Introduction
Total hip arthroplasty (THA) is a widely performed procedure in the treatment of hip osteoarthritis (OA). Total hip arthroplasty owes its popularity to both high efficacy and cost-effectiveness [1, 2]. Moreover, most patients report very high satisfaction after the operation [3, 4]. However, the high level of satisfaction with THA goes together with surgeons’ great responsibility of meeting patients’ expectations [3].
The final outcome of THA depends on various factors, the most important of which are use of the appropriate surgical technique and proper prosthesis components’ placement [5, 6].
To obtain both the best functional and radiological results, minimal wear and risk of reoperation, femoral and acetabular component parts must be placed properly in such a way that recreates the center of rotation (COR) as close as possible to the normal side [7].
Restoration of the COR is crucial for reconstruction native hip biomechanics after THA. It allows for proper muscle tension and force distribution in the hip joint [8]. Malposition of the components can lead to variety of clinical problems, and even increase the risk of dislocation [6].
To achieve these goals, a surgeon has to overcome several obstacles. One of the most serious mistakes that can negatively affect postoperative functional outcomes is shift in THA cup positioning. It might be a consequence of poor acetabular roof structure and inadequate bone molding during the cup placement [9]. Both vertical and horizontal misplacement of the acetabular component are commonly observed radiological findings [7, 10–13]. Center of rotation malposition leads to improper force distribution, different muscle tension and thus poorer postoperative results [7].
During THA acetabular component placement thesurgeon has to assess the optimal cup placement position based on the hip joint anatomy. It is possible that the superior border of the native acetabulum morphology has an impact on cup positioning and COR restoration in patients undergoing THA.
The anatomical variation of the acetabular structure may confuse the surgeon during THA, resulting in the placement of the cup that will lead to COR malposition. Perhaps the shallow superior roof of the acetabulum may predispose to a shift of the COR of the cup to the superior part and result in lowering adductor muscles’ force vectors.
The aim of this study was to assess whether the superior border of the native acetabulum morphology has an impact on cup positioning and COR restoration in patients undergoing THA as treatment of primary OA of the hip.
Material and methods
The study cohort comprised 150 consecutive patients (62 males, 88 females) who were diagnosed with end-stage primary hip OA (grade 4 according to Kellgren-Lawrence classification). Mean age of the participants was 69.67 (range 50–93). The ratio of operated sides (right to left) was 85 : 65. Their clinical condition was assessed on the basis of the modified Harris Hip Score (mHHS) scale and range of motion examination both preoperatively and postoperatively. All patients underwent total hip replacement surgery between January 2021 and December 2021 at the single institution. All the participants met the inclusion criteria:
age above 50 years on the day of the surgery,
diagnosed with end-stage primary hip OA,
qualified for total hip replacement surgery,
diagnostic radiographs taken pre- and postoperatively.
Patients who were excluded from the study were:
diagnosed with a different condition than end-stage primary hip OA,
referred for surgery other than total hip replacement,
those for whom non-diagnostic radiographs were taken.
All operations were performed at a level III academic hospital, by a single fellowship-trained surgeon. All patients were operated through an anterolateral approach with the patient lying on the healthy side with one-third medium gluteal muscle dissection. Uncemented Polarstem/R3 total hip implants (Smith & Nephew, Warsaw, IN, USA) were used in every case (Fig. 1). Femoral neck dissection was performed after full joint dislocation, between the tip of the greater trochanter to the point 10 mm proximal to the lesser trochanter. The acetabular cup was placed aiming 40–45 degrees of acetabular cup inclination and 10–15 degrees of anteversion. Such values were possible to achieve within the surgery using a dedicated positioning guide supplied by the prosthesis manufacturer. The femoral stem was aimed to be placed in the anatomical axis of the femur. The postoperative protocol included chemical and mechanical thromboprophylaxis unless specifically contraindicated. All patients received one dose of parenteral antibiotics at the induction of anesthesia and two further doses post-operatively. No pre- or postoperative ectopic bone formation prophylaxis was performed.
