Introduction
Osteoarthritis (OA), the most prevalent form of arthritis, affects approximately 302 million individuals globally and is a leading cause of disability in older adults [1]. It is characterized by joint pathology involving cartilage degradation, bone remodeling, osteophyte formation, and synovial inflammation, resulting in pain, stiffness, swelling, and impaired joint function. As OA progresses over decades, patients often require multiple pharmaceutical and non-pharmaceutical treatments, frequently in combination [1]. Despite these interventions, OA typically worsens over time, with no available therapies to reverse the disease once initiated [2]. Addressing the broader needs of OA patients, beyond disease management, is essential for improving their overall health and quality of life [3]. Understanding these needs is critical for healthcare systems and society as a whole [2].
One of the objectives of the research was to evaluate the impact of OA on physical functionality, defined as the ability to perform basic and complex movements essential for maintaining independence and fulfilling daily roles. Impaired physical functionality can lead to reduced physical capacity, increased dependence, and diminished overall well-being. Furthermore, physical limitations are associated with an elevated risk of long-term disability [4]. Aging affects nearly all bodily systems, including joints, with OA incidence rising significantly after middle age [4]. Osteoarthritis predominantly affects older adults, who often experience comorbidities and are subject to polytherapy and polypharmacy [2]. Age may serve as a proxy for prolonged exposure to risk factors such as obesity, joint injury, and chronic joint overloading [2, 4].
Living with musculoskeletal pain extends beyond physical discomfort, significantly impacting various aspects of life, including work performance, disability, and interpersonal relationships [5]. The associated symptoms – pain, stiffness, swelling, and impaired joint function – substantially diminish the overall well-being, often leading to stress, hopelessness, anxiety, and depression [2, 6]. Although pain is not the sole symptom, it plays an important role in prompting medical consultations and influencing patients’ willingness to initiate and adhere to treatment [7]. Patients’ need to understand pain relief does not equate to disease management, emphasizing the importance of continued treatment and adherence to medical advice.
It is crucial to provide patients with comprehensive education on maintaining a healthy lifestyle, including regular physical exercise, a balanced diet, and proper weight management [8]. However, many patients, particularly in the early stages of the disease, resort to self-treatment without adequate information or rely on questionable sources. Such practices can unpredictably affect disease progression and complicate medical assessment and treatment efficacy [2]. Patients often prefer topical remedies, followed by oral medications, with faster-acting treatments being favored. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used by patients and recommended by physicians to manage joint pain [2, 9].
Given the need for long-term NSAID use in OA management, the optimal agent should combine high efficacy with a low risk of adverse events [2, 10–15].
The COVID-19 pandemic significantly disrupted OA treatment, limiting access to non-pharmacologic therapies and elective surgery due to public health measures. Concerns about interactions between OA medications and the virus further complicated care, particularly for those with severe OA, leading to a decline in health-related life satisfaction [16]. While access to healthcare was restricted, the pandemic accelerated the adoption of telemedicine and telerehabilitation, with nonurgent services delivered remotely [16–19]. Additionally, the more sedentary lifestyle during lockdowns worsened chronic pain for many OA patients [16–19].
To evaluate the impact of the pandemic on OA care, particularly regarding movement restrictions, sedentary lifestyles, limited access to healthcare consultations, and dietary changes during quarantine, we conducted quantitative research among patients in four Eastern European countries.
Material and methods
The research project consisted of two main pillars: a quantitative survey conducted among patients and a so-called Scientific Leader Team workshop with healthcare professionals (HCPs). The geographical scope of the two pillars covered four countries – Bulgaria, Romania, Serbia, and Kazakhstan – selected due to their representation of diverse healthcare environments within the Central and Eastern Europe (CEE)/Commonwealth of Independent States (CIS) region.
