Introduction
Non-traumatic spinal cord injury (NTSCI) results from various pathological processes originating within or adjacent to the spinal canal, leading to spinal cord compression [1]. Non-traumatic spinal cord injury constitutes a diagnostic and therapeutic emergency, necessitating early intervention due to its implications for both vital and functional prognosis [1]. In developed countries, the etiologies of NTSCI are predominantly degenerative and neoplastic causes [2]. In developing countries, Mycobacterium tuberculosis and human immunodeficiency virus (HIV) infections are reported to be the main cause of NTSCI, although tumors are also implicated [2]. In sub-Saharan Africa, NTSCI presents a high morbidity rate with 50% disability and an estimated 10% mortality at admission, leading to significant economic consequences for patients [3]. This syndrome, despite its neurological nature, is also encountered in rheumatology, as rheumatologists manage musculoskeletal disorders, and spinal involvement above L2 poses a risk for NTSCI. However, limited data exist on the different profiles and specific characteristics of this syndrome within rheumatology [2], prompting our study aimed at describing the etiological aspects and associated factors of NTSCI in the Rheumatology Department of the University Hospital Center of Bogodogo (CHU-B) in Ouagadougou, Burkina Faso.
Material and methods
This was a cross-sectional, retrospective study with descriptive and analytical aims, conducted from January 1, 2017, to December 31, 2023, in the Rheumatology Department of CHU-B. Patients included were those hospitalized in the Rheumatology Department during the same period with at least 75% completeness of clinical records. These were patients who were hospitalized and diagnosed with NTSCI based on clinical presentation of spinal, lesional, and sublesional syndromes, or based on imaging findings, with an established etiological diagnosis. Patients not meeting the inclusion criteria were excluded. Data were collected using a specifically designed form. Source documents included hospitalization registers, medical records, and reports of medical imaging and laboratory results.
The variables of interest were:
sociodemographic data: age, sex, occupation, and residence;
clinical data: reason for consultation, duration of symptom evolution, pain characteristics, spinal syndrome, radicular syndrome, and sphincter disturbances;
etiological data;
paraclinical data: type of radiological examination, radiological lesions, location and origin of the compression;
therapeutic data: glucocorticosteroid therapy, bisphosphonate, chemotherapy, anti-tuberculosis treatment, antibiotic, analgesic, radiotherapy, and surgical treatment;
evolutionary data: discharge against medical advice (DAMA), recovery, death, complete deficit recovery, incomplete deficit recovery, transfer to other services, and complications of immobility.
Data were entered into an Excel database and all analyses were performed using SPSS software version 20.0. Missing data were treated as such during analyses. The hospital frequency of NTSCI was calculated from the total number of patients hospitalized in the department during the study period. Continuous variables were summarized using measures of central tendency (mean and median) and dispersion (range, standard deviation). The association between the dependent variable (motor deficit recovery) and each independent variable was studied using the χ2 test or Fisher’s exact test followed by the p-value. A significance threshold of 5% was used.
Bioethical standards
Anonymity and data confidentiality were maintained in accordance with the recommendations of the Declaration of Helsinki. Bogodogo University Hospital provided ethical approval for the study (No. of approval: 2024-02-32). Identifiers were assigned to each patient during data collection, ensuring that no names appeared in our database, thus preserving anonymity and confidentiality.
Results
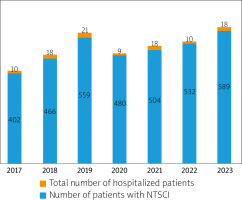
A total of 3,532 patients were admitted to the conventional hospitalization unit of the Rheumatology Department at the CHU-B from March 1, 2017, to December 31, 2023. Among these, 104 patients had NTSCI, yielding a frequency of 2.94%. Figure 1 shows the distribution of NTSCI cases by year. The mean age of the patients was 57.91 ±13.56 years, ranging from 27 to 85 years. Males represented 65.38% (n = 68) of the cohort, resulting in a sex ratio of 1.88. Table I displays the socio-demographic, clinical, and paraclinical characteristics of our study population.
Table I
General characteristics of our study population
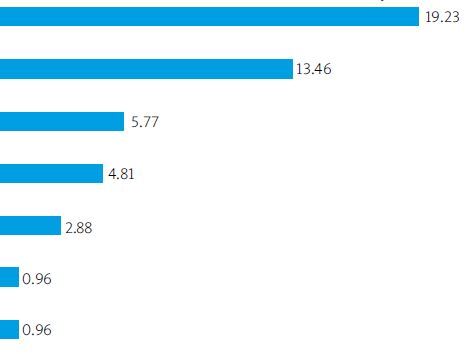
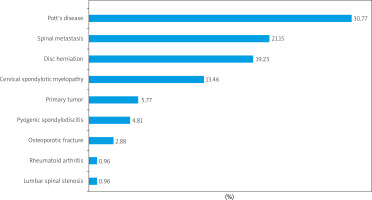
Tuberculosis was diagnosed in 32 cases (30.77%) (Fig. 2), followed by spinal metastases in 22 cases (21.15%). The main etiologies are illustrated in Figure 3.
Fig. 2
Pott’s disease of T7–T8 spondylodiscitis complicated by spinal cord compression with intraductal abscess.

Fig. 3
Distribution of different etiologies of NTSCI in the Rheumatology Department of Bogodogo University Hospital.
