Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune condition characterized by synovial inflammation, which results in joint destruction. Compared to the general population, individuals affected by RA have significant morbidity, with RA impacting physical and social functioning, ability to work and emotional wellbeing [1]. In Morocco, the prevalence of RA is on the rise, presenting an escalating burden on the healthcare system. Epidemiological data underscore the considerable impact of these diseases on patient quality of life, necessitating a multidisciplinary approach to their management [2].
Traditionally, the management of RA has been focused on medication-based treatments aimed at controlling inflammation and alleviating symptoms. However, a holistic approach, integrating non-pharmacological interventions, has become essential to enhance patients’ quality of life. Non-pharmacological management (NPM), including tailored physical activity, rehabilitation, nutrition, and stress management, can effectively complement medical treatments, promoting improved joint functionality, reduced fatigue, and overall well-being enhancement [3–8].
It is imperative to understand attitudes, practices and perceived barriers to implementing NPM of RA. Assessing these aspects will provide an accurate overview of the situation in Morocco, thus contributing to the development of strategies and recommendations tailored to the local reality, and will help to promote an integrated approach in the management of patients with RA.
The aim of this study, initiated by Rheumatology Department B and its association Moroccan Association for Research and Scientific Assistance to Rheumatic Patients (AMRAR), was to assess the level of integration of NPM by Moroccan rheumatologists for RA, to identify their attitudes, practices and their perceived barriers towards its implementation and to analyze the factors associated with the lack of integration of non-pharmacological treatment by rheumatologists in the Moroccan context.
Material and methods
Study design and population
We conducted a national cross-sectional, web-based study among Moroccan rheumatologists from January 15 to February 30, 2024.
Study eligibility criteria
The inclusion criteria were as follows: all rheumatologists practicing in Morocco, whether in the public, private, or university sectors. There were no exclusion criteria.
Sampling strategy
This was an exploratory and comprehensive study targeting all rheumatologists currently practicing in Morocco. We did not use a sampling method as the questionnaire was disseminated to all practicing rheumatologists via email addresses provided by the Moroccan Society of Rheumatology (la Société Marocaine de Rhumatologie – SMR).
Data collection
The survey was online-based and self-administered. We collected the data through the online survey tool Google Forms. An email list of all Moroccan rheumatologists (440 rheumatologists) was provided by the SMR, which has a database containing the e-mails of all rheumatologists practicing in Morocco. An e-mail detailing the study’s purpose and process, along with a survey link, was sent to all rheumatologists on January 15, with a reminder sent on February 15. Responses received between January 15 and February 29 were included. All survey questions were mandatory. The questionnaire aimed to explore attitudes, practices, and perceived barriers towards NPM of RA.
Questionnaire
The survey questionnaire, detailed in Appendix 1 (available in online version), was developed following a comprehensive review of existing literature on the basis of the American College of Rheumatology’s guidelines for non-pharmacological interventions in RA [9] and related narrative reviews and surveys, by a group of four expert rheumatologists (PhD and professor level) working in the university hospital sector.
To ensure the questionnaire’s quality, it underwent two rounds of reviews to verify that the questions were clear, relevant, and aligned with the study objectives.
To assess completeness, we ensured that the questionnaire comprehensively covered all relevant aspects of NPM in RA, based on the guidelines and literature reviewed.
To evaluate feasibility, the questionnaire was subjected to simulated completion and pilot testing with ten rheumatologists, after which a further revision was made to enhance the questionnaire’s clarity and applicability. The average completion time during pilot testing was 5 minutes.
The final version of the questionnaire consisted of four sections:
the first section collected sociodemographic information, including four items on participants’ demographic data: sex, age, workplace, and duration of experience;
the second section, composed of four questions, assessed participants’ attitudes about:
– the level of awareness among rheumatologists and patients regarding the importance of integrating various components of NPM of RA,
– the level of patient adherence to NPM of their RA,
– rheumatologists’ attitudes regarding the necessity of developing tailored NPM recommendations for RA adapted to the Moroccan context;
the third section, which included 12 questions, assessed participants’ practices, focusing on the level of integration of non-pharmacological treatment for RA in routine practice. It included questions about personalization of non-pharmacological interventions based on patients’ needs and capabilities, the stage of disease management at which personalized NPM was proposed, and the involvement of patients by rheumatologists in the decision-making process regarding NPM;
in the fourth section, composed of 9 questions, rheumatologists were asked about perceived barriers to integrating non-pharmacological interventions into the management of patients with RA. These barriers included: lack of knowledge about non-pharmacological treatment for RA, lack of suitable training, time management difficulties during consultations, neglect by rheumatologists, challenges in organizing multidisciplinary care, lack of multidisciplinary team members, difficulties in communicating with patients due to their educational level, economic constraints, and lack of specialized infrastructure.
