Introduction
Rheumatic diseases are chronic, systemic conditions that affect the musculoskeletal system, characterized by remissions and acute attacks with varying clinical courses and symptoms. This scope encompasses not only rheumatic, inflammatory, and systemic diseases but also degenerative joint and spine diseases, soft tissue rheumatism, and metabolic bone diseases. More than 200 rheumatic diseases have been identified, including rheumatoid arthritis (RA), osteoarthritis, ankylosing spondylitis (AS), fibromyalgia, and gout [1].
Rheumatic diseases pose significant health problems in terms of causing mobility limitations and disabilities, loss of workforce, and treatment and care costs. Rheumatic diseases are present in approximately one-third of individuals with physical disabilities, constituting the most common cause of physical disability in the elderly. With the increasing aging population, it is predicted that the prevalence of rheumatic diseases and associated activity limitations will rapidly increase in the coming years [2].
Rheumatic diseases affect the individual as a biopsychosocial entity. Individuals with rheumatic diseases often experience physical symptoms such as joint pain, loss of mobility, arthritis, inflammation, lung and heart involvement, as well as psychological and social issues including insomnia, fatigue, anxiety, and depression. These diseases can significantly limit daily life activities, restrict individuals’ ability to work, participate in social and leisure activities, and seriously affect their overall functioning and quality of life [2].
Rheumatic diseases are chronic conditions, and rather than focusing solely on disease treatment, the emphasis is placed on disease management. Individuals with rheumatic diseases should maintain disease management throughout their lives. With advancements in drug therapies, there is also a need for development in the field of rheumatological rehabilitation. In recent years, there has been increasing recognition of the importance of biopsychosocial approaches in the active management of chronic diseases, wherein the patient plays a role. According to the biopsychosocial model, individuals with chronic diseases should aim not only to improve their physical functions, such as musculoskeletal system problems, but also to enhance their overall health status, psychological, and social well-being [3]. Therefore, in the rehabilitation process, there is a need for a multidisciplinary and interdisciplinary treatment team to reduce the symptom burden of the disease, increase independence, and maximize the quality of life. In some countries, a rheumatology team consisting of various specialists such as rheumatologists, physiotherapists, rehabilitation nurses, occupational therapists, psychologists, and social workers work together in an interdisciplinary approach. This multidisciplinary and interdisciplinary rheumatological rehabilitation profile contributes to clinical effectiveness and reduces treatment costs [3].
In rheumatic diseases, the collaboration between rheumatologists and physiotherapists in the early stages of the disease and the implementation of physiotherapy and rehabilitation practices tailored to the stages of the disease are of critical importance [4]. Physiotherapy programs initiated in the early stages can be effective in preventing joint deformities, reducing activity limitations, and preventing further joint damage. Additionally, pulmonary physiotherapy, applied in addition to pharmacological treatment for disease-related lung diseases, has shown positive effects on dyspnea, fatigue, functional exercise capacity, and quality of life [3, 4].
Individualized emotional and cognitive psychological interventions that increase patients’ awareness of emotional regulation and coping strategies can help improve their long-term functioning and quality of life. In this context, treatment education programs should be supported by home exercises and both individual and group sessions [3, 4]. Considering the effectiveness and complexity of rheumatological physiotherapy and rehabilitation, increasing awareness and knowledge in this field nationwide in Turkey is an important necessity. Our study, designed to examine the biopsychosocial conditions of patients hospitalized in the rheumatology service of a university hospital, aims to contribute to this goal.
Material and methods
Participants
Ninety-six patients receiving inpatient treatment at the rheumatology service of a university hospital were included in our study. Inclusion criteria were: being 18 years of age or older, and having a diagnosed rheumatic disease. Patients with missing data for any reason and those not admitted to the rheumatology service were excluded from the study.
Assessment
A form was created to record the following information of the individuals included in our study: name, surname, age, height, weight, sex, dominant side, diagnosed rheumatic disease, duration of disease, accompanying diseases if any, length of hospital stay, history of previous admissions to the rheumatology service, employment status, smoking, ambulation level, use of assistive devices and exercise habits.
