Introduction
Total knee arthroplasty (TKA) is considered one of the most successful orthopaedic procedures. Patient satisfaction varies from 75 to 90% and depends on both non-surgical and surgical factors. Among non-surgical factors are socio-economic status, mental health, general physical condition, and patient’s expectations [1–3]. Within surgical factors one of the most difficult preoperative decisions is the choice of implant type. In this study surgeons focused on the two most common types of implants: cruciate retaining (CR) and posterior stabilized (PS). Orthopaedic surgeons select the type of prosthesis based on their own experience and subjective clinical examination of the patient’s knee. Use of either the CR or PS implant can be chosen preoperatively with possible conversion during the procedure depending on the intraoperative posterior cruciate ligament (PCL) efficiency [4–6].
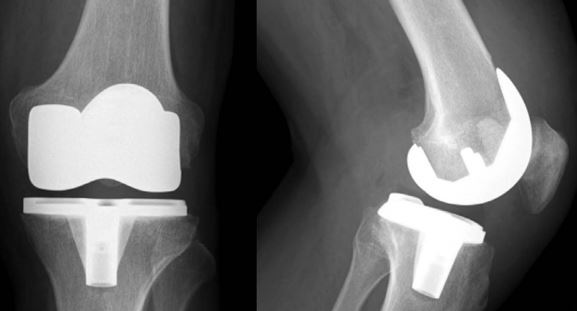
In Figure 1 A and B the postoperative X-rays are presented.
Fig. 1
Postoperative X-rays depicting both implants described in the text: A) posterior stabilized; B) cruciate retaining.

Cruciate retaining and PS are two types of prosthesis that differ in the mechanism providing sagittal and rotational stability. The CR implant relies on sufficient PCL. Its main advantages include lesser forces being transferred between the bone and the cement, improved proprioception, kinematics, and bone preservation. In comparison, utilizing the PS implant requires a total resection of the PCL. The prosthesis allows easier ligament balancing, has a conforming articulation, allows for a wider range of knee flexion, has more predictable kinematics and reproducible rollback, and a lower range of axial rotation and condylar translation. Another advantage of the PS implant is elimination of the risk of progressive PCL insufficiency, which, among CR prosthesis treated patients, leads to dramatic deterioration in knee kinematics [7–11].
Standard radiographic evaluation for patients undergoing primary TKA includes a weight-bearing AP and lateral knee X-ray imaging and patellofemoral joint view, such as the skyline view. Long leg radiographs are not performed routinely at every institution; many authors consider them obligatory in preoperative planning, especially in complex cases with significant mechanical axis deviation or anatomical abnormalities [12, 13].
Computed tomography (CT) and magnetic resonance imaging (MRI) are rarely indicated in primary TKA planning. Computed tomography can be invaluable when use of an implant of an unconventional size is planned. It helps assess the desired size and whether a custom-made implant is required. When patient-specific instrumentation and/or custom implants are considered, an MRI and CT are required in the production process [14].
On the other hand, in assessment of PCL efficiency radiography, ultrasound, and computed tomography all have clinical value, but MRI remains the gold standard. Only MRI and posterior stress radiographs were proved to be objectively reliable [15, 16].
The most accurate physical test for PCL efficiency is the posterior drawer test, but other tests such as Muller’s test or the dynamic posterior shift test may aid the diagnosis [17, 18].
The most common type of PCL insufficiency among patients with osteoarthritis (OA) is chronic insufficiency, which typically results in posterior tibial translation [19].
The aim of this study was to investigate the relationship between the posterior subluxation of the tibia on preoperative radiograms and implant type used. The choice of implant type was made upon intraoperative PCL assessment. The secondary aim was to evaluate the correlation between patients’ demographic data (sex, age) and implant type.
Material and methods
This study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement [20] and an appropriate checklist was presented to the editors. Informed consent was obtained from all subjects involved in the study.
Patients included in the study were 1) > 50 years of age, 2) had clinically and radiologically confirmed primary OA of grade IV on the Kellgren-Lawrence scale, and 3) were undergoing primary TKR with a PS or CR implant without patellar resurfacing. Exclusion criteria were: history of lower limb surgery (fractures, previous surgery), patients with rheumatoid arthritis, patients without complete radiologic examination available for review (lateral X-rays), patients with a history of PCL injuries, collateral ligament instability.
A consecutive series of patients were evaluated and operated on by two fellowship-trained surgeons in the level IV academic hospital between 2021 and 2022. They were operated on with on-label use of PERSONA PS and CR (Zimmer-Biomet, Warsaw, IN) total knee implants without patella resurfacing as a treatment for end-stage knee OA. PCL condition was examined intraoperatively.
Radiographic evaluation
Preoperative lateral radiographs were analysed retrospectively. All images were weight-bearing and taken at 10–15 degrees of flexion. Retrospective analysis of the images was performed.
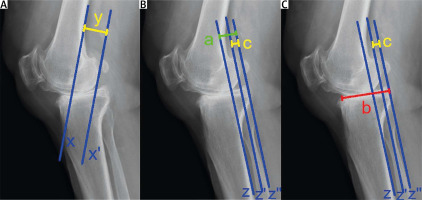
Three parameters were measured:
ratio between the length of the part of tibial plateau posterior to the line of posterior femoral condyles and the length of the tibial plateau (calculated as the percentage of subluxation),
ratio between the length of the part of plateau posterior to the line of the posterior femoral condyles and the part of the plateau posterior to the line of the posterior tibial cortex,
posterior condylar offset measured as the length of the line between the posterior femoral cortex and the posterior femoral condyles (Fig. 2).
