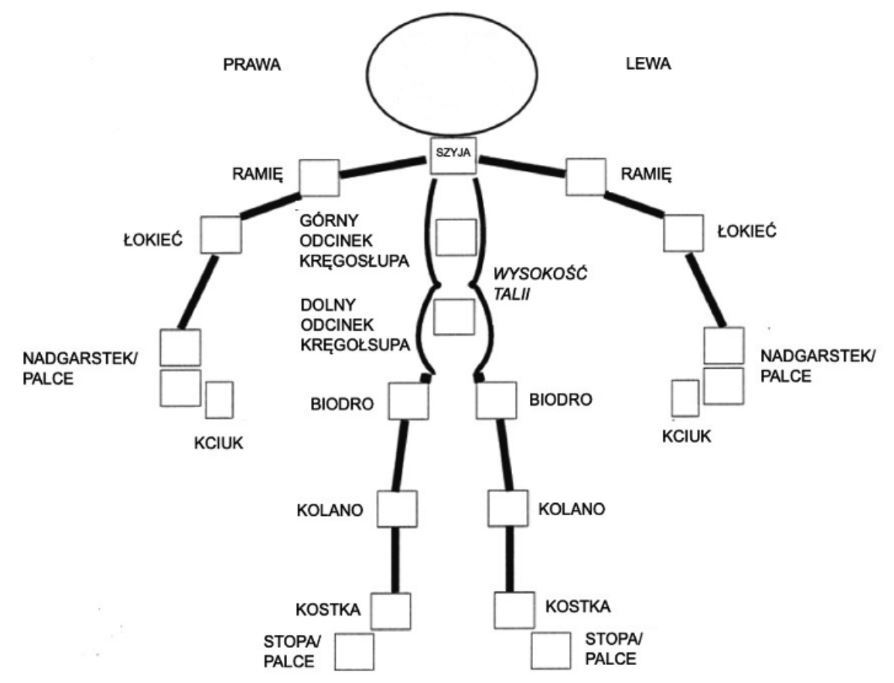
The Psoriasis Epidemiology Screening Tool (PEST) is a self-administered questionnaire consisting of 5 items, complemented by a figure for patients to mark areas of concern. PEST demonstrates a sensitivity of 92% and a specificity of 78% in patients with PsO. Each item in the questionnaire has a “Yes” or “No” answer, scored as 1 and 0 points, respectively. A total score of 3 points or higher indicates a positive result and suggests the need for further rheumatological evaluation. Although the manikin does not contribute to the discriminative ability of the questionnaire, it enables the physician to quickly identify affected joints. The figure does not enhance the diagnostic accuracy of the questionnaire; however, it provides valuable information for clinicians to efficiently identify affected joints, thereby facilitating the referral process when indicated [3]. Another tool, designed for early detection of PsA, is Early Arthritis for Psoriatic Patients (EARP), a straightforward 10-item questionnaire with a sensitivity of 85% and a high specificity of 92%. The EARP questionnaire includes questions about joint pain, stiffness, swelling, lower back pain, and other related signs. Each question has a “Yes” or “No” answer, scored as 1 and 0, respectively. The total score is calculated by summing positive answers, with a score of 3 points or higher indicating the need for further rheumatological evaluation. For patients scoring below 3 points but with persistent or worsening symptoms, it is recommended to consider reevaluating with EARP or consulting a specialist [4]. Until now, none of these tools has been officially available to the Polish population. The objective of this study was to translate and further validate the PEST and EARP questionnaires, creating a Polish-language version as a screening tool for identifying individuals with PsA in the Polish population.
Material and methods
Translation and validation
The Polish translations of the EARP and PEST questionnaires were carried out according to the international guidelines [5, 6]. Initially, two independent forward translations for each questionnaire were prepared (P.K.K., K.M.T.). Then, the final, unified version was created by a third, independent consultant (J.C.S.), a PsA expert fluent in both Polish and English, to resolve any discrepancies between the translations. The next step involved creating two separate back translations of the harmonized Polish versions of both questionnaires (A.Z., P.W.). None of the translators was familiar with the original versions of the questionnaires. These English versions were presented to a member of the original questionnaire development team, who accepted the translations without further modifications, ensuring the accuracy of the final Polish versions of the EARP and PEST questionnaires. Cognitive debriefing was conducted with eight participants, consisting of 4 females and 4 males diagnosed with PsA. Participants were asked to provide suggestions for improving the clarity and understandability of the questions and answer categories in both questionnaires. After the translation, Polish versions of the EARP and PEST questionnaires were validated as follows.
