Introduction
Juvenile idiopathic arthritis (JIA) is a heterogeneous group comprising idiopathic inflammatory arthritis affecting children younger than 16 years of age and lasting six weeks or longer [1]. In western populations, studies have reported an incidence and a prevalence of JIA varying from 2 to 150 per 100,000 [2].
The etiopathogenesis of idiopathic arthritis (IA) is unknown, and the diagnosis is established on the basis of the clinical picture and exclusion, which means that other causes of arthritis need to be ruled out before final diagnosis. Molecular studies indicate many associations between subtypes of JIA and human leukocyte antigen (HLA) genes [3].
Seven subtypes of juvenile idiopathic arthritis have been distinguished by the International League of Associations for Rheumatology (ILAR): systemic JIA, oligoarthritis, polyarthritis positive rheumatoid factor (RF), polyarthritis negative RF, psoriatic arthritis, enthesitis-related arthritis (ERA), and undifferentiated arthritis.
The last subtype does not fit the criteria of any of the other categories, also overlapping syndromes are included into this last subtype. Oligoarthritis subtype is the most common and concerns approximately 27–60% of children with juvenile idiopathic arthritis [1, 3].
In general, regardless of subtype, JIA is characterized by prolonged synovial inflammation that can cause cartilage and bone damage, and it leads to impairment of physical function and has a significant impact on quality of life [4].
Damaged cartilage facilitates binding of synovial inflammatory cells leading to increased risk of even more cartilage degeneration in the future [5]. Thus, early diagnosis is essential for the prevention of development of potentially irreversible pathological lesions.
Magnetic resonance imaging (MRI) is one of the most advanced imaging techniques available in modern medicine. A wide range of diseases can be diagnosed and monitored in MRI. Rheumatoid disorders primarily affecting the musculoskeletal system are frequent referral causes to radiology departments in order to perform MRI examination.
Thanks to a lack of ionizing radiation, high spatial and contrast resolution, as well as multiplanar imaging, MRI is a valuable tool in diagnosis of arthritis [6]. It is more sensitive than physical examination, and optimized MRI protocols allow pediatric patients as young as 4 years old to undergo examination without sedation or general anesthesia [6].
The knee is the most commonly affected joint in children with JIA [7], and MRI of this anatomical region is the most frequently performed cross-sectional musculoskeletal imaging examination in the pediatric group of patients [8].
Thus, in this article we review the latest literature concerning MRI of the knee joint in JIA and present the most common MRI findings that every pediatric rheumatologist should be familiar with.
Magnetic resonance imaging – general information
Magnetic resonance imaging of the knee joints in JIA patients is usually the third imaging examination, after radiography and ultrasonography. Radiography is the standard examination in the assessment of JIA, especially in the differential diagnosis and treatment monitoring of disease.
It is also possible to recognize growth deviations (acceleration or retardation) and easily compare collateral joints, which in some cases may be crucial (for example, to identify early epiphyseal hyperplasia/ballooning due to hyperemia), not mentioning advanced destructive lesion in the knee joint in the course of juvenile idiopathic arthritis [9].
However, this modality is not able to visualize early signs of inflammatory changes in soft tissues, such as synovitis, enthesitis, and tenosynovitis, or bursitis or inflammatory involvement of the bone marrow. Such early findings can be diagnosed with MRI or ultrasonography (US).
Ultrasound is commonly performed for knee joint assessment and provides information on soft tissue involvement (effusions, synovitis, tenosynovitis, bursitis), but it has limited access to all joint surfaces, which means that the hyaline cartilage is only partially visible.
It has also limited ability to evaluate bone tissue, due to lack of penetration of ultrasound through that tissue; therefore, not all subchondral or subcortical cysts and erosions are seen.
The advantage of magnetic resonance imaging over US and radiographs is the ability to precisely assess all tissues involved by JIA, both the soft tissues and bone, including bone marrow edema, which is only visible in MRI and may be an additional feature of early JIA and a predictor of erosive joint damage [9, 10].
