Introduction
Lumbosacral transitional vertebra (LSTV) and spina bifida occulta (SBO) are common congenital malformations of the spine, found incidentally during work-up for lower back pain (LBP). Lumbosacral transitional vertebra occurs due to the abnormal fusion of the sacrum with the vertebra above, to a variable extent [1].
It results either from sacralization of the fifth lumbar vertebra (L5) or lumbarization of the first sacral vertebra (S1) (partial or complete). An extra joint is formed between the ala of sacrum and the elongated transverse process of the vertebra above on one or both sides, which can result in LBP.
Spina bifida occulta occurs due to non-fusion of the posterior elements of the vertebral arch [2]. Unlike spina bifida, it has no neurological sequelae and is usually asymptomatic. It commonly affects L5 and the lower part of the sacrum.
Patients with LBP frequently consult rheumatologists due to suspicion of spondylarthritis. Radiograph of the pelvis in the antero-posterior projection is obtained in such patients to visualize the sacroiliac joints. It is not unusual to find other incidental findings, which may or may not contribute to back pain. Lumbosacral transitional vertebra, being the commonest malformation of the spine, is frequently noticed.
We present perhaps the first-ever case series of 27 LBP patients with coexisting LSTV and SBO. Both being congenital malformations of the spine, there is a possible association between them. According to epidemiologic data, SBO has an overall prevalence of 12.4% in the general population [3].
The aim of our article is to encourage researchers to consider further observational studies with larger number of subjects to assess the true nature of association of LSTV and SBO in patients with LBP. In addition, our study aims to increase awareness about LSTV as an important cause of LBP.
Material and methods
The patients described in the paper were seen in the Rheumatology Clinic of Fortis Hospital, Vasant Kunj, New Delhi, between April 2019 and March 2021. Patients with LBP along with LSTV on pelvic radiograph were included in the study. Severity of back pain was assessed on a Visual Analogue Scale (VAS) from 0 to 10. Requirement for analgesics was recorded by non-steroidal anti- inflammatory drug (NSAID) index [4].
Additional clinical features were also noted (as discussed further). Radiograph of the pelvis (antero-posterior projection), complete hemogram, erythrocyte sedimentation rate, C-reactive protein, and liver and kidney function tests were obtained in all the patients. Magnetic resonance imaging of the pelvis (and/or spine) and radiograph of the spine were ordered if clinically indicated.
Statistical analysis was performed using the test of a single proportion. The z-score obtained was 4.87, which gave us a 2-tailed p-value of < 0.001. Thus, the 95% confidence interval for the prevalence of SBO in a population of LSTV was 30.24–53.76%. This suggests that SBO occurs more frequently in patients with LSTV than in general population (p-value < 0.001).
Results
Descriptions of selected cases
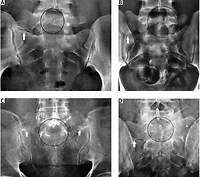
Case 1. A 26-year-old woman had LBP for 2 years, with pain aggravated by prolonged standing and bending forwards. Examination revealed joint hypermobility. Radiograph of the pelvis showed pseudo-articulation of elongated right transverse process of L5 with ala of sacrum (white arrow, Fig. 1 A), suggestive of LSTV. In addition, there was non-fusion of posterior elements of the vertebral arch of L5, suggestive of SBO (encircled area, Fig. 1 A).
Fig. 1
Radiographs of the pelvis, antero-posterior projections of cases 1 to 5. Type IIA lumbosacral transitional vertebra (LSTV) on the right side (white arrow) and spina bifida occulta (SBO) of the fifth lumbar vertebra (L5) (encircled area) (A). Type IA LSTV on the right side (white arrow) and SBO of L5 (encircled area) (B). Type IIIB LSTV (white arrows) and SBO of L5 (encircled area) (C). Type IV LSTV (type II on the right [white arrow] and type III on the left side [asterisk]) and SBO of L5 (encircled area); bilateral sacroiliitis is also present (D). Type IIA LSTV on the left side (white arrow) and SBO of the sacrum (encircled area) (E).
Case 2. A 32-year-old man had LBP radiating to the right lower limb with a burning sensation in the right foot. Symptoms were aggravated by prolonged stan-ding. Straight leg raising test was positive on the right side at 45 degrees. Radiograph of the pelvis showed type I LSTV on the right side (white arrow, Fig. 1 B) (discussed further) along with SBO (encircled area, Fig. 1 B).