The Polish versions of the EARP and PEST questionnaires were distributed to 45 adult patients diagnosed with PsA according to the 2006 Classification Criteria for Psoriatic Arthritis. Data were collected from three different clinical centers – the Department of Rheumatology and Immunology in Krakow; the Department of Rheumatology and Systemic Connective Tissue Diseases in Warsaw; and the Department of Rheumatology and Internal Diseases in Wroclaw – with 15 patients from each center. The study group included 20 females and 25 males, 19 to 73 years (mean age: 49.16 ±12.62 years). All participants were asked to complete the Polish versions of the EARP and PEST questionnaires twice, with the second completion occurring 3–5 days after the first. This interval enables a similar clinical state to be maintained and is sufficiently long to prevent participants from recalling their previous responses.
Statistical analysis
The statistical analysis of the obtained data was conducted using IBM SPSS Statistics v. 26 (IBM Corp, USA). The internal consistency of both questionnaires was assessed with the Cronbach’s α coefficient, where a coefficient of at least 0.7 is considered indicative of internal consistency [7]. The reproducibility (test-retest reliability) of each questionnaire was evaluated by comparing each patient’s two sets of responses using the intraclass correlation coefficient (ICC). To demonstrate adequate reproducibility, the ICC, like the Cronbach’s α coefficient, should also be at least 0.7 [8]. The correlation between individual items from the first and second completions was analyzed separately for each questionnaire using a Wilcoxon signed-rank test. The Spearman correlation coefficient was used for correlations between the validated questionnaires. A 2-sided p-value of ≤ 0.05 was statistically significant.
Results
The analysis of internal consistency of the Polish language versions of PEST and EARP indicated that the individual items from the questionnaires were correlated with one another. Cronbach’s α coefficient value for the PEST total score was 0.712, and for the EARP total score was 0.771, which indicated an adequate internal consistency of each of the translated questionnaires.
The reproducibility of the studied questionnaire, determined using the ICC, was 0.731 for PEST and 0.730 for EARP (Tables I, II). No statistically significant differences were found between the answers for each question obtained after completing the questionnaire twice (3–5 days’ interval).
Table I
Psoriasis Epidemiology Screening Tool – reproducibility of the results
Table II
Early Arthritis for Psoriatic Patients – reproducibility of the results
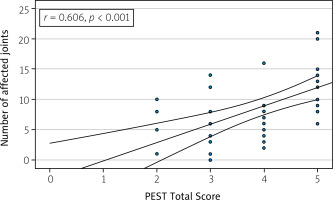
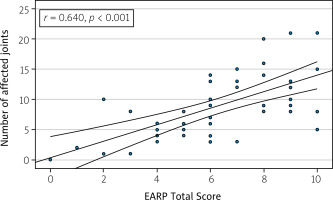
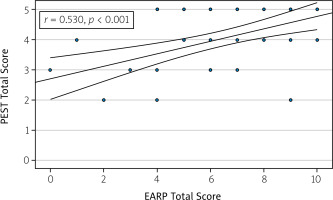
The correlation analysis indicates moderate to strong positive relationships between the total scores of PEST and EARP (Fig. 1), as well as between these scores and the number of affected joints (Figs. 2 and 3). Specifically, the PEST total score from the first assessment shows a moderate positive correlation with both the number of affected joints (r = 0.606, p < 0.001) (Fig. 2) and the EARP total score (r = 0.530, p < 0.001) (Fig. 1). Additionally, a strong positive correlation is observed between the number of affected joints and the EARP total score (r = 0.640, p < 0.001) (Fig. 3).
Fig. 1
Psoriasis Epidemiology Screening Tool Total Score and Early Arthritis for Psoriatic Patients Total Score correlation.
The Polish validated versions of PEST and EARP are presented in Figures 4 and 5. The original versions are available in the supplementary file (Suppl. Figs. 1 and 2).
Discussion
Psoriatic arthritis is a chronic inflammatory condition characterized by joint damage and disability [1, 9]. Research indicates that up to 30% of individuals with PsO develop PsA, typically within 10 years of the initial appearance of skin symptoms. Studies suggest that between 5% and 15.5% of PsO patients may have undiagnosed PsA. Even a 6-month delay in diagnosis after symptom onset has been associated with joint damage and poorer long-term physical function [10].