Chest circumference measurement: Respiratory function is an important parameter in monitoring and evaluating respiratory functions. Measurement was taken from the level of the fourth rib passing under the lower end of the scapula with abduction of the arms while standing. Measurement was performed twice during rest, inspiration, and expiration [5].
Respiratory rate: Respiratory rate provides important information for diagnosing respiratory problems and the individual’s overall health status. The number of breaths taken by the individual in one minute (how many times the chest rises) was counted. During assessment, the hands were placed on the patient’s chest to feel the movements occurring on the chest wall, and the counts during rest, inspiration, and expiration were evaluated [6].
Manual muscle testing: Manual muscle testing is used to assess an individual’s muscle strength and identify any potential weakness or imbalance [7]. The strength of large muscle groups such as the quadriceps femoris and biceps brachii is necessary for individuals to maintain their daily activities. Weakness in these muscles can negatively affect a person’s independence and quality of life. In our study, muscle strength was evaluated with a score between 0 and 5 (0: no contraction can be felt in the muscle, 5: full motion of the segment against gravity and maximal resistance).
Visual Analogue Scale (VAS): The VAS includes a scale with a starting and an end point on a line for evaluating a specific characteristic [8]. Individuals assess the severity of their condition by placing a mark on this line. On this scale, 0 indicates the absence of a specific characteristic or no sensation, while 10 represents the highest intensity of that characteristic. It was used in our study to assess general well-being.
Fatigue Severity Scale (FSS): The scale consists of 9 questions and is unidimensional. Armutlu et al. [9] conducted the Turkish validity and reliability study for the scale. Individuals indicate their level of agreement with the items on the scale by selecting a number from 1 (completely disagree) to 7 (completely agree). The total score is evaluated as the average of all responses. A score of ≥ 4 on the scale is considered fatigued, while a score of < 4 is considered not fatigued.
Rivermead Mobility Index (RMI): The RMI is an index used to measure mobility status, including basic mobility activities. It consists of 14 questions answered by the patient and 1 question based on the observer’s observation. It covers activities ranging from turning in bed to running. The RMI was primarily developed to evaluate the outcomes of physiotherapy and rehabilitation practices following head injuries and strokes. A score of 1 point is given for “yes” answers, and 0 points for “no” answers. The total score ranges from 0 to 15. As the score increases, the individual’s level of mobility also increases. Akın et al. [10] demonstrated that the RMI is valid and reliable in Turkish.
Beck Anxiety Inventory (BAI): It is a 21-item self-assessment scale scored between 0 and 3. According to the scores obtained from the scale, patients’ anxiety levels are classified as low (0–7 points), mild (8–15 points), moderate (16–25 points), and severe (26–63 points). A high score indicates a high level of anxiety experienced by the individual. The Turkish validity and reliability study of the scale was conducted by Ulusoy et al. [11].
Nottingham Health Profile (NHP): The NHP is a general health questionnaire consisting of 6 sub-parameters including energy level, emotional reactions, physical mobility, pain, sleep, and social isolation, and a total of 38 items. The answers to the questions are given as “yes” or “no” according to the perception of the current situation. The total score ranges from 0 to 100, with a higher score indicating a lower perceived quality of life related to health. The Turkish validity and reliability study of the scale was conducted by Küçükdeveci et al. [12].
Statistical analysis
The data were analyzed using the SPSS 25.0 package program. Continuous variables were given as mean ±standard deviation, and categorical variables were given as number and percentage. The normal distribution of the data was examined using the Kolmogorov-Smirnov Z test. The relationship between evaluation parameters was examined using Pearson correlation analysis when parametric test assumptions were met, and Spearman correlation analysis was used in non-parametric conditions. A significance level of p ≤ 0.05 was accepted and interpreted in statistical test results.
Results
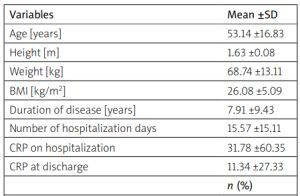
The demographic characteristics of the 96 patients admitted to the university rheumatology service were analyzed (Table I).