Regarding therapeutic and evolutionary aspects, systemic corticosteroids were prescribed for 74 patients (71.15%), and second-tier analgesics were used in 40.38% of cases (n = 42). Twenty-nine patients (27.89%) experienced complications related to immobility. Table II outlines the different evolutionary modalities of our patients.
Table II
Progression of patients treated for NTSCI
| Evolution | Frequency(n = 104) | Percentage (%) |
|---|---|---|
| Incomplete recovery | 57 | 54.80 |
| Full recovery | 47 | 45.19 |
| Transfer to another department | 28 | 26.92 |
| Deaths in service | 11 | 10.57 |
| DAMA | 5 | 04.80 |
In bivariate analysis, no factor was significantly associated with deficit recovery (Table III).
Table III
Results of bivariate analysis of factors associated with recovery of motor deficit
Discussion
According to our knowledge, this study is the first to focus on the epidemiology and analysis of factors associated with NTSCI in a rheumatology department in Burkina Faso. The NTSCIs are relatively less frequent in our context compared to those commonly described in Western literature, where the incidence ranges from 20 to 68 cases per million inhabitants per year [4]. However, the data found in our series are similar to those from other studies conducted in African populations, with hospital frequencies between 0.6% and 3% [5, 6]. The lower frequency of NTSCI in our study compared to high-incidence Western studies can be attributed to several factors. First, it is possible that the diagnosis of spinal compressions is less frequent due to the multidisciplinary nature of spinal compression management, where most patients are admitted to various medical and surgical specialties. Consequently, our study, conducted solely within a rheumatology department, contrasts with other studies mainly conducted in neurology and neurosurgery units [4].
In our study, a higher number of men (65.38%) than women were affected by NTSCI, a trend also observed in other African studies [5, 6]. In contrast, Smith et al. [3] found a female predominance (51.2%) in the European population. The mean age of the patients in our study was 57.91 years, similar to that reported by Ndao et al. (58 years), and to that of Western studies (56.6 years) [3, 6, 7]. These results suggest that NTSCIs primarily affect individuals in their fifties, and the older age of our patients and the male predominance are likely correlated with the observed etiologies, notably Pott’s disease and neoplastic causes.
Back pain was present in all our patients, unlike the series by Kassegne et al. [8] (55%) and Ouboukhlik et al. [9] (67%). This difference can be explained by the fact that our study was conducted in a rheumatology department where back pain is the main reason for consultation, whereas other studies were conducted in neurology and neurosurgery departments where neurological signs were more prominent. Furthermore, the average duration of motor deficit onset of 3 months in our study, compared to one month in the Irish population, indicates a delay in seeking medical care in our populations within the African context, partly due to the absence of health insurance [3].
Magnetic resonance imaging (MRI) was the most frequently performed second-line examination in our series, consistent with observations in the existing literature, with a rate of 55.77% [2, 6, 7]. This predominance is due to MRI’s status as the reference examination for diagnosing spinal cord compression syndrome, displaying remarkable sensitivity (93%) and specificity (97%) [10]. However, the widespread adoption of MRI is hindered by its high cost, which is a limiting factor in our daily practice.
A notable characteristic of our continent is the predominance of tuberculosis etiology in cases of spinal cord compression. This observation, corroborated by several African studies, including ours, highlights Pott’s disease as the most frequent pathology, regardless of the type of receiving department [6–11]. In contrast, data from Asia and Europe reveal a higher prevalence of degenerative etiology of NTSCI, at 59% and 32% respectively [4]. In North America, tumor etiologies and lumbar canal stenosis dominate, representing 26% and 56% of cases, respectively [4]. This etiological disparity can be explained by several factors. Firstly, the prevalence of tuberculosis in the Caucasian populations of developed countries is relatively low, contrasting with African realities [4]. Secondly, the aging population in the West largely contributes to the predominance of degenerative pathologies and malignant tumors, which are known to be more frequent in older subjects [4].
Regarding short-term evolutionary modalities, complete recovery of neurological deficits was observed in 16.34% of our patients. These results, lower than those of Kassagne et al. (41%), can be explained by delayed consultation and limited access to neurosurgical interventions due to insufficient financial resources [8]. In terms of mortality, 10.7% of our patients died during hospitalization, a rate significantly higher than that observed in the Israeli population over a one-year follow-up (0.6%) [12]. It is also significantly higher than that observed in the American (0.2%) and Australian (1.2%) populations [13, 14]. This low mortality can be attributed to early functional rehabilitation and a low representation of malignant and infectious etiologies in their sample.
This study has some limitations. Firstly, as in all retrospective studies, some cases may have been missed, a bias also recognized in other high-quality studies [3–6]. Secondly, we were unable to collect data on the Frankel score, subsequent management, and the evolutionary modalities of patients referred to other departments. Finally, due to the limited number of our patients, our analytical results were not statistically significant.
Conclusions
Non-traumatic spinal cord injury in rheumatology remains an emergency. In our study, the main causes identified were Pott’s disease and spinal metastases. Magnetic resonance imaging continues to be the reference examination for confirming the diagnosis and guiding etiological investigation. We did not find any factors associated with the recovery of the motor deficit. Further research is necessary to evaluate deficit recovery and long-term mortality. Geoepidemiological risk factors and geographical distribution should be taken into account in NTSCI analysis. The establishment of an NTSCI global registry and international cooperation in analysis of this clinical problem are necessary to better assess the causes, and to improve diagnostics and treatment schemes in NTSCI.