The added value of ultrasonography is a dynamic examination during joint motion, which provides valuable information (e.g. on the patellofemoral joint), whereas Doppler modalities allow assessment and follow-up of synovium and tenosynovium vascularity [2].
In the detection of early inflammatory lesions in JIA several studies have confirmed that MRI is superior to ultrasonography [11].
Also, in the case of early identification of erosions, Malattia et al. [12] confirmed the superiority of MRI; however, ultrasound was at least as good if not better than plain radiography for the detection of cortical erosions.
Fortunately, due to the availability of efficient treatment protocols in developed western countries, erosive changes in knee joints are rare among patients with JIA nowadays and are seen only in very advanced cases as a late complication [13].
Novel biological drugs have been developed, shifting the focus of pediatric rheumatologists from erosive lesions toward inflammatory changes in the early stages, which cannot be detected in radiography [14].
This has resulted in increased necessity of US and MRI diagnostics of those subtle changes. Prompt diagnosis and treatment are essential to prevent permanent joint damage and preserve joint functionality [2].
Magnetic resonance imaging findings in knee joints in the course of juvenile idiopathic arthritis
The main indications to knee joint MRI in JIA patients comprise assessment of inflammatory lesions in joints, tendon sheaths, bursae, entheses, inflammatory changes in bone marrow, and their complications (mainly cysts, erosions, cartilage damage).
Synovial thickening, synovial inflammation (synovitis), joint effusions, and bone marrow edema are the most prevalent disease features, followed by destructive, chronic lesions, such as cartilage loss, bone erosions, tendinopathy, and enthesopathy, which occur significantly less frequently [13]. The process is shown in Figures 1–3.
Fig. 1
T2-weighted short-tau inversion recovery magnetic resonance imaging is fluid sensitive sequence. Arrow indicates joint fluid in the axial plane.
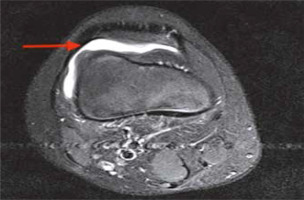
Fig. 2
A 10-year-old boy with advanced juvenile idiopathic arthritis. Non-contrast sagittal proton density fat saturated magnetic resonance imaging shows bone marrow edema (red arrows) and joint effusion (green arrow).

Fig. 3
Non-contrast sagittal proton density knee magnetic resonance imaging of a 12-year-old girl with long history of juvenile idiopathic arthritis presents bone erosion on the articular surface.

Other findings described by researchers include developmental lesions, such as cruciate ligament thinning as well as menisci hypoplasia due to synovial hypertrophy extending over the meniscal surfaces, which result in meniscal hypoplasia and degradation [15].
Of note, joint complications can result from treatment as well (bone loss and fractures, or avascular necrosis), and MRI is the method of choice in diagnosing the early stages of such pathologies [9].
Table I presents basic lesions that can occur in arthritis, described by the ESSR (the European Society of Musculoskeletal Radiology) arthritis subcommittee along with their particular MRI definitions [16].
Table I
Magnetic resonance imaging features of lesions observed in juvenile idiopathic arthritis [16]
The most commonly seen pathology in the knee joint is synovitis. A vicious circle of inflammatory cells and cytokines interacting with synovium triggers synovial hypertrophy and joint effusion, which are revealed at the early stage.
Subsequently synovitis occurs and progressively leads to cartilage loss and bone erosions. Synovial hypertrophy in MRI according to the Juvenile Idiopathic Arthritis MRI Scoring (JAMRIS) is defined as an enhancing thickened synovial membrane.
Thus, the scoring requires intravenous (i.v.) contrast injection and describes synovitis as enhancing synovial tissue > 2 mm in thickness [17].
In the subsequent magnetic resonance imaging study of Hemke et al. [18] the maximum measured synovial thickness in knee joints among 57 healthy children was 1.8 mm, which confirmed the good reliability of the 2 mm cut-off value in the JAMRIS system.