Table I
Demographic and disease-related data of patients
Of the patients, 64.6% (n = 62) were female, and 35.4% (n = 34) were male. The mean age of the patients was 53.14 ±16.83 years, with a mean height of 1.63 ±0.08 m and mean weight of 68.74 ±13.11 kg. The mean disease duration of patients was 7.91 ±9.43 years. The average length of hospital stay was 15.57 ±15.11 days (Table I).
Regarding employment status, 39.6% (n = 38) of the patients were employed. Smoking was reported in 12.5% (n = 12) of the patients. Physical exercise habits were present in 21.9% (n = 21) of the patients, and 43.8% (n = 42) had a history of previous admissions to the service. In terms of ambulation level, 5 patients (5.2%) were at bed level, 4 patients (4.2%) at sitting level, 7 patients (7.3%) at standing level, and 80 patients (83.3%) were at walking level. The rate of assistive device use in mobilization was 17.7% (n = 17) (Table I).
When patients’ general well-being was assessed with the VAS, the mean score was 6.03 ±2.51. Their average respiratory rate was 22.55 ±6.03 breaths per minute. The average chest circumference measured at the level of the fourth rib was 97.01 ±9.70 cm at rest, 99.71 ±9.67 cm at inspiration, and 94.10 ±13.91 cm at expiration. Regarding the respiratory pattern, 11.5% (n = 11) exhibited abdominal, 24% (n = 23) exhibited thoracic, and 42.7% (n = 41) exhibited mixed type respiration (Table II).
Table II
Clinical presentation of patients
The mean quadriceps muscle strength was 4.26 ±0.74 on the right and 4.16 ±0.76 on the left. For the biceps brachii, the mean muscle strength was 4.46 ±0.64 on the right and 4.39 ±0.78 on the left. Mobility level assessed by RMI had a mean value of 11.41 ±4.11 (Table II).
The total NHP quality of life score for patients was 39.18 ±22.44, with subparameters as follows: energy level 52.89 ±37.06, pain level 39.07 ±33.76, emotional reactions 33.13 ±30.0, social isolation 25.01 ±29.36, sleep 45.03 ±28.69, and physical mobility level 39.41 ±29.03 (Table II).
Fatigue level, assessed by FSS, had a mean score of 4.27 ±1.90. Anxiety level had a mean score of 15.12 ±9.87, with 69.8% (n = 67) classified as mild, 21.9% (n = 21) as moderate, and 2.1% (n = 2) as severe anxiety (Table II).
Discussion
In the present study, the biopsychosocial assessment was conducted on 96 patients diagnosed with rheumatic diseases and hospitalized in the rheumatology service of a university hospital. The patients admitted to the rheumatology service had decreased inspiratory capacity, elevated respiratory rates, average levels of mobility and energy, and significant levels of fatigue and anxiety that needed attention, all of which could negatively affect their overall condition.
For preservation and enhancement of health it is necessary to consider biological, psychological, and social characteristics together and focus on protective factors aimed at improving biological, psychological, and social living conditions. Factors such as improving healthcare services, ensuring accessibility to education, increasing welfare, maintaining a happy family life, having a satisfying profession, and ensuring security may influence health outcomes [13].
Muscle strength is a critical factor for healthy living, functional performance, and quality of life. Research indicates that muscle strength decreases by 25–70% in patients with RA following the development of interstitial lung disease, compared to healthy individuals [14]. This situation emphasizes the association of low muscle strength with activity limitation, increased levels of fatigue, and decreased quality of life [15]. In RA patients, atrophy due to disuse associated with symptoms and the impact of RA on the sarcotubular system, mitochondria, and myofibrils result in decreased skeletal and respiratory muscle strength [14]. Our study revealed a decrease in the strength of the quadriceps and biceps brachii muscle groups. It is important to perform strengthening and stretching exercises targeting major muscle groups to maintain daily life activities, reduce complications, and support overall health and well-being.