Rheumatologists’ attitudes and perceived barriers were evaluated using Likert scale items with 5 levels: 1 – strongly disagree, 2 – disagree, 3 – neutral, 4 – agree, or 5 – strongly agree.
Rheumatologist’s’ practices were evaluated with Likert scale items of 5 levels as: 1 – never, 2 – rarely, 3 – sometimes, 4 – frequently and 5 – always.
Management and statistical analysis
The data were entered and analyzed, and a descriptive analysis of the validated data was then carried out.
Qualitative variables were expressed as numbers and percentages, and quantitative variables were expressed as means and standard deviations, and medians with interquartile ranges, as appropriate. We performed univariate analysis using parametric and/or non-parametric statistical tests, as appropriate.
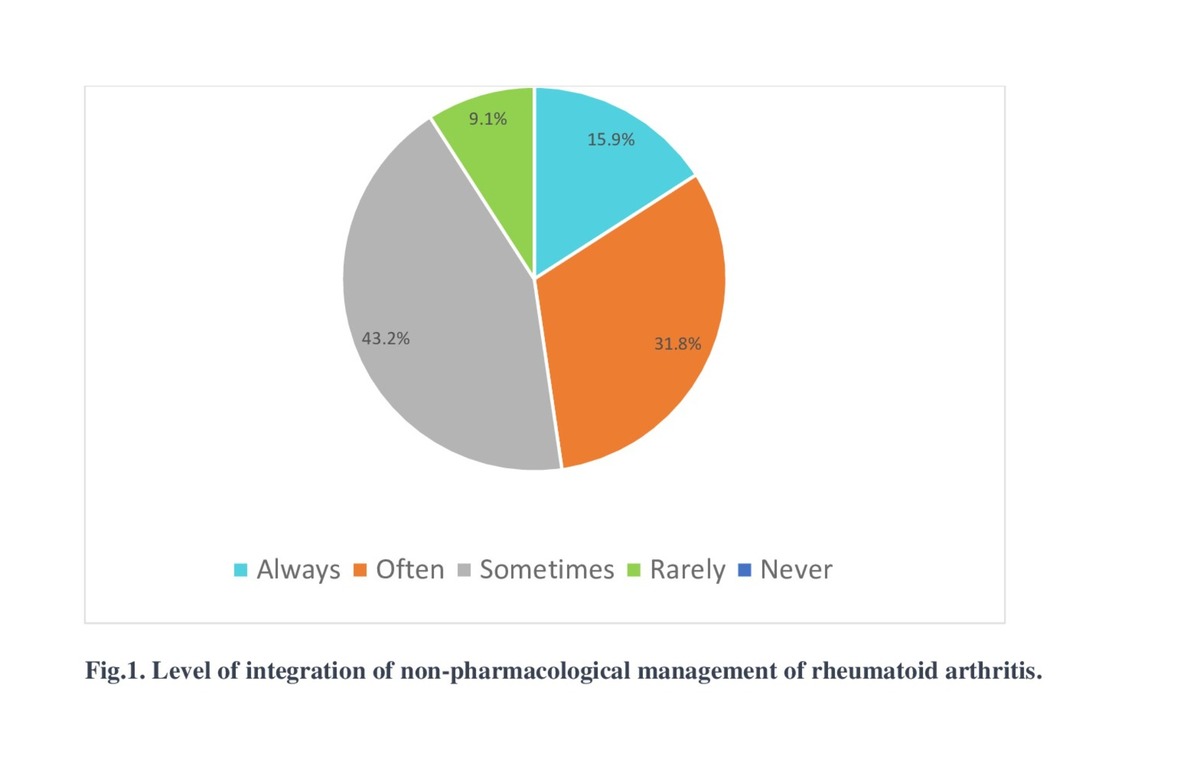
The level of integration of NPM of RA was changed to a binary variable: lack of integration of NPM included responses with never, rarely and sometimes, whereas a satisfactory level of integration included responses with often and always.
Responses to perceived barriers were also changed to a binary variable: “perceived barrier” of non-pharmacological treatment included responses with strongly agree and agree, whereas “absence of barrier” of integration included those with responses including disagree, strongly disagree and neutral.
Univariate analysis was performed using the χ2 test, Fisher’s exact test and Mann-Whitney test depending on the test conditions.