Fig. 1
Acetabular roof angle measurement.
α – angle between the most lateral and the most superior part of the native acetabulum.

Standard standing anteroposterior pelvic X-rays were performed pre- and postoperatively and appropriate measurements were taken.
The authors performed analysis of the X-ray images using the INFINITT PACS system (INFINITT Healthcare, Seoul, South Korea). Evaluation included preoperative acetabular roof angle measurement, pre- and postoperative center of rotation, femoral offset, cup offset and total offset assessment. Acetabular offset in this study is defined as the distance between the center of the femoral head and the pelvic teardrop [14]. Preoperative X-rays showing the technique whereby the authors measured the mentioned parameters are presented below (Figs. 1–5).
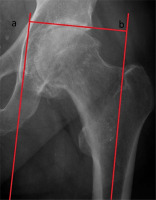
Fig. 2
Determination of center of rotation (COR).
a – line at level of ischial tuberosities, b – line at level of iliac crests, c – line perpendicular to lines a and b, passing through points D and E; D, F – points situated along the horizontal line at level of cup’s subchondral roof; E – point located 5 mm lateral to intersection of Shenton’s and Köhler’s lines; G – equidistant between E and F (center of rotation – COR).

Fig. 3
Cup offset measurement – distance between a and b.
a – line through medial wall of quadrilateral plate, b – line passing through center of rotation (COR).
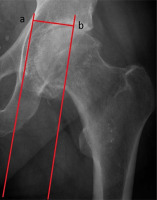
Fig. 4
Femoral offset assessment – distance between a and b.
a – line bisecting long axis of femur, b – line passing through center of rotation (COR).

Fig. 5
Total offset measurement – distance between line a and b.
a – line through medial wall of quadrilateral plate, b – line bisecting long axis of femur.
Statistical analysis
Statistical analysis of results was performed. All comparisons were performed between continuous variables.
Due to significant deviation from normality of the distribution examined with the Shapiro-Wilk test, Spearman’s rank correlation coefficient was used to measure the association between the given variables.
The significance level was set at a p value < 0.05. All statistical analyses were conducted using SAS software, Version 9.4 for Windows (SAS Institute Inc., NC, USA).
Bioethical standards
This retrospective study was conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The X-ray imaging assesment was the part of routine managament in OA patients who are planned to undergo arthroplasty and in postoperative evaluation. Informed consent was obtained from every participant of the study.
Results
The study revealed that there was significant positive weak correlation between change in cup offset and acetabular roof angle (rs = 0.25, p = 0.002). This means that in patients whose preoperative acetabular roof angle was higher, the change in acetabular offset was more distinct.
There were insignificant positive associations between acetabular roof angle and change in COR (rs = 0.14, p = 0.097), acetabular roof angle and change in total offset (rs = 0.087, p = 0.29) and a negative association between acetabular roof angle and femoral offset (rs = –0.071, p = 0.39) (Table I).
Table I
Comparison of X-ray measured parameters. Rs-value and p-value depict correlation between a variable and α angle
Discussion
To our best knowledge, this is the first study analyzing acetabular roof angle, cup offset and COR restoration simultaneously.
The results of this study confirm that the high angle of the superior roof of the acetabulum might influence cup positioning during total hip replacement. However, the only values that differ significantly from the native acetabular roof angle are the cup offset values. The reason for such observations might be subconscious thoughts to achieve proper cup fixation in the upper part of the acetabulum. That results in excessive reaming of the acetabulum. However, the restoration of the center of rotation remains unaffected by the angle of the roof of the acetabulum. Nevertheless, the subject is relevant and requires further investigation. Thus, conducting studies on a wider group of patients using different prosthesis types would help to authenticate the obtained results. Moreover, we should determine whether a surgical approach is a factor that may influence cup positioning and as a result the acetabular roof angle.