Rheumatic diseases commonly lead to postural problems due to their impact on the lungs. Increased thoracic kyphosis, widening of the chest anteroposterior diameter, shoulder protraction, and increased trunk flexion are some of the frequently encountered postural problems. These postural abnormalities result in increased respiratory workload by causing a reduction in pulmonary function. Decreased lung flexibility and airflow restriction due to inflammation and fibrosis in the lungs can lead to decreased inspiratory capacity [16]. This explains the elevated respiratory rates and decreased inspiratory abilities observed in our study. Specialized practices in pulmonary physiotherapy, a subfield within physical therapy and rehabilitation, assist in treating symptoms associated with lung involvement such as dyspnea, secretion accumulation, pain, fatigue, decreased exercise tolerance, and postural problems [17].
Periodic and persistent pain is a fundamental emotional challenge for individuals with rheumatic diseases. It is evident that these negative effects can lead to psychosocial adjustment problems. As with any illness, the primary obstacle in rheumatic diseases is adapting to the disease and treatment. Rheumatic diseases necessitate a continual adaptation process by adversely affecting individuals’ functions and overall well-being. Various issues such as regression in interpersonal relationships with family and friends, depression or emotional distress, economic difficulties, and caregiving needs may arise, impairing the quality of social interactions [18]. Research indicates that individuals with rheumatic diseases experience psychological issues more frequently than the general population. Patients with RA have a high risk of anxiety, depression, and suicide, along with low self-esteem. In a study by Kłak et al. [19], it was reported that approximately half of the patients experienced dysfunction in social interaction, communication with others, and emotional behavior. Another study observed that rheumatic diseases have a diminishing effect on marital satisfaction [20]. In our study, the moderate level of overall well-being among patients may indicate the influence of the disease on emotional status. Decreased social support networks due to hospitalizations lead to reduced activity levels and mobility, which may result in a sedentary lifestyle, weight gain, depression, and a decreased sense of well-being. Research suggests that these psychological factors are associated with negative outcomes in terms of disease severity and activity, as well as increased pain, fatigue, and functional impairment [21].
Fatigue represents a significant economic burden and unmet need for both patients and society. It has been defined as one of the most challenging symptoms to manage for patients with inflammatory rheumatic diseases and is associated with low quality of life [22]. Fatigue is also a significant independent predictor of work loss and disability in patients with RA, AS, systemic lupus erythematosus (SLE), primary Sjögren’s syndrome (pSS), and vasculitis. Patients with fatigue often report feeling weak in their muscles and being unable to sustain prolonged or intense activity. Decreased muscle strength and endurance correlate with disease activity in patients with inflammatory arthritis and are associated with reduced physical activity. Sarcopenia (reduced muscle mass) and myositis (muscle inflammation) can be observed in many inflammatory rheumatic diseases, contributing to fatigue [23, 24]. In our study, fatigue symptoms were present in 63.5% of our patients, highlighting the importance of assessing fatigue levels. Therefore, understanding the underlying mechanisms, identifying modifiable psychosocial factors, and understanding their contribution to treatment are crucial for making effective treatment decisions.
In a cross-sectional study, female patients with pSS were observed to have lower maximal oxygen consumption (VO2max), muscle strength and function, and higher levels of fatigue compared to age and habitual physical activity-matched healthy women [25]. However, in a randomized controlled trial involving supervised walking in pSS patients, improvement in VO2max and cardiovascular fitness was found to be associated with decreased fatigue and depression [26]. A study comparing the effectiveness of different exercise methods in patients with RA observed significant improvements in fatigue status in all groups [27]. Additionally, it is believed that Pilates exercises, by activating the parasympathetic nervous system through respiratory control, may enhance overall well-being and have positive effects on physical and mental fatigue [28].
Physical activity in rheumatic diseases can vary depending on the severity of symptoms, type of disease, and overall health status of the individual. In our study, patients’ mobility levels were at average values. 83% were at the walking level, and 17.7% required assistance devices for mobilization. 78.1% of patients did not have regular physical exercise habits. A study examining 443 patients with RA showed that 78% of patients were generally inactive or had low levels of physical activity. Physical fatigue is the strongest determinant of decreased physical activity in RA. Researchers have suggested that physical activity may potentially improve fatigue in RA patients, but the effect size is small to moderate [29]. Studies in patients with SLE have shown that home exercise programs conducted for 8–12 weeks resulted in decreased fatigue, and if participants continued to exercise, this decrease continued for 3 months [30].