The patient survey included 400 participants, with 100 patients from each of the four countries. All participants had experienced chronic musculoskeletal pain due to OA for at least the past three years and were managing their pain with prescribed topical or oral medications. On average, participants reported pain in 3.7 distinct regions. Patients experiencing hip, hand/fingers, wrist, ankle, or elbow pain frequently report additional musculoskeletal pain in other areas.
Data collection was anonymous, with no personal information gathered. All participants provided informed consent. A formal ethics committee review was not sought, as the data were anonymous and non-confidential, and the topics addressed were unlikely to cause distress or require disclosure or reporting obligations.
Patients completed a quantitative questionnaire that captured sociodemographic data, subjective disease experiences, treatment behaviors, and methods of obtaining health-related information, particularly regarding OA. Additionally, the study included questions on lifestyle changes due to COVID-19. Data were collected using computer-assisted personal interviews and online questionnaires.
The research utilized a non-validated, 50-item questionnaire addressing respondents’ sociodemographic characteristics, subjective disease experiences, health information-gathering habits, and lifestyle changes due to COVID-19.
Data from the four countries were aggregated and analyzed using SPSS statistical software. Descriptive data are presented by country, with cross-tabulations employed to compare results across the four countries.
The distribution of nominal variables between countries was tested using a two-tailed χ2 test, while the Z-test was used for comparing country-specific proportions of discrete variables. Both tests were performed at a 95% confidence level, with statistical significance set at p < 0.05.
A soft launch of the patient survey was conducted, during which feedback was obtained after the completion of 10–20 questionnaires to assess any issues or challenges encountered by the respondents. Following this consultation with the interviewers, no revisions to the questionnaire content were deemed necessary based on the feedback received.
The Scientific Leader Team Workshop, a qualitative research method, is a well-proven way to share and discuss the insights of the different markets or stakeholders. To discuss the disease and the patient support opportunities with healthcare providers and understand their views about the results, a so-called Scientific Leader Team workshop was brought together, where we asked the opinion of prominent rheumatologists. We invited participants who were actively practicing in this field and who were engaged in patient-focused healthcare. The cross-country workshops were conducted on Zoom.
Gedeon Richter Plc (Budapest, Hungary) commissioned Inspira Research Ltd. (Budapest, Hungary), an independent market research agency, to conduct the regional market research study among patients. Inspira Research was responsible for the execution of the Scientific Leader Team workshop and the multi-country patient survey and the analysis of the results.
Results
People with osteoarthritis – limitations in their everyday activities
Our data indicate that individuals reporting poor or fair health status more frequently experience difficulties in performing various activities, including leisure activities, walking, standing, sitting for extended periods, lifting or carrying objects, and participating in social or outing events (Fig. 1).
The majority of respondents (over 60%) reported that impaired locomotor function negatively impacted several aspects of their daily activities (Fig. 2). In terms of pain management, rapid pain relief emerged as the top priority for respondents, particularly in patients from Kazakhstan and Serbia; 60% of participants emphasized its importance (Fig. 3). Additionally, the frequency of adverse events was higher when medications, particularly NSAIDs, were used for self-treatment rather than under medical supervision. This was especially pronounced when patients failed to consider their physical and health conditions or did not adhere to the prescribed therapeutic regimen.
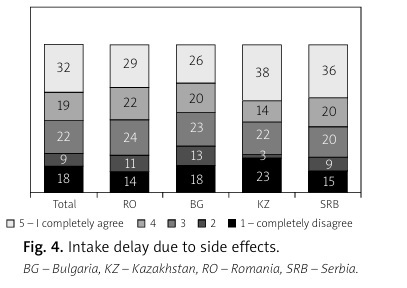
Additionally, more than 50% of patients potentially delay or skip treatment due to concerns about possible side effects (Fig. 4).
The treatment options reported were highly varied
Over-the-counter (OTC) analgesic creams and prescription (Rx) oral painkillers played the most prominent roles in managing musculoskeletal pain. While significant differences in treatment patterns were observed between countries, patients commonly employed multiple treatments concurrently (Fig. 5).
Fig. 5
Different treatment palettes were used.
