Introduction
Rheumatic diseases remain among the most common pathologies in the world, the first among which is rheumatoid arthritis (RA) – this autoimmune disease affects about 1% of the general population (in Ukraine – 0.4%, in Europe and North America – from 1 to 2%) [1].
Lyme arthritis (LA), which is accompanied by an intense inflammatory process in the joints, is also important in rheumatology. Chronic pain and loss of physical function are the most serious consequences of the inflammatory process in the joints and have a great impact on various areas of human life [2].
The criteria for effective treatment in world medical practice is the duration and quality of life of patients [3]. Ineffective or non-targeted treatment leads to deformation and destruction of the joints and limitations of social, physical, and mental functioning [4–6].
Currently, the influence of RA on patients’ everyday routine is still very high despite more effective treatments [7]. Rheumatoid arthritis and complications of this serious disease cause extremely poor quality of life of patients [7]. And the long search for the cause of the infectious nature of arthritis, the delay in examination for borreliosis in an atypical course of arthritic syndrome [8], leads to difficulties in early diagnosis of Lyme disease (LD) and timely initiation of aetiotropic treatment [9].
The changes in the patient’s personality, which occur during the first year of life of patients since diagnosis, have a significant influence over the disease on RA [10]. Early detection of the disease and prevention of disabi- lity largely depends on timely and adequate treatment aimed at achieving remission of the disease [11–13].
To maintain long-term remission in pharmacological and non-pharmacological ways is attempted to restore function in the affected joints and improve the physical and mental functioning of patients [14]. An important aspect and consequence of arthritis is the growth of disablement and loss of efficiency.
Because the progression of the disease is unpredicta-ble, patients become anxious about the future, they become concerned about the growth of mobility limitations and the side effects of treatment. They have a fear of losing the opportunity for self-care, which negatively affects the self-awareness and all spheres of life of such patients [15].
Given the growing incidence of LD, it is important to further research the psychosocial factors associated with patients’ quality of life that affect the perception of the disease and the ability to cope with it [16].
Mac et al. [16] conducted a systematic literature review of quality of life of patients with LD in North America and Europe, included 46 studies, in 6 electronic databases, published between 1994 and 2019. Visual Analogue Scale (VAS) measures of joint pain, depression, fatigue, impairment of memory and concentration, and the ability to perform activities of daily living were significantly different (p < 0.05) for patients with LD than for controls, suggesting reduced quality of life and greater impairment for patients with LD [17].
On the example of the results of our own observations in the article, we see that the quality of life of patients with LA is worse due to severe joint pain and a greater degree of functional disorders compared to the patients with RA.
It was found that inflammation is considered a sign of depression [18]. A study of cytokine levels in peripheral blood before and after antidepressant treatment found that IL-10, IL-6, and IL-4 were considerably reduced during pharmacological therapy with antidepressants [19].
The severity of LD and the complications associated with it emphasize the need for a modern approach to treatment [20]. Today, the number of cases with a confirmed diagnosis of LD is growing rapidly in Europe and America [21].
Lyme disease is a complex immune-mediated dise-ase of infectious origin and inflammatory in nature [22, 23], in which 80–90% of the skin is affected as well as 10–20% of other organs [24]. In the absence of timely antibiotic therapy for LD, in more than 60% of patients LA developes – a late manifestation of the disease – which has symptoms of pain and swelling in the joints, similar to RA [25, 26], and it typically begins months after the initial tick exposure [27, 28].
The severity of the disease and the psychological disorder negatively affect the quality of life of patients with RA. It should be considered in the management of patients with RA to improve treatment standards [29].
Therefore, it was considered appropriate to estimate the functional state and life quality in patients with RA and LA according to the Health Assessment Questionnaire-Disability Index (HAQ-DI) and the 36-Item Short Form Survey (SF-36) questionnaires. The aim of this study is to stratify factors influencing quality of life in patients with RA and Lyme disease.
Material and methods
A survey of 90 patients, 36 males and 54 females, according to the SF-36 and HAQ-DI questionnaires was performed to evaluate their quality of life [30–33]. All studied patients had diagnosis of RA, but 44 (48.89%) also had confirmed Lyme disease. All studied patients were referred to the rheumatology clinic of Ternopil Regional Council “Ternopil University Hospital”.