Cup placement is a highly surgeon-dependent stage of THA procedure. Since in many cases the postoperative COR differs from the native one [7, 10], it is critical to be aware of the biomechanical consequences of placement achieved after the operation. Center of rotation changes affect soft tissue tension in the hip joint and have a significant effect on abductor muscle tension. Greater trochanteric pain syndrome (GTPS) is a degenerative condition that affects the gluteal tendons and bursa, which could be one of the postoperative causes of pain in the operated hip. Currently, there is no evidence-based protocol for the management of greater trochanteric pain syndrome. Most surgeons use physical examination alone for diagnosis. A detailed analysis indicates that surgeons primarily treat GTPS with oral anti-inflammatories (57.1%), structured physiotherapy (52.4%), and glucocorticosteroid injections (45.2%) [8, 15, 16]. Additionally, the superior placement of the hip center caused delayed recovery of abductor muscle strength in hips with anterolateral minimally invasive THA. There seems to exist no biomechanical reason why the same should not also be the case for the muscle-sparing approach [17, 18].
Many research papers focus on medialization of the COR, sometimes linked with the increase in femoral offset, although the correlation between the offset and the range of motion is also under discussion [19]. Several authors claim that medialization of the COR decreases the lever arm of the body weight, which leads to reduction of the hip load [20–22]. Nevertheless, such cup positioning is negatively correlated with postoperative range of motion [23] and can lead to a variety of different issues, such as bone loss or proprioception changes [11]. What is more, THA with the COR shifted medially and posteriorly is more likely to dislocate [24]. There is an ongoing debate on how important restoration of the physiological COR actually is. For now it seems to be one of the most significant factors affecting postoperative results as it provides proper distribution of forces and reduces the wear [25]. Some authors consider that COR restoration in THA within 5 mm from its anatomical position is optimal [23].
Some authors have tried to investigate factors that may affect the success in COR restoration as it strongly impacts the final outcome of the THA procedure. Shao et al. [9] found that reaming depth had an influence on recreating the COR. However, their study had limitations as it only evaluated results based on anteroposterior radiographs. This method gives only a partial view on three-dimensional COR shift [9]. Another concept presented by Zhang et al. [26] is COR restoration based on pathomorphology of the acetabulum and Harris fossa. The authors claimed that this method is successful, but they did not describe differences of postoperative outcomes between groups with different pathomorphology [26].
As correct acetabular component placement is key to successful THA there are attempts to make this part of the procedure more precise. Kanawade et al. [27] used computer-guided instrumentation to achieve maximal precision during bone preparation and cup implantation. We may call this attempt successful as COR was restored in 81.5% of robotic assisted operations [27]. Hasegawa et al. [28] managed to obtain better accuracy of cup orientation and inclination using computed tomography-based navigation. However, other studies do not support this statement, indicating that freehand and navigated THA outcomes do statistically significantly differ in the aspect of COR restoration [29]. Our results suggest that surgeons should pay special attention to preoperative measurements of the acetabular roof angle and either adjust the intensity of acetabulum reaming or utilize computer guidance as depth of reaming is the main factor affecting COR restoration.
The current study had some limitations. The authors measured the parameters only on anteroposterior radiographs. To obtain more precise measurements, computed tomography (CT) scans may be considered as an alternative to X-rays. Moreover, a few other parameters may be gathered on different planes on CT scans. Another limitation is the size of the group of patients that were included in the analysis. A larger cohort could have made it possible to detect stronger correlations between obtained parameters. It also seems that using only the mHHS scale to assess the patient-reported outcome might not be sufficiently reliable, and the authors of this study should have added another questionnaire.
Conclusions
The study determined that acetabular cup placement in relation to the transverse axis is determined by acetabular roof angle measured preoperatively. This information can be useful for preoperative planning and risk assessment of acetabular malposition. Therefore, the study results may be helpful for adjusting the surgical technique during total hip replacement surgery for a better outcome.