The symptoms of rheumatic diseases typically include pain, swelling, stiffness, and limited mobility. These symptoms can negatively impact daily life and restrict a person’s functionality. Additionally, the necessity to cope with chronic pain and make lifestyle changes can lead to emotional reactions such as stress, anxiety, and depression [31]. Challenges in disease management, side effects, failure to achieve expected outcomes, and uncertainty about the future can also increase anxiety. While dealing with pain and stiffness that limit daily activities, individuals may also encounter difficulties in areas such as work, family, and social life, negatively affecting their quality of life. Anxiety has been associated with more severe depressive symptoms, worse functional disability, a higher number of tender joints, more severe pain, and increased fatigue [32]. In our study, significant decreases in mild to moderate anxiety and quality of life were observed in patients. Therefore, recognizing the interconnectedness of the medical, emotional, and behavioral aspects of the disease is crucial for developing appropriate interventions to improve patients’ quality of life.
Research conducted in the last 20 years emphasizes the importance of a holistic approach in the treatment of rheumatic diseases [33]. In a study examining the biopsychosocial characteristics of 20 patients with AS, many factors such as disease activity, fatigue, quality of life, sleep hygiene, kinesiophobia, and anxiety/depression were found to be moderately to highly correlated, highlighting the need for approaches that encompass these factors in the treatment program [34]. Improvements in quality of life were observed in patients and healthy individuals with mild to moderate group exercises. Bize et al. [35] found a significant relationship between individuals’ level of physical activity and health-related quality of life. Significant improvements in the biopsychosocial conditions and depression levels of individuals practicing Pilates were observed during the coronavirus disease 2019 (COVID-19) pandemic [28]. Electronic cognitive behavioral therapy approaches have been shown to improve psychological distress in RA and anxiety and quality of life in psoriasis [36, 37]. While reformer Pilates exercises have positive effects on disease activity and muscle strength, home-based mat Pilates exercises have been reported to have positive effects on the number of painful areas, disease activity, biopsychosocial condition, and physical component of quality of life [38].
In the management of rheumatic diseases, comprehensive approaches and patient and family education are necessary [39]. These may include behavioral interventions such as weight management, improving sleep hygiene, psychological interventions related to stress, anxiety, and depression, increasing physical activity, exercise, smoking cessation, and enhancing coping skills. Programs aimed at reducing social isolation can also be beneficial. If patients learn to effectively manage their emotions, thoughts, and behaviors, they can become active participants in controlling their well-being. In this way, they can increase their coping abilities, leading to more balance and peace in their lives [40].
The data obtained from our study suggest that evaluating individuals’ biopsychosocial characteristics in disease management can contribute to optimizing the benefits obtained from treatment, considering the chronicity of rheumatic diseases and their impact on various bodily functions. This assessment process allows for the design of personalized treatment plans by not only addressing the patient’s physical symptoms but also considering psychosocial and environmental factors. Additionally, our study may contribute to improving treatment processes through increased awareness and understanding of the roles and capabilities of physiotherapists, fostering more effective collaboration between rheumatologists and physiotherapists, and enhancing patient referrals.
The strengths of our study lie in its high statistical power and being one of the few studies examining biopsychosocial approaches in the management of rheumatic diseases. Participants were recruited from the inpatient rheumatology service at a university, which may limit the generalizability of the findings to some extent. However, it also provides a specific and focused sample for analysis. Future research efforts are warranted to further elucidate the role of the biopsychosocial model in effective treatment strategies for rheumatic diseases.
Conclusions
Inspiratory capacity of patients hospitalized in rheumatology service is low. Their respiratory rate is higher than normal. Their mobility and energy levels have average values, while fatigue and anxiety levels need to be considered. In addition to pharmacological treatments, we recommend that patients hospitalized in rheumatology service be supported by appropriate exercises provided by physiotherapists.