Introduction
Psoriasis (Ps) is a chronic, inflammatory disease of immune-mediated etiology, manifested not only by skin lesions, but also associated with the risk of development of an inflammatory process of peripheral joints and involvement of the spine and sacroiliac joints. Psoriatic arthritis (PsA) affects about 20–30% of patients with Ps [1, 2].
The prevalence of Ps is quite difficult to estimate, with as many as 81% of countries lacking accurate information in this regard [3]. It is assumed that the prevalence of Ps globally ranges from 0.5% (China) [4] to 11.9% of the population (Norway) [5]. If we assume that in Poland approximately 1.45% to 2.99% of the population have Ps, according to the estimated prevalence in previous studies conducted in the Polish population [6, 7] then the total number of patients ranges from 550,275 to 1,134,705.
It is known that the presence of Ps itself is associated with the possibility of developing a number of other inflammatory diseases such as inflammatory bowel disease, tendinitis, and uveitis [8]. Significantly, it has been proven to be closely associated with metabolic disorders, especially if the onset of the disease occurs after the age of 40. It is generally estimated that among patients with Ps, approximately 73% develop another inflammation-related disease [9]. The most common diseases associated with Ps include cardiovascular diseases (CVD), type II diabetes, gastrointestinal disease, diseases related to excretory function, rheumatic diseases, and metabolic syndrome [10]. The risk of cardiovascular events among patients with Ps is 1.5 times higher than in the general population, which deserves special attention and appropriate preventive interventions [11].
Psoriatic arthritis is most frequently related to the presence of psoriatic skin lesions, but in about 19% of patients PsA may precede the skin lesions, and a course of PsA without Ps is also possible [12].
The diagnosis of PsA is based on the CASPAR criteria, which include skin lesions of the patient and immediate family members, psoriatic nail changes, absence of rheumatoid factor in serum, dactylitis and the presence of characteristic radiological lesions (adnexal osteoproliferation with exclusion of osteophytes) [13].
Current recommendations for the management of patients with PsA, as well as Ps itself, include an assessment of the cardiovascular risk and possible metabolic changes, and it is recommended that treatment should take into account all aspects of such a complex disease [12, 14]. All information concerning patients with Ps is analyzed and translated into the problem of patients with PsA, which allows for proper treatment and optimal prevention and interventions in this group of patients. The aim of this study is to analyze the most common cardiovascular complications occurring in the course of Ps and PsA.
Prevalence of cardiovascular disease in the psoriasis population
There have been many articles and research studies in the fields of Ps, PsA, and CVD that provide considerable insight into the etiology, mechanisms, and common elements of these often related disease entities.
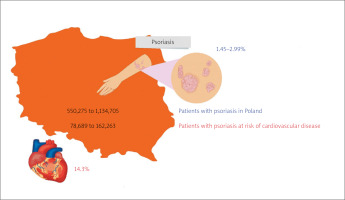
A retrospective study conducted on a population of 753 patients with Ps in North America estimated the risk of cardiovascular events at 14.3% [15]. If a similar assumption is made, 78,689 to 162,263 patients with Ps in Poland are likely to develop CVD (Fig. 1) [6, 7, 15].
Fig. 1
Estimated prevalence of psoriasis and cardiovascular disease in the psoriasis population in Poland [6, 7, 15].
This phenomenon is primarily driven by chronic inflammation, endothelial dysfunction, and traditional cardiovascular risk factors such as type II diabetes, hypertension, obesity, and nicotine addiction [16]. Moreover, many studies confirm that the risk of CVD among patients with Ps increases with the exacerbation of the inflammation in the skin area and the duration of the disease. Furthermore, it is estimated that each year of the disease – in the case of Ps – increases the risk of serious adverse cardiovascular events by 1% [17].