Case 3. A 38-year-old man complained of LBP radiating to both lower limbs. Examination showed bilateral positive straight leg raising test at 40 degrees. Radiograph of the pelvis showed elongated transverse processes of L5, which were almost completely fused with the ala of the sacrum on both sides (white arrows, Fig. 1 C). Non-fusion of posterior elements of the vertebral arch of L5 was also observed, suggestive of SBO (encircled area, Fig. 1 C).
Case 4. A 33-year-old man with known axial spondylarthritis for 5 years. The patient complained of persistent LBP for 3 months, in spite of being on treatment with adalimumab; he had normal acute phase reactants. Radiograph of the pelvis showed complete fusion of the left transverse process of L5 with sacral ala (asterisk, Fig. 1 D) and pseudo-articulation of the right transverse process of L5 with ala of sacrum (white arrow, Fig. 1 D).
This was suggestive of type IV LSTV (discussed further). Non-fusion of posterior elements of the vertebral arch of L5 were also observed, suggestive of SBO (encircled area, Fig. 1 D). Sclerosis and narrowing of the joint space were noted in the lower part of both sacroiliac joints. Lumbosacral transitional vertebra was the cause of his current back pain. Spondylarthritis was under control, as shown by normal values of acute phase reactants.
Case 5. A 42-year-old man had LBP radiating to the left lower limb for 6 months. Bending forwards and coughing aggravated the symptoms. Examination revealed tenderness in the left sacroiliac joint area with positive straight leg raising test at 50 degrees on the left side. Radiograph of the pelvis showed elongated left transverse process of L5 with its pseudo-articulation with ala of sacrum, suggestive of LSTV (white arrow, Fig. 1 E). Non-fusion of posterior elements of the lower part of the sacrum was observed, suggestive of sacral SBO (encircled area, Fig. 1 E).
Cases 6 and 11 [5] were inadvertently administered tumor necrosis factor (TNF) α inhibitors elsewhere because they had human leukocyte antigen (HLA) B27 in addition to LBP. The treatment did not provide relief and no evidence of spondylarthritis was found on further work-up. However, both patients had LSTV and SBO.
Case 7 had axial spondylarthritis, which was being treated with etanercept. The patient complained of new-onset LBP for 2 months. However, his acute phase reactants were normal. Radiograph of the pelvis showed LSTV and SBO in addition to bilateral sacroiliitis. Like case 4, LSTV was the cause of this patient’s current back pain because the spondylarthritis was well controlled.
A total of 3412 patients were seen in the clinic during the study period. Out of these, 33.8% (n = 1152) had back pain, 52.3% had peripheral arthritis, and 13.9% had miscellaneous disorders, which included vasculitis, fibromyalgia, autoinflammatory syndromes, etc. Sixty-four patients with LBP attending the rheumatology clinic of our hospital during the study period had LSTV. Out of these, 27 patients also had SBO (42.18%).
Radiculopathy was the most common symptom in addition to LBP, which was observed in 44.4% of patients (66.6% unilateral and 33.3% bilateral). The me- dian duration of LBP before diagnosis of LSTV and SBO was 24 months. Three (11.1%), 18 (66.6%), 4 (14.8%), and 2 (7.4%) patients had type I, II, III, and IV LSTV according to Castellvi classification, respectively [6].
Means of pain score on VAS and NSAID index were 4.4 and 39.3, respectively. Eighteen per cent of the analysed patients had additional causes of LBP, including prolapsed intervertebral disc, vitamin D deficiency, spondylarthritis (SpA), and osteoporotic morphometric fractures.
A summary of clinical data and identification of the type of LSTV are presented in Table I.
Table I
Summary of clinical data and identification of the type of lumbosacral transitional vertebra and level of spina bifida occulta
Discussion
Lumbosacral transitional vertebra and SBO are common congenital malformations of the spine. They are usually detected incidentally while evaluating patients with LBP. We observed frequent co-existence of LSTV and SBO in patients attending our rheumatology clinic for evaluation of LBP. There are only a few case reports in the literature reporting such co-existence [5, 7].