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines and was approved by the local bioethics committee.
The diagnosis of RA was verified according to the American College of Rheumatology and the European League Against Rheumatism classification criteria (2010). According to the recommendations of the US Centers for Disease Control and Prevention, a two-stage diagnosis of Lyme borreliosis was performed: ELISA and Western blot. In the first stage, antibodies to Borrelia burgdorferi IgM and/or IgG were determined by ELISA.
The results were considered positive if IgM showed 2 out of 3 antigen bands – arthritis was considered acute and IgG – 5 bands out of 10 – arthritis was considered chronic. Intermediate and positive results of the first stage of the study in the second stage were confirmed by a specific immunoblotting test. In patients with RA the number of swollen joints was 10.64 ±3.25, and the number of painful joints was 12.31 ±2.78, while in patients with LA it was 5.34 ±2.47 and 4.08 ±3.27, respectively.
To assess disease activity inflammatory parameters such as erythrocyte sedimentation rate (ESR) (mm/h) and C-reactive protein (CRP) (g/l) were measured. The Visual Analogue Scale (0–100 mm) was used to assess the pain intensity (PI). The disease activity score with the examination of 28 joints (DAS28) is a tool for disease activity assessment, and it was measured as 4 components scoring with ESR.
Using the SF-36 questionnaire, scores were assessed on 8 scales: physical functioning, role-physical functioning, PI, bodily pain (BP), vital activity, general health (GH), social functioning, role emotional, and mental health, as well as calculated 2 components of health: mental (MCS) and physical (PCS) [28, 29].
Each scale took values from 0 to 100; the higher the value, the better the quality of life for this parameter. Assessment of the patient’s functional status was performed using a health questionnaire – HAQ-DI, which includes 20 questions that relate to the patient’s acti- vity in everyday life. The answers to the questions were evaluated on a scale from 0 to 3:
0 – no difficulty,
1 – with some difficulty,
2 – with much difficulty,
3 – unable to do.
The Health Assessment Questionnaire has 25 possible values. Values from 0 to 1.0 indicate minimal disorders of life, from 1.1 to 2.0 – moderate, and from 2.1 to 3.0 – severe disorder [30–33].
Statistical analysis
Statistical data processing was performed using Microsoft Office Excel 2010 and Statistica 10.0. Shapiro-Wilk criteria were used to check the normality of distribution in the samples. Significance of differences was assessed using the Mann-Whitney U test for nonparametric distribution and Student’s t-criteria for parametric distribution.
To analyse the direction and strength of the relationship between certain indicators the method of correlation analysis was used with the calculation of the correlation coefficients of Pearson in the normal distribution and Spearman – under deviations from the normal distribution. At p < 0.05, the differences in data were considered probably significant. Multiple regression evaluation was used to identify the most significant factors influencing the patients’ life quality.
Results
High and moderate RA activity was found in all patients who consented to take part in the study. Among patients, Borrelia burgdorferi was determined in 48.89%. Patients of both groups, with and without Borrelia burgdorferi, infection did not differ significantly in age and gender.
Patients who were infected with Borrelia burgdorferi showed a high degree of disease activity, while patients without infection had medium results in the DAS28. It should be noted that the intensity of pain assessed by VAS and inflammatory parameters ESR and CRP in the cohort of patients with LA were also higher than in the group with RA (Table I).
The analysis of functional status and quality of life of patients with RA and LA (Table I) showed a decrease in all scales in the SF-36 and HAQ-DI questionnaires, indicating a deterioration in the life quality in patients of both groups. Patients with LA have significantly lower scores on the MCS scale and all its components: mental health, vitality, role emotional, social activity, and physical functioning.
