Introduction
Pyoderma gangrenosum (PG) is a rare disease characterized by aseptic inflammation and non-healing, ulcerative skin lesions. Pathergy – a phenomenon of development of excessive skin ulcers after even minor injury or surgical intervention occurs in 25–50% of cases [1]. The abnormal immune system reaction leading to neutrophil activation and migration is a postulated essential pathomechanism [2].
Pyoderma gangrenosum may coexist with autoimmune disorders such as inflammatory bowel diseases. The clinical presentation is very diverse, and diagnosis can be challenging in many cases. The diagnosis of PG relies on the exclusion of other pathologies since there are no specific serological markers, and the histopathology is variable and ambiguous [3–5].
Systemic glucocorticosteroids (GCs) and cyclosporine A (CsA) are the primary therapies, but several studies have reported successful outcomes with other immunosuppressive drugs. Due to the scarcity of controlled trials, proposed treatment regimens are based on expert opinions, case series, and case reports [6–8].
The presented case description of a 79-year-old woman who developed chronic PG after open reduction and internal fixation of a distal radius fracture (DRF) with a titanium plate was the reason for a more extensive discussion of this rare complication and a review of the literature on the subject. According to our best knowledge, it is the first reported PG case after DRF surgery.
Methods of the literature review
In the first step, Web of Science and Medline databases were queried for general information on pyoderma gangrenosum, including pathomechanism, presentation, diagnostic criteria, and treatment methods. The keyword “pyoderma gangrenosum” was used, and randomized controlled studies, systematic reviews, and consensus reports were only considered at this step. In the second step, Web of Science and Medline databases were queried using the keywords “pyoderma gangrenosum” and “orthopedics” to find exhaustively described cases of pyoderma gangrenosum after orthopedic surgery. The cases were analyzed, and an essential description of them was placed in Table I to present a variety of clinical presentations of this rare condition. Reviews of cases without presenting a new case were removed from the analysis.
Table I
Overview of the reported cases of pyoderma gangrenosum after orthopedic surgery
| Author | Patient | Medical history | Type of surgery | Clinical presentation summary | Primarily suspected and treated for infection | Reported treatment and outcome |
|---|---|---|---|---|---|---|
| Armstrong et al. 1999 [17] | Male, 69 years old | Skin healing complication requiring skin grafting after a dog bite one year before | THA | Wound healing complication – a large area of ulceration and necrosis starting two days after THA | + | Spontaneous healing after administration of 40 mg/day of prednisolone along with minor debridement and local and systemic antibiotics; 11 weeks to fully heal the wound |
| Attar et al. 2010 [18] | Female, 80 years old | – | TKA | Wound dehiscence and ulceration after bilateral TKA Antibiotics and debridement provided no improvement | + | Improvement after systemic GCs |
| Reid et al. 2014 [19] | Male, 55 years old | – | Elective rotator cuff and Bankart repair | Discharge from the wound 10 days after elective rotator cuff and Bankart repair Treated as infection, with multiple surgical debridements with no improvement Further deterioration to devasting myositis and myonecrosis of the left half of the thorax with hemodynamic insufficiency | + | High-dose systemic GCs gave dramatic improvement, defect covered with free and rotational flap autograft. Internal fixation necessary Full recovery |
| Hackl et al. 2015 [20] | Female, 33 years old | N/D | Tibial nailing | Wound healing complication after tibial fracture closed reduction with internal nail fixation | + | Systemic GCs, CsA then azathioprine provided significant improvement Wound closure with skin flaps |
| Burnett et al. 2015 [21] | Male, 76 years old | Atrial fibrillation | THA | Expanding ulcerative lesions at the surgical site after revision hip arthroplasty | + | IV antibiotics, surgical debridement and NPWT provided full healing No systemic treatment for PG |
| Nizamoglu 2015 [22] | Male, 82 years old | Hypertension, benign prostatic hypertrophy, myocardial infarction 16 years prior, atrial fibrillation, cardiac defibrillator | Dynamic hip screw | Erythema and purulent discharge from the wound 10 days after proximal femur fracture stabilization with a dynamic hip screw Primarily treated as infection with debridement with no improvement | + | Improvement in the wound site after prednisolone administration 1 mg/kg/day Death 30 days after surgery because of bronchopneumonia |