A difference was considered statistically significant if the p < 0.05. Associations were expressed as odds ratios (OR) with a 95% confidence interval. Data analysis was performed using Jamovi 2.3.19 statistical software.
Bioethical standards
The survey received approval from the ethics committee of the University Mohammed V, Rabat, Morocco (Faculty of Medicine and Pharmacy) (ethical approval no. 48/24) and was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable standards. Each rheumatologist received an Information Letter and Consent Form, detailing the purpose and process of the study along with a clickable link to the survey. Completing the self-administered questionnaire implied consent to use the responses, and all data were analyzed anonymously.
Results
Demographic and clinical characteristics
Out of 440 questionnaires sent, 132 rheumatologists completed and returned the questionnaire, yielding a response rate of 30%. The mean age of rheumatologists was 44 ±12 years. The majority were women (84.8%) with an average professional experience of 13 years [6; 22]. Forty-two point four percent were in the private sector, while 28%, 20.5%, and 9.1% were rheumatologists in the public sector, residents in rheumatology and rheumatologists in the university hospital sector, respectively. The demographics of the rheumatologists are presented in Table I.
Table I
Socio-demographic characteristics of participants (January–February 2024; n = 132)
| Factor | All patients | Level of integration of non-pharmacological management | |
|---|---|---|---|
| Good integration | Lack of integration | ||
| Average age [years]* | 44.4 ±12.8 | 45.6 ±13.1 | 43.4 ±12.5 |
| Sex** | |||
| Female | 112 (84.8) | 54 (48.2) | 58 (51.8) |
| Male | 20 (15.2) | 9 (45.0) | 11 (55.0) |
| Place of practice** | |||
| Resident in rheumatology in the university hospital sector | 37 (28.0) | 10 (37.0) | 17 (63.0) |
| Rheumatologist in the public sector | 56 (42.4) | 16 (43.2) | 21 (56.8) |
| Rheumatologist in the private sector | 27 (20.5) | 29 (51.8) | 27 (48.2) |
| Rheumatologist in the university hospital sector | 12 (9.1) | 8 (66.7) | 4 (33.3) |
| Experience** | |||
| ≤ 5 years | 29 (22.0) | 11 (37.9) | 18 (62.1) |
| > 5 years, ≤ 10 years | 17 (12.9) | 7 (41.2) | 10 (58.8) |
| > 10 years, ≤ 20 years | 42 (31.8) | 20 (47.6) | 19 (43.2) |
| > 20 years | 44 (33.3) | 25 (56.8) | 19 (43.2) |
Rheumatologists’ attitudes to implementing non-pharmacological management of rheumatoid arthritis
All rheumatologists strongly agree or agree on the importance of integrating NPM of RA into their daily practice. However, 40.1% believe (agree or strongly agree) that patients with RA are not aware of the importance of integrating NPM and that patients do not adhere sufficiently to the NPM of their disease (82.6%). Additionally, 98.5% of rheumatologists agree or strongly agree about the necessity to develop NPM recommendations tailored for the Moroccan context.
Rheumatologists practices in implementing non-pharmacological management of rheumatoid arthritis
In their routine practice 52.3% of rheumatologists lack integration of non-pharmacological interventions into the management of patients with RA (responding: never (0%), rarely (9.1%), sometimes (43.2%), as shown in Figure 1.
Only 27.3% always propose adapted and personalized NPM from the diagnosis of RA for their patients.
Rheumatologists always tailor non-pharmacological interventions based on the patient’s needs in 44.7% of cases and based on the patient’s capabilities in 40.2% of cases. Approximately 1 in 3 rheumatologists (35.6%) always involves patients in the decision-making process regarding non-pharmacological interventions.
The frequency of implementation of different types of non-pharmacological interventions for RA by rheumatologists is presented in Table II.
Table II
Frequency of implementing different types of non-pharmacological interventions for RA management
We measured on a 5-point scale (always/frequently/occasionally/rarely/never) and counted the number of “always” and “frequently”.
The non-pharmacological treatments mainly used were found to be patient education on smoking cessation (n = 117 [88.6%]), adapted physical activity (n = 98 [74.2%]), evidence-based dietary advice (n = 95 [72%]), and patient education on the importance of managing stress (n = 92 [69.7%]).
Rheumatologists’ perceived barriers towards implementing non-pharmacological management of rheumatoid arthritis
Perceptions of rheumatologists regarding barriers to NPM of RA are presented in Table III.