Magnetic resonance imaging protocols and scoring
According to recommendations of the ESSR arthritis subcommittee, the knee joint protocol should include the following MRI sequences: sagittal proton density (PD) fat suppressed (FS), coronal PD FS, axial PD FS, sagittal or coronal T1-weighted, and T1 or T1 FS after contrast administration [16].
Of course, as the authors underline in the recommendation paper, each MRI protocol should be adjusted to the individual machine scanner specifications, available coils, and image quality in particular sequences.
Hemke et al. [13] proposed the following knee protocol: sagittal and coronal T2-weighted FS or short-tau inversion recovery (STIR), coronal T1-weighted, sagittal gradient echo, or PD and T1-weighted FS post gadolinium sequence. This protocol is able to identify joint effusion, synovial thickening, bone marrow edema and inflammation (osteitis), bone erosions, and cartilage loss [13].
Intravenous contrast injection remains a significant problem, especially in the pediatric population. On the one hand, the accurate assessment of synovitis requires contrast injection because non-contrast MRI reduces sensitivity for detection of inflamed synovium to 62% [19].
On the other hand, MRI contrast material administration is associated with increased risk of serious adverse events such as allergic reaction, nephrogenic sclerosis, as well as gadolinium brain deposition [20, 21].
For that reason, increased interest in alternative, safer non-contrast sequences has initiated a new direction in research. Diffusion-weighted imaging (DWI) is an MRI modality, which does not require contrast and is a promising biomarker in JIA [22].
A recently published study Barendregt et al. [21] confirmed the accuracy of DWI in detecting JIA inflammatory lesions in knee joints and suggested that this modality can even replace contrast-enhanced MRI for imaging of synovial inflammation in children affected by JIA.
Like as diffusion-weighted imaging, T1ρ MRI sequence does not require contrast administration. It provides cartilage assessment and proved to be acceptable in patients with JIA [23]. However, imaging in DWI sequence requires relevant experience, software, and in everyday radiological practice can be time consuming.
Scoring systems
In juvenile idiopathic arthritis, disease activity is assessed with scales using clinical examination as well as laboratory tests such as the erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) [24].
To the best of our knowledge, MRI is still not part of the outcome measures in disease activity, but its potential has been highlighted by the European League Against Rheumatism (EULAR) Paediatric Rheumatology European Society (PReS) imaging task force [25].
In regular clinical practice MRI reporting includes a qualitative approach, which is a description of abnormal findings, their location, number, and size. For treatment monitoring, especially in clinical trials, semiquantitative scorings are proposed.
There are two main magnetic resonance imaging scoring systems evaluating morphological changes, which can be implemented for the knee joint assessment in JIA [26].
First was developed by the International Prophylaxis Study Group (IPSG) and concerned MRI scoring for hemophilic arthropathy [27]. It has been proven to be useful for the evaluation of early and moderate stages of arthropathy and treatment monitoring [28].
Hemke et al. [17] developed the JAMRIS scale for use specifically in JIA, which has been thoroughly researched in recent studies. Compared to the International Prophylaxis Study Group, the JAMRIS system includes bone marrow evaluation but lacks bone cyst assessment and the presence of blood and hemosiderin in the joint (Table II).
Table II
Comparison of features assessed in Juvenile Idiopathic Arthritis MRI Scoring, the International Prophylaxis Study Group and the Combined Juvenile Idiopathic Arthritis Magnetic Resonance Imaging Scoring System
[i] JAMRIS – the Juvenile Idiopathic Arthritis MRI Scoring, JIA – juvenile idiopathic arthritis, IPSG – the International Prophylaxis Study Group, P – performed, NP – not performed, (+) – assessed in scale, (–) – not assessed in scale, a – definition incorporated from the Juvenile Idiopathic Arthritis MRI Scoring, b – definition incorporated from the International Prophylaxis Study Group.