| Giugale et al. 2018 [23] | Female, 51 years old | Type 2 diabetes mellitus, depression, anxiety, giant cell tumor of the tendon sheath in hand excised with no complications | Carpal tunnel decompression | Erythema and wound drainage 5 days after open carpal tunnel decompression Treated for suspected infection with multiple debridements and irrigation with no improvement Deteriorating over time | + | High-dose prednisolone regimen provided excellent improvement Wounds healed by 2 months |
| Yik et al. 2015 [24] | Male, 56 years old | N/D | TKA | Wound healing complications starting 6 days after TKA Treated for suspected infection with NPWT and multiple debridements with no improvement | + | Improvement after prednisone 0.5 mg/kg/day Wound closed successfully with skin flap and graft |
| Berger et al. 2017 [25] | Male, 13 years old | Lip swelling after dental surgery under general anesthesia | Hip reconstruction | Boy treated for Perthes disease with subtrochanteric osteotomy Four days after surgery, dehiscence of the postoperative wound, gradually deteriorating Suspected for necrotizing fasciitis Primary treated with antibiotics, hyperbaric oxygen chamber and implant replacement. Hemodynamic complications | + | Sudden improvement of general condition after i.v. cortisone The wound and bones healed by secondary intention by 6 weeks after surgery |
| Ratliff 2019 [26] | Female, 68 years old | Osteoarthritis, inflammatory bowel disease, dyslipidemia, deep vein thrombosis in left leg, hypertension, lower gastrointestinal bleeding, obesity, scoliosis, spinal stenosis | Spine fusion | Four weeks after T4–T10 fusion due to broken rods at L5–S1 wound opening around a stich Deteriorating gradually VAC therapy and debridement for suspected infection with no improvement Additional lesion on the forearm | + | Improvement on prednisone tapered therapy Full healing by 3 weeks |
| Franklin et al. 2020 [27] | Male, 71 years old | Smoking, alcohol overuse, bilateral THA, right THA complicated with infection | Proximal humerus plating | Seven days after open reduction and internal fixation with a plate for proximal humerus fracture erythema of the wound Multiple debridements with no improvement Wound deteriorating Additional lesion appeared on the left thigh | + | Prednisolone 60 mg/day provided full wound healing |
| Bates et al. 2021 [28] | Male, 35 years old | – | Knee arthroscopy | Arthroscopy and screw fixation of medial femoral condyle osteochondral lesion Eight days after surgery edema and erythema deteriorating to pustules and ulcerations at the site of surgical incision Additional lesions in the inguinal site Debridements and antibiotics with no improvement | + | Initial methylprednisolone and then tapered oral prednisone therapy provided fast improvement Wound closed with gastrocnemius flap |
| de Thomasson Caux, 2010 [29] | Female, 65 years old | Previous operations for adenocarcinoma of colon and pancreas without complications | THA | Wound healing complication after THA | + | Improvement after systemic prednisone 1 mg/kg/day, complete heal after 6 weeks |
| Hoelscher et al. 2020 [30] | Male, 60 years old | Fibromyalgia, alcoholism, inflammatory bowel disease | Lower extremity internal and external fixation | Multitrauma patient, treated with external and internal fixation for lower extremity fractures One week after surgery, discharge and erythema on traumatized skin, fever Primarily treated for infection with no improvement | + | Systemic high-dose GCs, topical dapsone, skin flaps for wound closure Wounds healed by 1 year |
| Bellamy, Ananthakrishnan 2021 [31] | Male, 65 years old | Hyperlipidemia, skin cancer, myotonic dystrophy | Spine fusion | Nine days after T4-sacral instrumented fusion drainage from the wound and fever Treated for infection with NPWT, irrigation and debridement, and antibiotics with no improvement | + | Dapsone, then methylprednisolone and CsA with improvement Wound coverage by flaps Adalimumab for maintenance Fully healed within 1 year |
| Mizushima 2021 [32] | Female, 69 years old | Myelodysplastic syndrome, Basedow disease | THA | THA for arthritis, with granulocyte colonystimulating factor as prevention of infection from MDS Seven days after surgery, wound healing complication Previously treated as infection with antibiotics | + | Tapered prednisolone regimen starting from 60 mg/day with improvement Fully healed within 2 months |
