Introduction
Paraneoplastic rheumatic syndromes are rare. They are the indirect result of a tumor or its metastases. The signs and symptoms may be induced by substances secreted by the neoplasm (hormones, cytokines) or the immune system’s response to the tumor cells. Many organs can be involved even at sites distant to the primary tumor. Rheumatic paraneoplastic syndromes may occur during the course of neoplastic disease; they can precede the diagnosis by a number of years, appear simultaneously or occur after the diagnosis of malignancy. Rheumatic disease signs/symptoms will subside with recovery from malignant disease. Reappearance may suggest relapse of the neoplasia [1]. About 8–10% of cancer patients suffer from paraneoplastic syndromes [2].
Material and methods
We performed a PubMed Medline database search for articles published up to 30th of April 2022. We used key words and phrases related to paraneoplastic rheumatic syndromes and in particular systemic sclerosis, palmar fasciitis and polyarthritis, erythromelalgia, digital necrosis and Raynaud’s syndrome.
PubMed Medline search words included: paraneoplastic systemic sclerosis, paraneoplastic palmar fasciitis and polyarthritis, paraneoplastic erythromelalgia and paraneoplastic digital necrosis and Raynaud’s (Table I).
Table I
Summary of analyzed case reports of paraneoplastic systemic sclerosis, palmar fasciitis and polyarthritis, erythromelalgia and Raynaud’s/digital necrosis in association with non-hematological malignancy
| Authors and year | Type of malignancy |
|---|---|
| Paraneoplastic systemic sclerosis | |
| Orphanos et al. 2008 [5] | Rectal cancer |
| Gangopadhyay et al. 2013 [6] | Non-small cell lung cancer |
| Reynolds, Knights 2014 [7] | Breast cancer |
| Rovisco et al. 2014 [8] | Colorectal carcinoma |
| Samotnij et al. 2018 [9] | Rectal adenocarcinoma |
| Sedhom et al. 2018 [10] | Endometrial carcinoma |
| Paraneoplastic palmar fasciitis and polyarthritis | |
| Wright, Doherty 1997 [4] | Metastatic ovarian carcinoma |
| Enomoto et al. 2000 [11] | Gastric tubular adenocarcinoma |
| Denschlag et al. 2004 [12] | Serous papillary carcinoma of fallopian tube origin |
| Yogarajah et al. 2008 [13] | Poorly differentiated ovarian carcinoma |
| Bolibar et al. 2009 [14] | Ovarian carcinoma |
| Nadal et al. 2013 [15] | Prostate cancer |
| Lazarev et al. 2015 [16] | Small cell lung cancer |
| De Boer et al. 2020 [17] | Prostate carcinoma |
| Okumura et al. 2021 [18] | Lung adenocarcinoma |
| Paraneoplastic erythromelalgia | |
| Mork et al. 1999 [19] | Colon adenocarcinoma |
| Paraneoplastic digital necrosis and Raynaud’s | |
| Wong et al. 2003 [20] | Non-small cell lung cancer |
| Madabhavi et al. 2012 [21] | Lung adenocarcinoma |
| Onitilo et al. 2012 [22] | Squamous cell lung carcinoma |
| Lai et al. 2020 [23] | Ovarian cancer |
| Lokineni et al. 2021 [24] | Squamous cell lung cancer |
Inclusion criteria:
English language,
case report,
free full text article,
paraneoplastic rheumatic syndrome associated with non-hematological malignancy.
The following number of articles meeting the above inclusion criteria were identified in each of the areas:
paraneoplastic systemic sclerosis: 50 articles – 6 met inclusion criteria,
paraneoplastic palmar fasciitis and polyarthritis: 11 articles – 9 met inclusion criteria,
paraneoplastic erythromelalgia: 2 articles – 1 met inclusion criteria,
paraneoplastic digital necrosis: 6 articles. 1 selected as meeting inclusion criteria,
paraneoplastic Raynaud’s phenomenon: 22 articles – 4 met inclusion criteria.
Description of cases
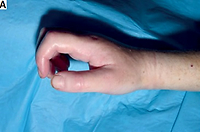
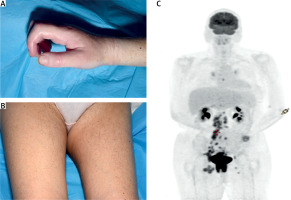
The images presented in Figure 1 concern a 51-year-old woman with a 6-week history of pain and stiffness in the hands and legs which was associated with skin tightening. The patient also reported a 4-week history of diarrhea and faecal incontinence. Further investigations revealed a rectal mass which was confirmed to be a tumor on subsequent MRI of pelvis and rectum. Positron emission tomography (PET) scan demonstrated metastatic lymphadenopathy. Biopsy confirmed poorly differentiated squamous cell carcinoma. In immunological tests anti-RNA-polymerase III antibody (anti-RNAP) was positive. The palliative chemotherapy was used but without efficacy [3].