Table III
Rheumatologist’s responses on perceived barriers to the integration of NPM of RA
The lack of integration of NPM for RA into the practices of Moroccan rheumatologists was not found to be significantly associated with age, sex, experience, or place of practice, as presented in Table IV.
Table IV
Associations between the different variables and lack of integration of NPM of RA
In univariate analysis (Table V) the lack of integration of NPM for RA into routine practice of Moroccan rheumatologists was found to be significantly associated with insufficient training (p = 0.03) and lack of knowledge about the various components of NPM of RA (p = 0.008).
Table V
Barriers affecting the integration of NPM of RA
Rheumatologists who expressed lack of knowledge about the NPM of RA were 0.34 times (OR 0.34; 95% CI: 0.15–0.76) less likely to have a good level of integration of NPM than those who did not express this barrier. The integration of NPM of RA in routine practice was significantly lower in rheumatologists who expressed the lack of suitable training for non-pharmacological treatment (OR 0.09; 95% CI: 0.01–0.86).
Discussion
Our study sheds light on the substantial prevalence of non-implementation of non-pharmacological treatments in the management of RA by Moroccan rheumatologists. It explores attitudes and practices regarding these treatments, and identifies the main factors reported by rheumatologists as barriers preventing consistent use of non-pharmacological treatments in the management of RA in their routine practice.
Rheumatoid arthritis is the leading cause of chronic inflammatory rheumatic diseases. It affects approximately 1% of the global population. It is a debilitating condition that leads more or less rapidly to cartilage and bone destruction and, in the long term, in the absence of treatment, to severe functional impairment and/or disability [10].
While the treat-to-target approach has transformed outcomes for patients with RA, emerging evidence suggests that achieving remission alone may not fully restore patients’ quality of life or mitigate the extra-articular effects of RA. Therefore, patients are likely to benefit from management strategies that go beyond addressing synovitis and include more holistic assessments of the broader impacts of RA and their management [11].
Consequently, there is a compelling need for an integrated approach that aims to achieve both biological remission and remission of the impact on patients’ lives [12]. This will require both pharmacological and non-pharmacological interventions ideally in the context of a multidisciplinary team. Its evidence base was established through a recent umbrella review, which assessed the effectiveness of such interventions across the seven key domains of RA impact: pain, functional disability, fatigue, emotional well-being, sleep, coping, and physical well-being [13].
Non-pharmacological treatments demonstrate a complementary effect in RA management, particularly in difficult-to-treat RA (D2TRA), where non-pharmacological interventions can enhance the efficacy of pharmacological therapies. The EULAR guidelines for managing D2TRA emphasize the importance of incorporating non-pharmacological interventions, which are increasingly recognized for their role in improving outcomes in this condition [14].
Attitudes
All rheumatologists participating in the survey were aware of the importance of NPM of RA, which aligns with the findings of a survey on the clinical practice of RA management by Korean medical doctors [15].
According to our responders, patients are not fully aware of the importance of integrating non-pharmacological care in managing their disease, and their adherence to non-pharmacological care was considered insufficient.
Our findings align with another study [16] that evaluated PR patients’ adherence to physical activity, a crucial aspect of non-pharmacological care. Individuals with RA tend to exhibit more sedentary behavior and engage in less physical activity compared to healthy individuals.
Therefore, health professionals should prioritize raising awareness among patients about the significance of non-pharmacological treatment. It is imperative that patient education be customized to individual patient needs, as it serves as a cornerstone in patient adherence to treatment goals and protocols, as well as to non-pharmacological interventions.
Moreover, the gaps observed in non-pharmacological treatment for RA management may also stem from the absence of recommendations regarding the NPM of RA in Morocco. In light of this, all rheumatologists unanimously agreed on the necessity of developing tailored recommendations to our local context.
Practices
Despite their awareness about the positive effect and the importance of NPM of RA, the lack of implementation remains prevalent in our context (52.3% of responders).
A minority of respondents (less than one-third) advocated for NPM from the onset of RA diagnosis, reflecting potential gaps in clinical practice compared to recommended guidelines. The 2016 EULAR recommendations [17] underscore the importance of incorporating non-pharmacological interventions alongside drug treatments in early arthritis management, emphasizing the significance of shared decision-making between patients and rheumatologists.
Our study revealed that only 35.6% of rheumatologists systematically involved patients in non-pharmacological disease management, with less than half tailoring interventions to individual patient needs. This underscores the need to prioritize shared decision-making in clinical practice, enabling patients and providers to collaboratively navigate treatment decisions based on both scientific evidence and patient preferences [18].