Both scales provide definitions of pathologies [26, 27, 29] and score soft tissue as well as osteochondral parts of the joint. The reliability of Juvenile Idiopathic Arthritis MRI Scoring and JPSG in JIA has been evaluated by the outcome measure in juvenile idiopathic arthritis: outcome measures in rheumatology (OMERACT), with promising results proving their good reliability in knee joint assessment [26].
This study concluded by combining JAMRIS and JPSG into one scale. The combined juvenile arthritis MRI scoring system assesses five features: synovial thickening and bone marrow edema originating from JAMRIS and joint effusion, cartilage loss, and bone erosions originating from JPSG (Table III) [13].
Table III
Combined juvenile arthritis magnetic resonance imaging scoring system [13]
| Feature | Definition | Scoring |
|---|---|---|
| Synovial hypertrophy | An area of the synovial compartment that shows a thickened synovial membrane and which can show enhancement after intravenous gadolinium administration | Scored at six locationsa (0) normal, ≤ 2 mm (1) mild, > 2 mm to ≤ 4 mm (2) moderate/severe, > 4 mm Totals result in a minimum score of 0 and a maximum score of 12 |
| Joint effusion | An increased amount of fluid within the synovial compartment with high signal intensity on T2-w images and low signal intensity on T1-w images Joint effusion has no post-gadolinium enhancement | Scored at the largest pocket of joint effusion: (0) normal, ≤ 3 mm (1) mild, > 3 mm to ≤ 5 mm (2) moderate/severe, >5 mm large Totals result in a minimum score of 0 and a maximum score of 2 |
| Cartilage lesion | Loss of cartilaginous tissue either focally (superficial or deep) or diffusely | Scored at the most severely affected location: (0) none, (1) any loss, (2) > 50% volume loss, (3) full-thickness loss, (4) full-thickness loss > 50% of surface Total result in a minimum score of 0 and a maximum score of 4 |
| Bone marrow changes | An abnormality within the trabecular bone of the epiphysis, with ill-defined margins and high signal intensity on T2-w fat-saturated images and low signal intensity on T1-w | Scored semi-quantitatively based on the subjectively estimated percentage of involved bone volume at each site at eight locationsb, as follows: (0) none, (1) < 10% of the whole bone volume, (2) ≥ 10–25% of the whole bone volume, (3) > 25% of the whole bone volume Total result in a minimum score of 0 and a maximum score of 24 |
| Bone erosion | A sharply marginated bone lesion with correct juxta-articular localization, typical signal characteristics and visible in two planes with a cortical break in at least one plane; on T1-w images there is a loss of the normal low signal intensity of cortical bone and loss of the normal high signal intensity of trabecular bone | Scored at the most severely affected: location (0) none, (1) mild, any loss (2) moderate/severe, >50% surface involvement Total result in a minimum score of 0 and a maximum score of 2 |
Additional magnetic resonance imaging features that were listed by the authors [26] but were not included in their scoring are as follows: degree of synovial enhancement (scored 0–2), infrapatellar fat heterogeneity (0/1 binary assessment), and the presence of enthesopathy and tendinopathy of the patellar and quadriceps tendons (binary scoring 0/1).
Limitations of magnetic resonance imaging
Magnetic resonance imaging is not without disadvantages. The procedure is long and requires a motionless position. Very young, agitated patients with additional pain may require participation of anesthesiologists during the MRI scan.
High cost, limited accessibility, and lack of experience in MRI assessment of children affected by JIA are putative causes for underuse of MRI diagnosis in this group of patients. Moreover, the assessment involves one joint, with no possibility of comparing the contralateral side or performing a dynamic examination, which is possible in ultrasound [9, 30].
Although enhanced synovial thickening is a crucial MRI finding in JIA, some clinically active patients may show no synovial thickening on MRI of the knee joint [31].
This raises some doubts about the usefulness of MRI in determining whether the disease is active in all JIA patients or the disease activity is overrated in clinical examinations.