Cardiovascular system involvement in psoriasis
Inflammation of blood vessels (vasculitis)
The severity of psoriatic lesions assessed by the Psoriasis Area Severity index (PASi) has been shown to be positively correlated with vascular (aortic) inflammation as demonstrated by positron emission tomography/computed tomography with 18F-fluorodeoxyglucose labeling (PET/CT-FDG) and assessment of the aortic target-to-background ratio. This correlation was independent of traditional risk factors for cardiovascular events [18]. Among patients with Ps with more than 10 years of the disease, the risk of vascular inflammation is significantly increased compared to the general population and the population of patients with less than 10 years of the disease [17].
It is known that chronic inflammation causes damage to the endothelium, disrupts its homeostatic function and induces a local inflammatory response in the blood vessels. Thus, it also causes thickening of the carotid intima-media membrane complex and coronary microvascular dysfunction, and contributes to atherosclerosis [17, 19].
Atherosclerosis
Previous studies indicate a positive correlation between Ps and calcium deposition in coronary arteries, as well as endothelial dysfunction caused by chronic inflammation, which is the starting point for atherosclerosis [20]. The combination of these two phenomena – atherosclerotic plaque formation and skin plaques that appear in Ps – is described in the literature as two plaques for one syndrome [21] because they share a similar profile of cytokines secreted by Th1 (tumor necrosis factor α [TNF-α] and interferon γ [IFN-γ]) and Th17 (interleukin 17 [IL-17] and IL-22) lymphocytes [22, 23]. A study by Yamazaki [24] indicated that the pro-inflammatory cytokine TNF-α has the greatest impact on atherosclerosis formation.
The development of psoriatic complications, to which genetic predisposition and environmental factors contribute, was called the “psoriatic march” by Boehncke WH [25].
Genetic factors include expression and mutations of the CARD14 (caspase recruitment domain, family member 14) gene, which is found not only in the keratinocytes but also in vascular endothelial cells as a potential risk factor for inflammatory and atherosclerotic changes [26]. Furthermore, in Ps an increased serum homocysteine level resulting from DNA demethylation is observed, which is also an independent risk factor for cardiovascular incidents [27].
The systemic inflammation associated with Ps, along with modifiable risk factors such as obesity, directly contributes to insulin resistance and consequently also exacerbates endothelial dysfunction and coronary artery calcification [24]. This is followed by the formation of an atherosclerotic plaque that causes reduction or closure of blood flow through the vessel (usually by plaque rupture), leading to myocardial infarction or stroke (Figs. 2, 3) [28].
Fig. 2
Atherosclerotic plaque in the carotid artery of a patient with psoriasis – longitudinal section of the vessel. Material: Department of Radiology, National Institute of Geriatrics, Rheumatology and Rehabilitation, Warsaw.
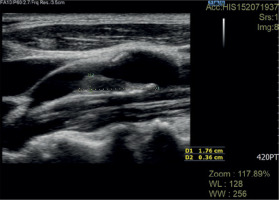
Fig. 3
Atherosclerotic plaque in the carotid artery of a patient with psoriasis – cross-section of the vessel. Material: Department of Radiology, National Institute of Geriatrics, Rheumatology and Rehabilitation, Warsaw.

Moreover, patients with chronic inflammatory diseases may be affected by inflammation-enhanced atherosclerotic syndrome, which differs from atherosclerosis in its course and symptoms in some patients [29].
Myocardial infarction
Proinflammatory cytokines released due to endothelial damage contribute to oxidative stress, which in turn leads to destabilization of the atherosclerotic plaque. Moreover, the imbalance between oxidants and antioxidants significantly accelerates the course of atherosclerosis and other cardiovascular incidents [19]. Due to rupture of atherosclerotic plaque with subsequent thrombus development, the coronary artery lumen is closed, blood supply to the myocardium is limited, and myocardial necrosis occurs [30]. Taking Ps as a CVD risk factor, it has been shown that patients over 30 years of age (third and fourth decades of life), characterized by a severe course of Ps, are at high risk of death from myocardial infarction [31].
Stroke
Psoriasis increases the risk of stroke [32]. Atherosclerotic plaque formation in the carotid arteries contributes to ischemic stroke [33], which occurs more frequently in the Ps population than in the general population in both mild and severe Ps patients, significantly increasing CVD mortality [34]. The risk of ischemic stroke in this population is not fully elucidated and, according to some researchers, is not caused by an increased presence of the traditional cardiovascular risk factors but by the inflammation itself associated with Ps and PsA [33–35]. A severe course of Ps, according to a study by Gelfand et al. [35], increases the risk of stroke in the Ps population by 44%.