Table I
Clinical and laboratory parameters, and indicators of functional status and quality of life of patients with Lyme arthritis and rheumatoid arthritis
[i] BP – bodily pain, CRP – C-reactive protein, DAS28 – disease activity score with examination of 28 joints, ESR – erythrocyte sedimentation rate, GH – general health, HAQ-DI – Health Assessment Questionnaire-Disability Index, LA – Lyme arthritis, MCS – mental component of health, MH – mental health, PCS – physical component of health, PF – physical functioning, RA – rheumatoid arthritis, RE – role of emotional functioning, RPF – role of physical functioning, SF – social functioning, SF-36 – 36-Item Short Form Survey, VAS – Visual Analogue Scale, VT – vital activity, *p < 0.05 – reliable difference of indicators between groups of patients, **p > 0.05 – unreliable difference of indicators between groups of patients.
There was no significant difference in patients between physical function and role physical activity, but BP and GH in patients with LA were significantly different. Therefore, as a result, the PCS scale in patients with LA was lower, but a significant difference between this value in groups of patients was not found. In Table II correlations between PCS SF-36, MCS SF-36, HAQ-DI, and clinical manifestations of LA and RA are presented.
Table II
Correlations between Physical Component Summary scales 36-Item Short Form Survey, Mental Component Summary scale 36-Item Short Form Survey, Health Assessment Questionnaire-Disability Index, and clinical manifestations of the disease in patients with Lyme arthritis and rheumatoid arthritis
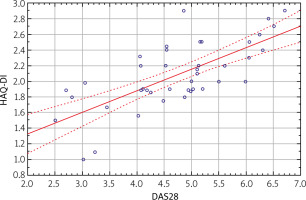
There was a direct firm correlation between the HAQ-DI and illness activity of patients with LA and a medium direct correlation in patients with RA, which is explained by a higher degree of functional disorders in patients with higher disease activity, which is presented in Figs. 1, 2.
Fig. 1
Health Assessment Questionnaire- Disability Index (HAQ-DI) scatter plot depending on the disease activity score with examination of 28 joints (DAS28) in patients with rheumatoid arthritis. Scatterplot of HAQ-DI against DAS28, HAQ-DI = 0.7787 + 0.2748*x; Conf.Int.
DAS28 – disease activity score with examination of 28 joints, HAQ-DI – Health Assessment Questionnaire-Disability Index.
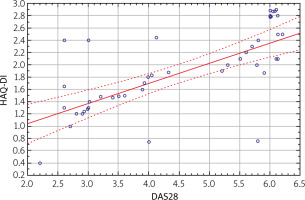
Fig. 2
Health Assessment Questionnaire- Disability Index (HAQ-DI) scatter plot depending on disease activity score with examination of 28 joints (DAS28) in patients with Lyme arthritis. Scatterplot of HAQ-DI against DAS28, HAQ-DI = 0.3755 + 0.3291*x; Conf.Int.
DAS28 – disease activity score with examination of 28 joints, HAQ-DI – Health Assessment Questionnaire-Disability Index.
No significant age quality and life quality relationships were found in patients with RA based on a weak inverse correlation between SF-36 PCS and a weak direct correlation with the Health Assessment Questionnaire-Disability Index.
Age in LA is also not a significant factor for quality of life. Regarding the total number of affected joints, we have the following data: in case of RA, a mean inverse correlation of the number of affected joints with PCS SF-36 and a mean direct correlation with HAQ-DI and a weak feedback correlation with MCS SF-36 take place.
A multiple regression evaluation was performed (Table III) to define the most significant factors that worsen the life quality of patients in both study groups. It turned out that the life quality in patients of both surveyed cohorts was influenced by the duration and activity of the disease, while age and total number of affected joints – only for patients with RA.
Table III
Correlation between Physical Component Summary scale 36-Item Short Form Survey, Mental Component Summary scale 36-Item Short Form Survey, Health Assessment Questionnaire-Disability Index, and the most significant factors according to multiple regression analysis in patients with Lyme arthritis and rheumatoid arthritis
Discussion
The logical conclusion based on the presented results is that the more joints are involved in the pathological process; the lower the patient’s activity in everyday life, the worse the physical and emotional state. This statement is true for RA; however, in patients with LA no relationship was found between these indicators.
For example, Ibn Yacoub et al. [33] examined the disease-related parameters affecting of quality of life of 250 individuals with RA. Their results showed also that PI, disease duration, functional disability, disease activity, and immune status were the main determinants linked with disruption of the quality of life in RA patients.