Statistical analysis
Statistical analysis of results was performed. All comparisons were performed between continuous variables. Due to significant deviation from normality of distribution, the Mann-Whitney U test was used for comparisons between the groups and Spearman’s correlation coefficient was used to assess the correlation between age and given variables. For categorical variables Fisher’s exact test was used. The significance level was set at an α value below 0.05. All statistical analyses were conducted using SAS software, Version 9.4 for Windows (SAS Institute Inc., NC, USA).
Fig. 2
Measurements described in the text above as I (c/b × 100%), II (c/a) and III (y): A) the part of the plateau posterior to the line of the posterior tibial cortex; B) length of the tibial plateau; C) length of the part of the tibial plateau posterior to the line of the posterior femoral condyles; y – length of the line between the posterior femoral cortex and the posterior femoral condyles.
Results
Radiographs of 100 patients were measured postoperatively. Within this group, 70 arthroplasties were performed using PS and 30 using the CR implant type.
Analysis of measured parameters revealed that 52 patients had posterior tibial subluxation.
Another 48 patients had anterior tibial subluxation and were excluded from calculations.
Baseline characteristics of the participants are depicted in Table I.
Table I
Baseline characteristics of patients included in the analysis. The bold value is statistically significant
There was no statistically significant difference between CR and PS groups with regard to percentage ratio of the part of the plateau posterior to the line of the posterior condyles to the length of tibial plateau (6.6 [4.1–12.2] vs. 5.5 [3.6–10.0], p = 0.6), the ratio of the part of the plateau posterior to the line of the posterior condyles and the part of the plateau posterior to the line of the posterior tibial cortex (28.9 [11.8–35.7] vs. 19.4 [11.1–27.8], p = 0.4) and posterior condylar offset (PCO) (29.0 [24.0–31.0] vs. 28.5 [27.0–32.0], p = 0.8). Additionally, there was a significant difference between the groups with regard to mean age (68.5 [60.0–72.0] vs. 72.5 [68.0–75.0], p = 0.006). However, there was a non-significant, very weak negative association between age and parameter D (rs = –0.17, p = 0.24) and between age and parameter E (rs = –0.14, p = 0.31) (Table II).
Table II
Comparison of mean values of measured parameters. The underlined value is statistically significant
[i] CCR – cruciate retaining, D – percentage ratio between the part of the plateau posterior to the line of posterior condyles and the length of the tibial plateau, E – ratio of the part of the plateau posterior to the line of the posterior condyles and the part of the plateau posterior to the line of the posterior tibial cortex, PCO – posterior condylar offset, PS – posterior stabilized.
Discussion
The appropriate choice of implant type is necessary to fully capitalize on the advantages of a particular design. Defining objective criteria for use of each type could help surgeons in the process and decrease the number of intraoperative conversions.
It was reported that the rate of intra-operative conversions from CR to PS in TKAs ranged from 9.9% to 17.0% [21, 22]. One of the reasons for such conversions, apart from iatrogenic PCL injury, is intraoperatively detected ligament insufficiency. Changing the implant type during the surgery lengthens the procedure, which is a proven risk factor of periprosthetic infections and thromboembolic complications [23–26]. It also plays a role in the department’s financial efficiency and implant ordering logistics as both types need to be available during the surgery along with implant specific instrumentation.
It is recommended that surgeons envision the selection between CR and PS in the preoperative plan based on history, physical examination and imaging, taking into account both the advantages and disadvantages of implant designs [27, 28].
According to Jackman et al. [29], the kneeling technique of stress radiography is inexpensive and reliable in quantifying posterior knee laxity and it could become a standard of objective pre-operative PCL evaluation. It is important to note that this type of radiograph is not typically used in preoperative planning and thus an additional X-ray would need to be taken, which is associated with additional exposure to radiation [30]. Nonetheless, the benefits of more precise preoperative planning by far outweigh the potential risk associated with exposure to ionizing radiation.
In this study, the surgeons intraoperatively decided which kind of implant would be suitable for the patient after examination of the PCL. If the PCL was in a good condition, the CR type of implant was chosen, whilst when the PCL was insufficient, the PS type of implant was used.
Our study found that tibial subluxation measured on weight-bearing radiograms cannot play a role in evaluation of PCL sufficiency. As a consequence, it is not useful in choosing the implant type.
During this study we also discovered a significant correlation between patient’s age and implant type used. That is consistent with the results of other papers stating that the risk of chronic PCL insufficiency is correlated with patient’s age.
In Figure 3 a diagram with the implant selection methodology is presented.
Fig. 3
Diagram showing the way of choosing the final type of implant.
CR – cruciate retaining, PCL – posterior cruciate ligament, PS – posterior stabilized.

The current study had some limitations. First, it had a retrospective study design with a limited level of evidence. Performing a prospective randomized-controlled trial could have improved the scientific value of this study. The measurements were performed in a neutral, non-forced position; a different technique of visualization might be more appropriate to assess the condition of PCL. Moreover, the study group could have been larger, so the study would have been more reliable and valuable for further investigations.
Conclusions
Currently the choice of implant type is based on intraoperative assessment of PCL function. Manual examination is not considered as an objective measure and is not quantifiable. Developing a radiological method of presurgical assessment would allow for an objective and potentially more adequate choice of implant. It could also be cost-effective as only one implant type and instrumentation would be needed during surgery. This study revealed that preoperative posterior tibial translation measured on weight-bearing X-rays does not significantly correlate with the choice of implant type and so probably not with the PCL function and efficiency either. As a result, we conclude that it cannot be used as a substitute of the intraoperative functional assessment in the implant selection process. Additionally, this study showed that PCL insufficiency is related to age, as the group of patients with the PS implant had a significantly higher mean age than in the CR group. More studies are needed to find a way to objectively assess the PCL function before the surgery without additional exposure to potentially harmful radiation.