A multidisciplinary approach involving primary care physicians, dermatologists, and rheumatologists is essential for improving the early detection and diagnosis of PsA [11, 12]. Factors such as the severity of PsO, specific locations of skin lesions (e.g., scalp, nails, intergluteal area), and the presence of certain biomarkers or genetic predispositions may indicate a higher risk of joint involvement [13–16].
To support earlier detection, several simple and validated screening tools have been developed, including the EARP questionnaire [4], the Psoriatic Arthritis Screening and Evaluation (PASE) tool [17], PEST [3], the Psoriatic Arthritis Uncluttered Screening Evaluation questionnaire [18], and the Toronto Psoriatic Arthritis Screen (ToPAS) [19]. Despite their demonstrated utility, these tools remain underutilized in clinical settings [20].
Experts emphasize the importance of early referral to rheumatologists for PsA patients. Approximately two-thirds of patients with PsA diagnosis present with at least one joint erosion at their first rheumatology consultation [20, 21]. Late referrals are associated with worse functional outcomes, as measured by Health Assessment Questionnaire scores [22]. Moreover, a proactive approach to managing newly diagnosed PsA, incorporating regular reviews and treatment adjustments every 4 weeks, has been shown to significantly improve joint health outcomes [23].
In 2021, Urruticoechea-Arana et al. [20] published a systematic review that, among other objectives, compiled studies comparing various early PsA screening tools within the same population. The study found that PEST and EARP demonstrated slightly better performance compared to other commonly used questionnaires, such as PASE and ToPAS [20]. Therefore, they were considered for the current project.
In 2024, Biln et al. [24] published the results of a study aimed at identifying existing triage approaches for referring patients with suspected inflammatory arthritis from primary care physicians to rheumatologists. Using a comprehensive search strategy across multiple international databases, the authors included 53 studies. They highlighted several tools – including the Early Inflammatory Arthritis Questionnaire, the Case Finding Axial Spondyloarthritis tool, and PEST – that have the potential to improve current referral processes [24].
Early Arthritis for Psoriatic Patients has been used in multiple languages, including Italian (authors of original questionnaire) [4], Thai [25], Japanese [26], Spanish [27], Hebrew [28], and Dutch [29]. Notably, the Japanese version [26] demonstrated very high sensitivity and specificity, both 97.2%, indicating excellent diagnostic accuracy. The Thai version of EARP [25] also showed good performance, with a sensitivity of 83% and specificity of 79.3%, making it effective in its target population. Similarly, PEST has been translated into Thai [25], Portuguese [30], Italian [31], Spanish [27], Hebrew [28], and Dutch [29]. As in the case of EARP, the process of translation and validation was not described in every case mentioned. The Portuguese and Thai versions reported high levels of internal consistency (Cronbach’s α of 0.90) and good diagnostic performance. Sensitivity and specificity varied across studies, with reported ranges of 72–92% and 78–89.7%, respectively. This variability highlights the importance of adapting the questionnaires to the linguistic and cultural nuances of each region [20].
Comparisons between EARP and PEST in the same populations revealed variable performance levels. For example, EARP often demonstrated higher sensitivity, making it suitable for identifying more cases of PsA, while PEST offered higher specificity, reducing the likelihood of false positives. Studies suggest that EARP may be better suited for populations with a higher prevalence of PsA, whereas PEST is advantageous in settings where over-referral needs to be minimized [20].
Our study presents the successful translation and validation of the Polish versions of the PEST and EARP questionnaires, offering effective and accessible screening options for PsA in Polish clinical settings. The findings confirm that the Polish versions of both questionnaires retain strong psychometric properties, demonstrating adequate reliability, validity, and reproducibility, which supports their potential use in routine screening for PsA among PsO patients.
Study limitations
Despite these promising results, the study has certain limitations such as absence of convergent validity, primarily due to the lack of other validated Polish screening instruments. Moreover, the sample size, while sufficient for initial validation, restricts the generalizability of the findings to broader and more diverse populations. Additionally, a longitudinal approach could provide insights into the predictive accuracy of PEST and EARP over time, offering further validation of their effectiveness in screening.
Conclusions
The Polish versions of the PEST and EARP questionnaires are reliable and validated tools for PsA screening, facilitating early referral to rheumatology and optimizing patient care outcomes. This study lays the groundwork for integrating these tools into routine dermatologic and general practice in Poland, fostering earlier diagnosis and improved management of PsA in individuals with PsO.