Lumbosacral transitional vertebra can be classified into 4 types according to Castellvi classification [6]. In type I, the transverse process of L5 (or lumabarized S1) and ala of sacrum are in contact with each other, without forming any joint. Joint formation occurs in type II. In type III, there is complete bony fusion of the transverse process and sacrum. Type IV is the co-existence of type II on one side and type III on the other side, in the same individual. Types I, II, and III are further labelled A or B depending on whether the pseudo-articulation is unilateral or bilateral, respectively.
Spina bifida occulta is one of the neural tube defects, which is usually asymptomatic. Its population prevalence is about 12% [4]. It is commonly detected incidentally. It occurs due to the failure of fusion of posterior elements of vertebrae during embryogenesis [2]. It can be associated with overlying tuft of hair, pigmentation of skin, sinus tract, or lipoma. Rarely, neurological manifestations can be observed in those who develop tethering of the spinal cord within the spinal canal. Also, SBO leads to inappropriate distribution of weight and attachment of muscles due to incomplete vertebral arch [8, 9].
The African study by Muthuuri [10] showed that spinal instability due to SBO leads to abnormal pelvic growth and anatomy. Formation of an extra joint due to the transitional vertebra perhaps compensates for the mechanical instability.
Lumbosacral transitional vertebra can give rise to LBP, which is termed as Bertolotti’s syndrome [11].
Various mechanisms have been hypothesized for the genesis of pain in LSTV. One of them is the development of degenerative changes in the joint between the transverse process of L5 (or lumbarized S1) and ala of sacrum [12]. In addition, prolapsed intervertebral disc was more common in patients with LSTV in a study by Otani et al. [13]. The extra joint due to pseudo-articulation results in altered rotational movement in the lower part of the spine. This leads to early development of degenerative changes in the facet joints, intervertebral disc space, and spinal canal, leading to back pain [14].
Two of our patients had axial SpA (case 4 and case 7), who were on treatment with TNF-α inhibitors (adalimumab and etanercept, respectively). Despite normal acute phase reactants, both patients were perturbed with LBP. Radiographs of the pelvis revealed LSTV and SBO. Magnetic resonance imaging of the sacroiliac joints did not reveal evidence of acute sacroiliitis in either of the patients. However, sclerosis and erosions in the sacroiliac joints were present, suggestive of chronic sacroiliitis. Therefore, LSTV was the cause of the current back pain in both cases, which was treated with adequate measures; treatment for SpA was not escalated.
Not infrequently, HLA-B27 test is obtained in patients with LBP. 6% of the general population is positive for HLA-B27, without SpA [15]. Some of these patients even have LBP, but HLA-B27 might not contribute. Such patients should be assessed carefully for the cause of the LBP to prevent incorrect labelling with SpA, as had happened in case 6. We have previously reported a similar patient who was inadvertently treated with etanercept. On further evaluation, there was no evidence of spondylarthritis besides HLA-B27. Instead, the described patient had LSTV along with SBO [5].
Non-steroidal anti-inflammatory drugs and physio-therapy are the first-line treatment options in LSTV and SBO [16]. Local injection of an anesthetic agent and glucocorticosteroids into the extra articulation has also been used [12, 17]. Anti-epileptic drugs like gabapentin can be used for radiculopathy associated with LSTV. Refractory cases can undergo nerve block or surgery [16].
Study limitations
The first limitation of the presented study is its small sample size. Lower back pain is a common symptom, which is managed by many specialties including neu- rology, neurosurgery, orthopedics and general medicine in addition to rheumatology.
However, the patients included in our study were recruited only from the rheumatology clinic of our hospital, which is the second limitation. Lastly, for statistical analysis, we used a 12.4% population prevalence of SBO, as published before, because we did not have our own data on the population prevalence of SBO in our region.
Conclusions
Statistical analysis of our study showed that the frequency of SBO was significantly greater in patients with LSTV as compared to the general population (p-value < 0.001).
The results of our study suggest that LSTV and SBO, both being congenital malformations of the spine, co-exist more frequently than just chance occurrence, and there is possibly an association between them.
In patients with SpA and LBP, clinicians should be very careful in managing, because an incorrect assessment of the source of pain can lead to unnecessary changes of SpA treatment without obtaining the expected effect.