Fig. 1
Skin tightening in the right hand (A), skin tightening in both thighs (B), PET-CT scan demonstrating metastatic disease (C). Photographs taken in Rheumatology Department, Musgrave Park Hospital in Belfast – not published before.
In 1999 Wright [4] presented a case of a 58-year-old woman with skin thickening, stiffness and swelling. Examination revealed synovitis in metacarpophalangeal joints, palmar erythema as well as skin tightening especially over her palms. There were no features to suggest Raynaud’s phenomenon. There were no systemic symptoms and in the immunological test there were no specific antibodies for any rheumatic disease. The treatment with glucocorticosteroids (GCs) was not beneficial. Ultrasound of the abdomen and pelvis revealed ovarian mass. The final diagnosis was an ovarian carcinoma. Following surgery and chemotherapy the presented symptoms resolved [4].
In our clinical practice there was also a case of a 5-day history of painful and erythematous hands of a 56-year-old woman. In this case the diagnosis of erythromelalgia was established 3 months after diagnosis of ovarian cancer (clear cell carcinoma). Midline laparotomy, total abdominal hysterectomy, bilateral salpingo-oophorectomy and omentectomy were performed and the erythromelalgia resolved completely.
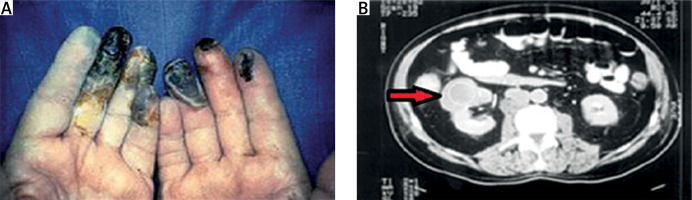
The case of a 71-year-old patient with rapidly progressing digital ischemia presented in Figure 2 A can also be given as an example of paraneoplastic syndrome. The presented patient had a confirmed renal mass (CT scan Fig. 2 B) and final diagnosis was of the renal cell carcinoma.
Discussion
Paraneoplastic syndromes are always a major challenge for clinicians. It is obvious that detection of malignancy at an early stage is important to maximize patient’s chances of curative treatment.
The described cases involve several phenomena/diseases, not only exclusively rheumatic, such as erythromelalgia, but often referred to a rheumatologist and requiring extensive differential diagnosis.
Systemic sclerosis is a connective tissue disease that is characterized by progressive fibrosis of the skin and internal organs. Its pathogenesis is poorly understood. Two types of the disease are recognized: limited (lSSc) and diffuse systemic sclerosis (dSSc). The limited type is characterized by skin involvement which is distal to elbows and knees. It usually progresses slowly and is associated with the presence of anti-centromere antibodies (ACA). In the limited type involvement of lungs and esophagus is observed less often than other organs [25].
In contrast, dSSc is characterized by skin thickening proximal to elbows and knees. It can also affect large areas of the body including anterior trunk and face. All internal organs may be affected but the most important are lungs with interstitial lung disease and fibrosis, kidney involvement, and vascular and heart damage. The diffuse type of SSc progresses rapidly and patients have anti-topoisomerase I antibodies (anti-Scl-70 antibodies) [25].
Raynaud’s phenomenon may be a first and main signal of both types of SSc. Features that should alert a physician to paraneoplastic etiology of both types of SSc include: asymmetrical Raynaud’s phenomenon which is unresponsive to treatment, systemic symptoms, e.g. fatigue, cachexia, temperature dysregulation, sudden onset and rapid progression of clinical symptoms or late onset of the disease (> 50 years of age) personal and/or family history of malignancy, and presence of anti-RNA polymerase III antibodies [9].
Anti-RNA polymerase III antibody is unique to SSc. It is not seen in cancer patients without scleroderma. Patients who are positive have shorter cancer-scleroderma interval (median 0.9 years). It is also associated with > 4-fold increased risk of cancer occurring within two years of SSc onset [26].