Moreover, the therapies used in the treatment of Ps and PsA influence the prevalence of myocardial infarction and ischemic stroke; we can observe both protective effects, e.g. methotrexate (MTX) or adalimumab (TNFi) for both these diseases or phototherapy for Ps, and increased risk of CVD, e.g. non-steroidal anti-inflammatory drugs and glucocorticosteroids [23, 34, 36].
Atrial fibrillation
The severity of Ps determines the occurrence of thromboembolic incidents and atrial fibrillation (FA). The risk of arrhythmia is additionally increased by factors predisposing to cardiovascular incidents accompanying severe Ps [37]. The process inducing this phenomenon is inflammation, which contributes to the oxidative damage in the left atrial tissue, thereby impairing its function [38]. The reduction of blood flow velocity in the left atrium (usually caused by the extension of inflammation to the atrium and/or atrial fibrosis) results in thrombus formation, which may eventually lead to an ischemic stroke. In addition, the inflammatory process causes an increase in epicardial fat mass and initiates the secretion of proinflammatory adipocytokines, resulting in atrial morphological changes and microcirculatory abnormalities.
Psoriasis as a risk factor increases the prevalence of FA from 25% to 50%, particularly in young, severely affected individuals [39].
Hypertension
Hypertension among patients with Ps is closely correlated with the course of the inflammatory skin disease, and the prevalence of the disease is significantly higher than in the general population [40]. Moreover, the treatment of hypertension in this group of patients often requires triple oral therapy due to the specific complexity of controlling blood pressure. It is estimated that the need for this type of therapy is 16.5 times higher among patients with Ps [41]. At the same time, hypertension is a part of the metabolic syndrome, which doubles the risk of cardiovascular incidents [42].
Moreover, hypertension is also a risk factor for the development of psoriatic dermatitis, and this correlation proves to be statistically significant even after excluding demographic variables, concomitant diseases, and medications used, including those that lower blood pressure [43].
Metabolic syndrome
Metabolic syndrome is a combination of cardiovascular risk factors including visceral obesity, dyslipidemia, glucose intolerance, and hypertension [44]. The most commonly used definition is that given by the National Cholesterol Education Program Adult Treatment Panel III. This definition requires that an individual has at least three of the following risk factors: 1) increased abdominal circumference, 2) low plasma high-density lipoprotein cholesterol, 3) elevated plasma triglycerides, 4) elevated blood pressure, 5) elevated glucose levels [45]. The presence of at least three of the five criteria allows the diagnosis of metabolic syndrome [46, 47]. Metabolic syndrome is estimated to affect about 20% to 50% of Ps patients [48]. A study by Kazlauskienė et al. [49] showed that metabolic syndrome alone significantly increases the risk of myocardial infarction by 1.8 times, and stroke by 2.05 times.
Psoriasis is a risk factor for obesity, but obesity may also contribute to the development of Ps. Obesity in the Ps population is a result of reduced physical activity due to Ps, but also because of the psychological consequences of the disease, including depression, which leads to reduced physical activity. Furthermore, visceral fat, accumulated excessively in this group of patients, plays a key initiating role for hypertension, insulin resistance or hyperlipidemia. In contrast, chronic inflammation (due to Ps or obesity) that disrupts the insulin signaling mechanism contributes directly to insulin resistance [50].
Hyperuricemia
A disorder that is associated with both Ps and metabolic syndrome is hyperuricemia, which is also an independent risk factor for CVD and Ps. The increased risk of obesity in the psoriatic population contributes to increased serum uric acid levels [51], which consequently leads to the impaired migration and proliferation of endothelial cells. The presence of uric acid in the blood initiates the inflammatory process and fat accumulation in liver cells, and contributes to oxidative stress in adipocytes. The oxidative stress induced by hyperuricemia also leads to impaired cardiomyocyte activity and initiates apoptosis of myocardial cells [52].