A similar study was conducted by Haroon et al. [34], who concluded that the quality of life in patients with RA was significantly lower compared with healthy popu-lations, and that functional disability was the most important factor affecting their quality of life. Al-Jabi et al. [11], in 2021, in a study involving 300 patients with RA, showed a relationship between treatment and functional status in order to improve the quality of life and reduce disability. In this case, only timely intervention by a multidisciplinary team of specialists in the treatment and rehabilitation of arthritis patients will allow patients to avoid changes in self-awareness and help to reduce the number of negative consequences of the disease that affect the quality of life [13].
Upon reviewing the results of research of quality of life in patients with RA by Martinec et al. [2], it can be concluded that pain and functional ability may have an important impact on quality of life in RA patients through the restrictions and unpleasant physical sensations they cause.
Salaffi et al. [35] compared the quality of life in patients with RA, ankylosing spondylitis, and psoriatic arthritis, and found that functional impairment and limi-tations due to physical functioning and physical pain had a significant impact on the quality of life in patients with RA as compared to those related to mental health, restrictions arising from vitality, emotional health, and social functioning.
But in our research, in patients with LA a significant decrease in physical activity compared to patients with RA was observed due to a significantly higher rate of PI and reduced overall health quality, and there was a significance difference in the patients’ mental state. Patients with LA have significantly lower scores of vitality, mental health, physical functioning, social activity, and the role emotional.
The value of HAQ-DI in a special questionnaire in patients with RA was in the range 1.1–2.0, which corresponds to a moderate impairment of life, but in patients with LA, this index was in the range of 2.1 up to 3.0, which indicates a greater impact of the disease on the daily activities of patients.
Correlation analysis (Table II) revealed a relationship between disease activity and PCS SF-36 in patients of both cohorts. Based on this, we found that the activity of the disease has a substantial influence on the patients’ life quality. With increasing disease activity, quality of life indicators, in particular PCS, decreased.
In a similar study by Martinec et al. [2] a significant positive correlation was obtained between the VAS pain scale and HAQ-DI. This means that a stronger pain experience leads to worse functional state.
Mean inverse correlations and mean straight lines between HAQ-DI were found between the duration of the disease and the SF-36 PCS in patients of both cohorts examined. This indicator shows that as the duration of the disease increases, the value of the HAQ-DI index increases, and subjects’ ability to perform daily tasks and professional responsibilities decreases significantly.
A relationship was also found between the disease duration and MCS SF-36: in patients with RA – mean direct, and mean reverse – in patients with LA, i.e. in patients with RA, with increasing duration of the disease, the rate of MCS SF-36 increases, due to the mental ada-ptation of the patient to the perception of the disease and health status. Conversely, in patients with LA with increasing duration of the disease the MCS was reduced due to an anxious state and frequent depression.
In a cross-sectional cohort study by Heinimann et al. [36], patients with RA showed a continuous increase of physical disability and articular destruction in parallel with disease duration. Health Assessment Questionnaire-Disability Index scores increased with disease duration. Even when, nowadays, a satisfactory control of disease activity can be achieved in most patients, RA remains a destructive disease leading to physical disa-bility and joint destruction in many patients.
We can speculate that the conscious that joints disease may be connected with infection not with the autoimmune disease caused a more depressive reaction [37, 38]. Depression imposes a significant burden on the health-related quality of life, disability, and mortality of individuals with arthritis [39]. A comparison between LA and RA to summarize the discussions and results obtained is presented in Table IV.
Table IV
A comparison between Lyme arthritis and rheumatoid arthritis to summarize the discussions and results obtained
Conclusions
According to the questionnaire survey results in patients with LA and RA, we confirmed a negative effect of arthritis on all indicators of the life quality in studied patients pursuant to SF-36 scales and the HAQ-DI.
Patients with LA have significantly lower MCS values, which is explained by the patients’ severe psychological adaptation to their own disease, given the prevalence of LD at the present and its tendency towards chronicity.
Factors that influence the life quality of patients in both groups are the disease activity and duration, while age and the total number of affected joints are significant only for patients with RA.