There are different types of paraneoplastic polyarthritis including palmar fibromatosis and remitting seronegative symmetrical synovitis with pitting oedema (RS3PE). The RS3PE is characterized by symmetrical polyarthritis that affects the small joints of the hands and feet with associated marked pitting oedema. In this disease response to GCs or disease-modifying antirheumatic drugs (DMARDs) is poor in patients with paraneoplastic etiology [1].
Palmar fasciitis and polyarthritis syndrome (also known as palmar fibromatosis) is most commonly seen in association with ovarian cancer. Palmar erythema and thickening as well as firm and painful nodules are the most common presenting features. Digital swelling and flexion contractures can also be seen [1]. The ovarian cancer is usually already present at an advanced stage (metastatic). Ovarian cancer can be quite difficult to diagnose as patients frequently present with non-specific symptoms.
Furthermore, given that there is currently no ovarian cancer screening this type of malignancy frequently remains undiagnosed until it is at an advanced stage. The most frequently occurring histological type of ovarian cancer associated with these rheumatological symptoms is papillary adenocarcinoma [27]. The pathophysiology of palmar fasciitis and polyarthritis syndrome is poorly understood; however treatment of the underlying malignancy is paramount in the management of these symptoms [27].
Ovarian cancer also may be associated with another paraneoplastic state such as erythromelalgia. This phenomenon is not often described and the case reports analyzed in this article date back to the 1990s [19]. Erythromelalgia is characterized by erythema and severe burning sensation predominantly in the hands and feet. There may also be increased skin temperature. The exact cause of the condition is unknown [28]. It can be primary or secondary. The primary (familial) form of this rare disease results from mutations in SCN9A gene which is involved in making one part of the sodium channel NaV1.7 [29]. These channels are found in nerve cells that transmit pain signals to the spinal cord and brain.
Secondary causes of erythromelalgia include: myeloproliferative disorders (most commonly essential thrombocythemia and polycythemia vera), connective tissue diseases, multiple sclerosis, peripheral neuropathy, diabetes mellitus (type I and II) and infectious diseases (i.e. HIV) [29]. It can also be seen as a side effect of various medications including: bromocriptine and nifedipine. Erythromelalgia symptoms are most frequently bilateral but can also be unilateral. They are thought to result from dysfunctional constriction and dilatation of blood vessels resulting in abnormal blood flow to the extremities. The characteristic feature of erythromelalgia is worsening of symptoms with exposure to heat or exercise and improvement in symptoms with cooling.
Digital necrosis with Raynaud’s syndrome which can be a symptoms of SSc but as in described clinical situation may also be a separate diagnosis is predominantly seen in association with solid tumors (stomach, lung, ovarian cancers) and lymphoproliferative disorders [28]. Raynaud’s syndrome can be primary (most common) or secondary which is most commonly seen in association with autoimmune connective tissue diseases such as systemic lupus erythematous, SSc and Sjögren’s syndrome (SS).
It can also occur in patients with blood disorders such as cryoglobulinemia, thyroid disorders and pulmonary hypertension. The hallmark of the Raynaud’s phenomenon is the triphasic change of colors of the fingers (white–blue–red), especially after exposure to cold. Physicians should be vigilant and consider paraneoplastic syndrome in a patient who is > 50 years of age and presents with thrombocytosis and digital ischemia [30]. Tumors are usually advanced at the time of diagnosis but vascular involvement may resolve after treatment of malignancy.
There are many more rheumatic conditions that can be paraneoplastic in nature; however they are not covered in this review. We focused on diseases manifested by the skin and vascular changes of the hands. Among described clinical situations SSc is a typical autoimmune connective tissue disease. Other symptoms/conditions can accompany the disease such as for example Raynaud’s phenomenon. Polyarthritis with palmar fasciitis is often analysed as different type of arthritis, including rheumatoid arthritis.
Paraneoplastic symptoms in the majority of cases will disappear with successful treatment of the underlying malignancy. Sometimes it may be necessary to treat the rheumatic symptoms with non-steroidal anti-inflammatory drugs or GCs.
Conclusions
In each case of an atypical picture of the disease/phenomenon, asymmetry, later age of onset, cancer in medical history of the patient and their family, exposure to other carcinogenic factors, lack of response to typical treatment or development of other symptoms not corresponding to the disease entity, it requires the clinician’s vigilance and wider diagnostics excluding cancer.
The role of rheumatologist is important particularly in the diagnostic phase.
Diagnosis and targeted treatment of the underlying malignancy is crucial in the management of the paraneoplastic rheumatic syndrome.