| Loomis et al. 2021 [33] | Male, 62 years old | Hypertension, hyperlipidemia, atrial fibrillation | TKA | Wound healing complication after bilateral TKA starting one week after surgery | + | Successful healing after oral GCs and combined skin and skin substitute (Integra) grafting Fully healed after 12 months |
| Suarez et al. 2011 [34] | Male, 81 years old | Myelodysplastic syndrome | Proximal femoral nail | Wound healing complications starting 3 days after gamma nail for peritrochanteric fracture Reoperation – lavage, empirical antibiotics empirically without improvement | + | Complete healing after 4 weeks from starting prednisone 1 mg/kg/day (15 days of therapy) |
| Nakajima et al. 2011 [35] | Female 80 years old | Type 2 diabetes mellitus | TKA | Wound healing complication starting 5 days after TKA Surgical debridement without improvement | + | Improvement after 20 mg/day of prednisolone and 100 mg/day of CsA The wound healed 3 months after skin grafting |
| Bagouri et al. 2012 [36] | Male, 33 years old | Ulcerative colitis that exacerbated during reported PG outbreak | ACL reconstruction | Wound healing complication starting 4 days after arthroscopically assisted anterior cruciate ligament reconstruction Several surgical debridements failed to improve | + | Full healing of the wound with intact ACL graft after administration of high-dose oral GCs |
| Wanich et al. 2012 [37] | Male, 51 years old | suspicion of Behçet disease | Repair of the patellar tendon | Wound healing complication starting 10 days after open repair of patellar tendon injury Empirical antibiotics failed to improve | + | Prednisone 60 mg/2 times per day and dapsone 50 mg/day later reduced provided successful healing after 12 weeks |
| Grollmus, de Retana 2013 [38] | Female, 48 years old | – | Ankle surgery | Wound healing complications starting within a week after ankle arthroscopy, debridement, microfractures, flexor digitorum longus transfer and medial slide calcaneal osteotomy Debridement of necrotic skin tissue and antibiotics failed to improve | + | Improvement after prednisone 2 mg/kg/day, after one month, wounds fully healed |
| Fang et al. 2013 [39] | Female, 74 years old | Several miscarriages, repetitive thrombosis, severe wound complication following cholecystectomy 20 years before | Ankle surgery | Wound healing complication 3 days after midfoot fusion and Achilles tendon reconstruction Primarily treated as infection with NPWT therapy and cefuroxime then latissimus dorsi flap transfer Pyoderma gangrenosum lesions outbreak also in the graft donor site and abdomen when LMWH was given | + | Below-knee-amputation Prednisone 100 mg per day and polyclonal immunoglobulin 20 g/day for 5 days Successful healing of the stump, without relapse within a year |
Case description
A 79-year-old woman with hypertension, ischemic heart disease, and Hashimoto’s disease sustained a closed fracture of the left distal radius due to a fall from patient’s height. The patient underwent closed reduction and immobilization in a plaster cast. Because of secondary displacement, eight weeks later, patient received open reduction and stabilization with a volar titanium locking plate and screws. After surgery, the patient suffered from severe pain and edema, but ultrasound showed no pathology related to the performed operation, and the symptoms relieved spontaneously.
After a 2.5-year asymptomatic period, the patient reported pain and edema of patient’s left wrist. The radiograph showed the loosening of one screw, causing conflict with soft tissues. We removed the implant, but we also found serous masses penetrating the surrounding tendon sheaths. Microbiological cultures revealed no pathogens; tuberculosis was excluded as well. Due to suspected infection, the patient empirically received clindamycin and ciprofloxacin.
One month after the implant removal, the surgical wound presented as ulceration with fistulae and purulent discharge (Fig. 1); radiographs revealed osteolysis within the styloid process of the radius. Despite many negative microbiological cultures, we still suspected infection as the most probable cause. We performed debridement of the lesion with application of local antibiotic carrier gentamicin beads and collagen gentamicin sponge with the addition of 1 g of cefazolin and 1 g of vancomycin. Negative pressure wound therapy (NPWT) to improve wound healing followed the surgery. After two weeks, wound healing was satisfactory.