The main reason for hyperuricemia is believed to be impaired excretion or excessive production of uric acid in the body, which in Ps is caused by the increased purine degradation associated with rapid DNA degradation due to excessive keratinocyte proliferation [53].
Although hyperuricemia itself is an important factor in increasing CVD risk, it is not necessarily associated with concomitant accumulation of uric acid deposits in tissues or the occurrence of gout attacks; however, the risk of gout is also increased in patients with Ps [54, 55].
Nevertheless, in the case of hyperuricemia, after the assessment of CVD risk, the target concentration of uric acid should be established and both non-pharmacological (lifestyle, including diet, possible correction of the drugs used, weight reduction, prohibition of alcohol) and pharmacological management reducing the serum uric acid concentration should be recommended.
miRNAs and cardiovascular risk
One of the key factors involved in the development of CVD is a single-stranded RNA molecule, miR-200c, which expression level is significantly elevated in the bloodstream of Ps patients. Due to its positive correlation with both PASI and disease duration, it is thought that it may represent an inflammatory biomarker for Ps [56]. High expression levels of miR-200c induce endothelial dysfunction, which is also associated with destabilization of atherosclerotic plaques by affecting the expression of miR-33a and miR-33b, which regulate cholesterol homeostasis [57].
Another important molecule is miR-22, increased expression levels of which are characteristic of cardiomyocyte hypertrophy, while low levels are found in femoral arteries whose lumen has been narrowed by an atherosclerotic plaque [58]. A low level of miR-22 expression is observed in the population of patients with Ps, which is probably due to the presence of atherosclerotic plaques [57].
An equally important molecule is miR-378a secreted by cardiomyocytes, whose overexpression contributes to the cardiovascular incidents in this population. Another molecule crucial for the development of CVD is miR-340, which regulates immune cell proliferation and is responsible for the development of several auto-immune diseases, including Ps [59]. There are more miRNA molecules associated with both Ps and CVD, but there are still insufficient clinical trials using therapies based on inducing or inhibiting the expression of particular miRNA molecules in the Ps patient population. Further research in this area is needed to develop tailored therapy and early detection of cardiovascular incidents.
Prevention of cardiovascular events
The recommended preventive interventions in this group at risk include monitoring of body weight (BMI greater than or equal to 25 kg/m2 is an indication for screening for diabetes on average every 3 years), blood pressure (over 40 years of age – indication for screening every 3–5 years, with high risk of hypertension – every year), lipid levels (cholesterol, triglycerides), hemoglobin, or abdominal circumference [12].
In terms of physical activity, a properly tailored exercise plan in the Ps population has been proven to alleviate symptoms and reduce the risk of cardiometabolic diseases, which are significantly caused by low levels of physical activity. Moreover, this relationship is also observed among patients with a family history of Ps [60].
The key intervention should be first of all reduction of inflammation through available therapies. In the case of both peripheral and axial forms of Ps, treatment with non-steroidal anti-inflammatory drugs (depending on the form) and biologicals (e.g. anti-TNF, anti-IL-12/23, anti-CTL-4), and in the peripheral form of PsA, treatment with synthetic modifying drugs (e.g. MTX) and biologicals should be applied.
Adequate physical activity, which reduces inflammation and the psycho-emotional consequences of the disease, are also essential for the regulation of BMI, the efficiency of the musculoskeletal system and the stabilization of the cardiovascular system through effects on the sympathetic and parasympathetic nervous system, reduction of insulin resistance, lipid circulation, and molecular and metabolic adaptation of the heart muscle [61].
Reducing the risk of cardiovascular incidents should also include a reduction in blood lipid levels, which can be achieved with lipid-regulating drugs with also a beneficial anti-inflammatory profile, mainly statins [62]. A helpful guideline for starting hypolipemic therapy and other therapeutic interventions should be the percentage of cardiovascular incident risk according to the table developed by the European Society of Cardiology multiplied by a factor of 1.5 [11].