OTC – over-the-counter, RX – prescription drug, TENS – transcutaneous electric nerve stimulation.

Our findings indicate that chronic pain seldom affects a single anatomical region. On average, participants reported pain in 3.7 distinct anatomical sites. Patients with hip, hand/fingers, wrist, ankle, or elbow pain were more likely to report concurrent musculoskeletal pain in other areas. Significant correlations were observed between musculoskeletal and joint pain symptoms: lower back, upper back pain, and neck pain frequently co-occurred, while limb pain often coexisted with arthritis, indicating the presence of complex, multifocal pain syndromes.
The COVID-19 pandemic significantly impacted the lifestyle of OA patients, exacerbating the burden of the disease. Patients reported reduced physical activity and increased food consumption, contributing to weight gain during the pandemic. While being overweight is already prevalent among OA patients, over half of the study sample had struggled with excess weight before the pandemic. This rate increased slightly across all countries evaluated (Suppl. Fig. 1). Weight gain and obesity are associated with poorer outcomes in OA, yet weight reduction became more challenging during the pandemic due to limited opportunities for aerobic exercise. Maintaining a healthy diet, particularly meeting protein requirements, was also identified as a major challenge during this period (Suppl. Fig. 2).
The outcomes of our research highlight that a significant proportion of OA patients experienced a worsening of their chronic condition during the pandemic. Approximately 30% of patients reported an increase in pain, irrespective of the affected body part (Suppl. Fig. 2). Patient compliance was generally high, with half of the respondents adhering strictly to their doctors’ instructions, while only about 10% did not follow recommendations. Self-treatment practices also increased, with nearly 50% of respondents stating that the pandemic prompted them to learn how to manage their symptoms independently (Suppl. Fig. 3).
Moreover, the role of online channels in OA patient care expanded during the COVID-19 pandemic, offering a valuable supplement to traditional therapy management. Before the pandemic, in-person consultations were predominant; however, remote visits, conducted via phone or online (telemedicine), became the norm across all countries. In the post-pandemic period, there is considerable variability in the extent of this shift, with the proportion of online visits continuing to rise in Serbia (Suppl. Fig. 4).
The Scientific Leader Team, in collaboration with key opinion leaders (KOLs) from the participating countries, played a pivotal role in identifying challenges in OA treatment. By leveraging the professional experiences of KOLs, the team aimed to pinpoint areas requiring improvement that affect OA patients and are considered significant by these healthcare professionals.
The involvement of the Scientific Leader Team was particularly crucial at two key stages of the research:
Insight-Generating Workshop: Before conducting the patient survey, an insight-generating workshop was held to provide a comprehensive overview of the OA therapeutic landscape. This included detailed discussions on patient flow, patient characteristics, and treatment patterns. The KOLs contributed objective clinical insights, complementing the subjective experiences shared by patients. The findings from this workshop informed the development and finalization of hypotheses and the survey questionnaire for the subsequent quantitative research phase.
Post-Survey Analysis and Validation: Following the patient survey, the Global Research stakeholder team, which included brand and category managers, collaborated with KOLs to validate or challenge the initial hypotheses. This phase allowed for a comparative analysis of country-specific findings, resulting in the identification of opportunities to improve patient education, optimize patient flow, and refine treatment strategies.
The contribution of the Scientific Leader Team was instrumental in consolidating the survey results, revealing both common and region-specific unmet needs. Key findings included limitations in effective pain management, inadequate access to comprehensive care (such as lifestyle counseling), and the need for improved patient-centered treatment approaches. These insights can inform the development of educational programs for patients, focusing on appropriate medication use and lifestyle modifications.
Additionally, the study highlighted the potential of technology to support OA patients in self-managing their condition. The KOLs affirmed that technological tools can provide effective guidance for pain management, lifestyle adjustments, and monitoring of chronic conditions, thereby improving patient outcomes.