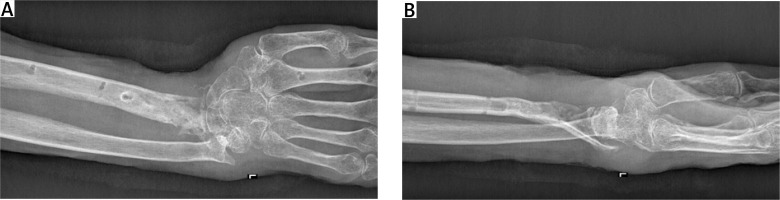
After another month, radiographs showed a pathologic fracture in the site of the previously treated osteolytic bone defect and screw canals. We performed external fixation with wrist canal decompression and local administration of gentamicin beads again. The wound healing was slow and microbiological cultures revealed Enterococcus faecalis. Targeted antimicrobial therapy with levofloxacin resulted in only partial improvement. As new purulent skin lesions appeared, we took skin and bone biopsies (Fig. 2).
Fig. 2
External fixation for pathologic fracture in the site of the bone defect. PG was diagnosed at that moment.

Histopathology of the bone was unspecific, but excessive numbers of neutrophils and plasmacytes were found in the skin. Radiographs showed a progressing deformation of the wrist and osteomyelitis (Fig. 3 A, B). After exclusion of plasmacytoma and other hematologic conditions, PG was diagnosed.
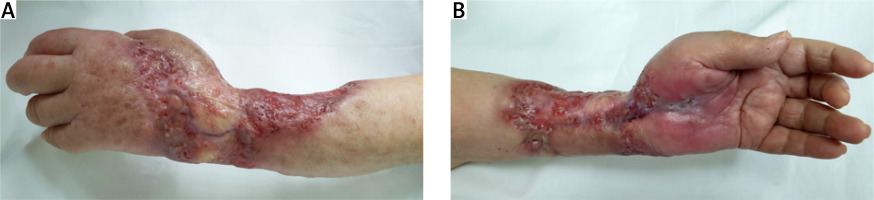
The introduction of immunosuppressive treatment with prednisone and CsA gave excellent clinical effects. Unfortunately, every attempt to reduce the prednisone dose below 20 mg/day led to the lesion’s recurrence despite concurrent CsA treatment with an adequate trough level of 100–130 ng/ml. Given the poor patient tolerance of the treatment and two episodes of superinfection, the immunologic treatment was not continuous, leading to a massive PG relapse (Fig. 4 A, B).
Fig. 4
A, B. Massive relapse of PG at the site of scars from healed previous lesions. Note edema of the hand because of clenched and damaged veins.
Severe pain, deformation of the extremity, and function alteration were the reasons for amputation of the proximal 1/3 of the forearm. The immunosuppressive treatment was discontinued after surgery because of the risk of infection. The wound healing was primarily good, but PG lesions relapsed in the stump after several weeks. Magnetic resonance showed fistulae and edema in soft tissues and osteomyelitis in forearm bones, but the culture from the wound was negative. Immunosuppressive treatment was started again, with an initially good response. Unfortunately, a massive relapse of ulcers occurred after decreasing the prednisone dose below 10 mg/day.
The next half of a year of local and systemic treatment did not succeed, which ultimately led to exarticulation in the scapulohumeral joint. At this point in time, 6 years had already passed since the primary fracture. The wound healing was good, but immediately after the surgery, the patient was diagnosed with COVID-19. High-resolution computed tomography scans showed that the viral inflammation affected 90% of both lungs. The patient was in a severe condition and required 6 mg/day of dexamethasone and high-flow oxygen therapy (40 l/min 100% O2). Five days later, when patient’s condition improved, oxygen supplementation was limited and ultimately ended after 10 days.
After two weeks, the patient was discharged home on prednisone 30 mg/day. The prednisone dose was gradually reduced and withdrawn after 8 months.
There was a relapse of PG one year after disarticulation – a purulent ulcer with morphology typical for PG in the postoperative scar. After a return to prednisone therapy, the ulcer healed completely. Now, every attempt to reduce prednisone dose below 30 mg/day results in a relapse of PG lesions, making the patient GC-dependent. Currently, the 85-year-old patient is suffering from iatrogenic Cushing syndrome, with kidney failure and fatigue as the most prominent symptoms. We are applying local GCs to avoid increasing the dose of systemic GCs.
Ethical standards: The written consent of the patient for publishing the case report was obtained.
Discussion
The exact causes of PG remain unknown. Dysfunction of neutrophils with increased local secretion of interleukin 8 and interleukin 16 promoting excessive chemotaxis is the probable explanation [2, 9]. The coexistence of PG and other immunological conditions like inflammatory bowel diseases is also noted [1, 2].