On the other hand, the authors did not analyze bone marrow edema in these patients as the possible sole site of disease, without synovitis, and new research is needed to verify which tissues are in fact mostly diseased in knee JIA.
Also, discriminating whether something is normal or pathological is a very challenging task among pediatric patients, and more research is needed in order to establish norms in MRI knee imaging, for example concerning the amount of fluid.
In healthy children usually the largest pockets of fluid are located around the cruciate ligaments and retropatellar region measuring approximately 3 mm in mean diameter [13].
Scoring systems proposed by IPSG and the combined juvenile arthritis MRI scoring system (shown above) scored abnormal joint effusion as thicker than 3 mm. Also, mild synovial thickening enhancing after contrast injection in the knee joint is not uncommon among children unaffected by clinical arthritis [32].
On the other hand, it is essential to keep in mind that JIA is a medical condition, which in some cases mimics or masks other musculoskeletal diseases [33]. For instance, traumatic injuries, impingements, patellofemoral joint malalignment are underestimated in children, which may cause delay of proper diagnosis.
In 2019 Yousef et al. [34] published a case report on avulsion of quadriceps tendon in an 8-year-old girl affected by JIA after a fall while playing. A distracting history of JIA had been deceiving doctors, which led to misdiagnosis. Consequently, delayed MRI was performed 10 days after trauma, revealing a serious traumatic lesion, which required urgent surgical intervention [34].
Different injury patterns of the knee joint in children than in adults, differences in ligamentous support, normal anatomic variants, and bone marrow appearance are factors that should be taken into consideration when evaluating the knee MRI in children [35].
Another challenging issue in pediatric rheumatology is the definition of remission, both in clinical and imaging studies. Quantitative measurements of synovial volume and the flow in the synovium through dynamic assessment of the uptake of gadolinium contrast can be useful in defining remission [36].
Discussion
The current criteria for the diagnosis of JIA, disease activity, and identification of remission are based mainly on clinical examination as well as laboratory tests [16]. Clinical assessment, even when performed by an experienced physician, has limited reliability.
Because the knee joint is the most frequently affected in JIA, MRI of this region should be considered as one of the priorities, which can help to diagnose disease at the early stage, tailor appropriate treatment, prevent irreversible progression, and decide when to cease drug administration. Magnetic resonance imaging is a superior and constantly developing musculoskeletal imaging technique.
The literature indicates that it is accurate, reliable, and feasible in detecting and monitoring JIA. Obviously, in clinical practice, the imaging approach usually starts from symmetric knee radiographs in two projections followed by ultrasound.
The former method provides limited data, especially in the early stage of JIA, regarding soft tissue swelling, joint space narrowing, and developmental disorders (mainly early epiphyseal hyperplasia).
Whereas the latter, ultrasound, enriches information with evaluation of synovial inflammation, but information regarding the bone, cartilage, and deeply located soft tissues is limited due to insufficient penetration of ultrasound waves. Nevertheless, it is worth emphasizing that the role of ultrasound in the diagnosis of JIA with knee involvement is indisputable.
Although less readily available, more time consuming, and more costly than ultrasound or radiography, MRI is far more objective, provides quantitative and semiquantitative evaluation of all tissues potentially affected by JIA (both soft and bone), and helps to differentiate from other conditions, such as trauma, overuse, or malignancies.
Quantitative studies are promising, providing more accurate assessment of inflammatory disease activity and treatment monitoring compared with semiquantitative systems [37].
Further research is required, especially regarding scoring systems, non-contrast sequences, and on potential incorporation of MRI into JIA classification criteria, disease activity monitoring, and remission diagnosis.
Conclusions
Magnetic resonance imaging is, and will undoubtedly continue to be, a method of precise assessment of joint changes in the course of JIA, with the possibility of quantitative assessment.
Good data archiving allows for a good comparative analysis of changes over time. The refinement of this method of imaging and measures of quantification of these changes may encourage the use of MRI while maintaining its cost-effectiveness.