Discussion
Our research project aimed to identify and understand the specific burdens and personal needs faced by individuals with OA and the impact of the COVID-19 pandemic. The results of our study indicate that a holistic and well-coordinated approach to OA, supported by collaborative efforts among healthcare systems, patients, and their families, is essential. Promoting interdisciplinary care and focusing on daily activities and environmental factors can enhance physical functioning and overall health status.
OA commonly develops and worsens with age. It often coexists with other conditions that negatively affect patients’ general health [4]. Our findings emphasize this concern, revealing that over 60% of respondents reported poor musculoskeletal conditions adversely impacting their daily activities. Osteoarthritis symptoms typically progress gradually [7]. In the early stages, patients often experience mild to moderate symptoms, which they may attempt to manage through avoidance, underestimation, or self-medication [8]. Pain remains the most distressing symptom for individuals living with OA [8], with more than 50% of patients in our study expressing a desire for rapid pain relief from their treatment.
Patients require reassurance regarding the safety of treatments, in addition to their effectiveness in alleviating symptoms [10, 14]. Nonsteroidal anti-inflammatory drugs are frequently utilized for their anti-inflammatory, antipyretic, and analgesic properties [10] and are recommended as a first-line therapeutic approach for managing OA [1]. One of the primary factors influencing patients’ decisions to initiate, accept, and adhere to NSAID therapy is the potential for adverse gastrointestinal effects [12, 13]. Given the necessity for long-term NSAID treatment in OA, the ideal medication should demonstrate strong efficacy, particularly in pain relief, while minimizing the risk of adverse gastrointestinal events.
The COVID-19 pandemic has impacted nearly all aspects of OA management [16]. In our study, approximately 30% of participants reported an increase in musculoskeletal complaints following the lifestyle changes associated with the pandemic. Furthermore, the role of online channels in OA patient care has evolved; our findings indicate that the proportion of visits conducted via online platforms fluctuated from 5% before the pandemic to 12% during the pandemic, returning to 9% after the pandemic.
The Scientific Leader Team, along with key opinion leaders (KOLs) from participating countries, identified challenges in OA treatment based on KOLs’ professional experiences. The study revealed unmet needs, such as inadequate pain management and access to comprehensive care, and highlighted the potential of technology to support OA patients in self-management.
Bulgaria, Romania, Serbia, and Kazakhstan were selected due to their representation of diverse healthcare environments within the CEE/CIS region. This diversity provided insight into how varying healthcare infrastructures and economic conditions impact the availability and accessibility of treatments for chronic musculoskeletal pain. The results show that, despite similar pain perceptions, attitudes toward healthcare, pain management, and medication use differ significantly across these countries, shaped by their distinct economic, cultural, and healthcare systems.
Study limitations
This study has some limitations. This patient survey presents the findings from an analysis conducted across Bulgaria, Romania, Serbia, and Kazakhstan. Future research focused on clinical outcomes would offer deeper insights, particularly if extended to a wider range of countries. Furthermore, a detailed analysis of the study population’s characteristics – including age, sex, body mass index, disease duration, and the specific joints involved – would improve the robustness of the findings. Including additional demographic and clinical variables, such as comorbidities (e.g., osteoporosis, obesity, cardiovascular, and gastrointestinal conditions), would also enhance the understanding of health outcomes.
Conclusions
Individuals with OA face significant limitations in their daily activities, with a predominant desire for prompt pain relief. Many patients are hesitant to seek treatment due to concerns about potential side effects. The use of multiple treatment modalities is common, with over-the-counter analgesic creams and prescription oral painkillers playing key roles in managing musculoskeletal pain. The COVID-19 pandemic has further influenced patients’ lifestyles, leading to increased food consumption and decreased physical activity, which negatively impacted OA symptoms and exacerbated chronic pain. Additionally, there has been a notable rise in the utilization of online channels for OA patient care during the pandemic. These findings underscore the need for tailored treatment approaches that prioritize effective pain management while addressing patients’ concerns about safety and side effects.