Even though 5 types of the disease are distinguished – ulcerative (the most common), pustular, bullous, peristomal, and vegetative – the clinical presentation of PG is various and the histopathologic findings are nonspecific, making this disease especially difficult to identify [1]. The diagnosis is always based on clinical presentation because there are no specific findings in histopathology or other tests that could be considered pathognomonic. It is vital that before making a diagnosis of PG, other infection mimicking conditions, such as vasculitis, vascular occlusive or venous disease, skin cancer, infection, or drug reaction, are excluded.
There are 3 systems of criteria – Mayo, Delphi Consensus, and PARACELSUS-score, among which the latter appears to be the most valuable [10].
In the case of our patient, all three major criteria of the PARACELSUS-score were fulfilled, i.e. progressive course of the disease, absence of relevant differential diagnosis and reddish-violaceous wound border, two minor criteria, i.e. alleviation after immunosuppressive therapy and extreme pain (VAS > 4), and one additional criterion: undermined wound border. The total of 14 points out of 20 possible indicated PG as the most reliable diagnosis, with the threshold set at 10 points.
There is a minimal number of reported cases of osteomyelitis in the course of PG. Most of them were in pediatric patients and only 2 in adults – both were after their 70s, like the patient presented here [11–13].
The precise pathological processes linking the disease of bones with lesions on the skin are unknown, and we are not able to state whether the destabilized implant screw irritated the soft tissues leading to PG or if PG was the primary cause of bone disease leading to implant loosening. We can only say that aseptic osteomyelitis, unresponsive to locally administered antibiotics, of the distal radius, and later the first wrist row was present along with skin PG.
During the active phase of PG, surgical interventions at the disease site should be generally avoided. Debridement and local antibiotic administration before starting immunosuppressive therapy can be counter-effective since they activate pathergy and aggravate the disease [14].
There is no established consensus on treatment regimens, but GCs and CsA remain the most often used drugs. Inhibitors of tumor necrosis factor α and antagonists of interleukins of the inflammatory cascade can also serve as additional treatment options. Several clinical trials are also underway to test the usefulness of other drugs [8]. In the single-blind, randomized STOP GAP trial, treatment with prednisolone (initial dose 0.75 mg/kg per day) showed a similar rate of improvement compared to patients assigned to CsA (initial dose 4 mg/kg per day) [15].
We believe that satisfactory healing of the wound after arm exarticulation was possible thanks to immunosuppressive therapy, used for the whole pre-and postoperative period and clear surgical margins, far from tissues affected by PG. However, since complete ulcer healing may take several months, the patient can suffer from significant adverse effects of long-term systemic GCs. In the present case, decreasing the prednisone dose too quickly was the main factor in a relapse of PG despite concomitant CsA treatment. Available studies do not make it possible to claim that immunosuppressive therapy worsened the course of COVID-19 in our patient [16].
The review of reported PG cases after orthopedic surgery (Table I) shows that infection was a primary diagnosis in all reported patients [17–39]. Ineffective antibiotic therapy and irrigation and debridement were performed before the correct diagnosis of PG. Hence this type of treatment even deteriorates the course of PG. Other authors, as we also do, highlight the need to actively seek PG in the case of sterile wound healing complications [7, 19, 21–33, 35–39]. Glucocorticosteroids were the most commonly used immunosuppressive, effective part of the regimens for postoperative PG treatment [17–20, 22–39].
Our review and the described case also show that even if lower extremities are the most common site for PG lesions, the disease can also affect other regions, even at a distance from the surgical incision [19, 23, 26, 27, 31]. In the reviewed cases coexistent inflammatory bowel disease was prevalent, which is consistent with findings from unselected patient groups [26, 30, 36].
Last but not least, our review shows how different a course of postoperative PG can be, affecting people of different ages and sexes. What distinguishes our patient from other reports is the very long course of the disease and frequent relapses when tapering the doses of GCs.
Conclusions
Based on the presented clinical case, experience and conducted literature review, we propose that every condition of non-healing wounds and ulcers with negative microbiological cultures and unresponsive to antibiotics should be checked for PG.
Treatment of PG in orthopedic patients is challenging and requires a multidisciplinary approach, involving a surgeon, dermatologist, and an experienced immunologist.
Most surgical interventions at the site of the PG symptoms should be avoided.
Long-term immunosuppressive therapy controlling the course of PG may be challenging for both patient and physician because of severe side effects.