Non-pharmacological therapies encompass a diverse range of interventions, spanning from dietary adjustments and lifestyle modifications to educational initiatives. Our study aimed to assess the most commonly utilized components of non-pharmacological care by rheumatologists in the management of RA. Among these, smoking cessation counseling emerged as a prominent intervention, with the majority of rheumatologists routinely providing advice to their patients on smoking cessation. This finding contrasts with the results of another observational study where smoking cessation counseling was documented in only 10% of visits, particularly when RA was well controlled [19].
Additionally, our study revealed that over 60% of rheumatologists frequently advocate for adapted physical activity, aligning with the 2018 EULAR recommendations [19] that emphasize the integration of physical activity into standard RA care. Health professionals play a pivotal role in promoting regular physical activity and fostering collaborative relationships across different disciplines to support effective disease management.
Furthermore, our findings indicate that certain non-pharmacological interventions are less commonly utilized by rheumatologists. Patient education on the importance of restful sleep was noted to be underutilized despite evidence linking pain and suboptimal sleep in RA patients. In addition, several studies found that higher disease activity is associated with sleep problems; thus, integrating sleep assessments and treatments into routine clinical assessments could alleviate pain and improve sleep quality in RA patients [21–23].
Promoting patient education on good oral hygiene, ergonomic advice and conducting psychological assessments were also underutilized by our responders. These also represent essential aspects of RA NPM, given their significant impact on disease outcomes. These interventions should be prioritized to enhance the overall well-being and quality of life for individuals living with RA [4, 5, 13].
Regarding the demographics, our study revealed no statistically significant relationships between the level of implementing the NPM and age, sex, years of experience, or working area. Our findings are consistent with another study assessing the use of non-pharmacological methods among nurses [24].
Restrictions on access and application of non-pharmacological management
Barriers related to NPM access were identified, including factors related to economic difficulties, lack of specialized infrastructure, lack of multidisciplinary team members and challenges in organizing multidisciplinary care. The most prominent access barrier highlighted by providers was the difficulty in organizing multidisciplinary care.
Regarding barriers related to NPM knowledge, rheumatologists noted a lack of understanding about NPM of RA and insufficient training in this area. These two barriers were significantly associated with the lack of implementation of NPM for patients with RA.
Barriers related to patient-rheumatologist interactions included difficulties in communicating with patients, particularly those with lower levels of education.
Additionally, rheumatologists reported challenges with time management during consultations and neglect issues.
All these barriers underscore the importance of improving patient-rheumatologist interactions by raising patient awareness of NPM of RA through motivational enhancement and educational messages. Additionally, there is a need for comprehensive training on various aspects of NPM of RA and the provision of adapted tools for effective communication with RA patients about the significance of NPM. Multidisciplinary collaborative work is essential to ensure optimal patient care. Expert recommendations tailored to our context are also needed to support the implementation of NPM of RA management.
Addressing socioeconomic factors and encouraging healthcare professionals to recommend non-pharmacological treatments while considering patients’ needs, capabilities, and preferences are crucial steps that can positively impact patient outcomes. Finally, significant efforts to overcome barriers such as lack of time and workload are imperative to increase the clinical utilization of non-pharmacological methods by RA patients.
Limitations
Our study has several limitations that should be noted. Despite our efforts to obtain a representative sample, the sample size of 132 rheumatologists may not fully capture the diversity of practices and perspectives within the country. Moreover, reliance on self-reported data introduces the potential for bias or inaccuracies, especially regarding practices and attitudes. Additionally, the cross-sectional design of our study restricts our ability to establish causality or monitor changes in attitudes and practices over time.
Furthermore, the lack of open-ended responses is another limitation. Such responses would have provided more personalized insights into the practice routines reported by rheumatologists.
However, despite these limitations, our study has provided relevant insights into the extent of implementation of non-pharmacological treatments for patients with RA among Moroccan rheumatologists. Additionally, it has shed light on the factors limiting the integration of adapted non-pharmacological interventions in our context.
Conclusions
Our study highlights significant gaps in the integration of NPM of RA among Moroccan rheumatologists. Despite strong recognition of its importance, practical implementation remains inconsistent. Key barriers identified include insufficient training, lack of knowledge, and infrastructural limitations. Additionally, challenges in patient-rheumatologist communication and time constraints were noted. Addressing these issues through tailored educational programs, enhancing multidisciplinary collaboration, and developing context-specific guidelines is essential. Future efforts should focus on overcoming these barriers to improve the holistic management of RA, enhancing patient outcomes and quality of life.