To summarize the topic, Table I presents the results/conclusions from selected clinical trials on the occurrence and type of cardiovascular incidents in patients with Ps and PsA. Publications were searched using Google Scholar, PubMed, and Scopus, using phrases such as “psoriasis” and “psoriatic arthritis”, in combination with “stroke”, “cardiovascular”, “prevention”, “atherosclerosis”, “hypertension”, “myocardial infarction”, “metabolic syndrome”, “hyperuricemia”, and “uric acid”. Inclusion criteria: original study, number of patients participating in the study more than 200, evidence of an association between Ps or PsA and the occurrence of CVD, articles published after 2000. The search was limited to article titles and abstracts. Figure 4 illustrates the process of searching and screening the publications.
Table I
Prevalence of cardiovascular events in the psoriasis and psoriatic arthritis patient population in selected clinical trials [17, 35, 43, 63–67].
| Study | Population | Observation time | Type of study | Country | Main findings |
|---|---|---|---|---|---|
| Kim et al. 2018 [43] | n = 42,726 patients with hypertension n = 213,630 control group | 2003–2013 | Prospective, nationwide population-based cohort study | Korea | 9,254 cases of psoriasis during 11 years of follow-up. The incidence of psoriasis was higher in the hypertensive group by 1.7% |
| Egeberg et al. 2017 [17] | n = 87,351 patients with psoriasis n = 4,234,793 control group | January 2013–June 2016 | Prospective study | Denmark | The study showed a strong association between the duration of psoriasis and the occurrence of adverse cardiovascular events and vasculitis |
| Eder et al. 2015 [63] | n = 235 patients with psoriatic arthritis | 1978 – cohort established 2010–2013 carotid ultrasound assessment | Prospective study | Canada | Increased cardiovascular risk is influenced by the presence of traditional cardiovascular risk factors prior to the development of psoriatic arthritis |
| Ogdie et al. 2015 [64] | n = 8,706 patients with psoriatic arthritis n = 41,752 patients with rheumatoid arthritis n = 138,424 patients with psoriasis | 1994–2010 | Population-based longitudinal cohort study | United Kingdom | There is an increased risk of myocardial infarction and stroke among patients with psoriatic arthritis as well as severe psoriasis. Deaths due to cardiovascular incidents are significantly more frequent among patients with rheumatoid arthritis and severe psoriasis |
| Gladman et al. 2009 [65] | n = 648 patients with psoriatic arthritis | 1978–2004 | Prospective study | Canada | The inflammatory process that accompanies psoriatic arthritis contributes to increased incidence of hypertension, myocardial infarction, and angina |
| Prodanovich et al. 2009 [66] | n = 3,236 patients with psoriasis n = 2,500 patients without psoriasis | January 1985–December 2005 | Retrospective study | United States | Psoriasis is associated with atherosclerosis, ischemic heart disease, peripheral vascular disease, and increased mortality from cardiovascular causes |
| Gelfand et al. 2009 [35] | n = 129,143 patients with a moderate course of psoriasis, n = 3,603 patients with severe course of psoriasis respectively: n = 496,666 control group, n = 14,330 control group | 1987–2002 | Retrospective study | United Kingdom | Psoriasis patients with severe symptoms are at high risk for stroke. This phenomenon occurs independently of major stroke risk factors |
| Gelfand et al. 2006 [67] | n = 130,976 patients with psoriasis n = 556,995 patients without psoriasis | 1987–2002 | Prospective, population-based cohort study | United Kingdom | The risk of myocardial infarction in the psoriasis population is high, especially in young people. |
Conclusions
Patients with Ps show a higher prevalence of traditional risk factors for cardiovascular events. Psoriasis is associated with occurrence of additional risk factors. Thus, diagnosis of Ps should focus the attention of the physician on risk factors both general and specific for the disease. Observation of these patients and periodic assessment of the development of cardiovascular complications is necessary, particularly for patients with body surface involvement greater than or equal to 10%.
Preventive measures available to reduce CVD risk such as therapies with effective inflammation-reducing drugs (classical and biologic disease-modifying agents) and recommendation of the lifestyle changes that should be made.





