Introduction
Osteoarthritis (OA) is one of the most common chronic diseases, and it is strongly linked with aging [1]. Although it is not a direct threat to the patient’s life, it is one of the leading factors causing disability and depleting physical function in the older population. Furthermore, it affects overall health-related quality of life and social functioning, and causes psychological distress [2].
Total hip arthroplasty (THA) is the gold standard of treatment for the advanced stage of OA. It is acknowledged as a highly effective procedure in the reduction of pain and improvement of limb function, enabling the patient to return to everyday activities [3].
Due to the rising life expectancy and aging population, there is a continually increasing need for THA [4]. With older age, the burden of comorbidities increases, opposite to the functional reserve and resistance to external stressors such as surgical procedure. This state of depletion of reserves is referred to as “frailty syndrome” [5].
Patients with frailty syndrome subjected to surgical interventions have a higher incidence of complications associated with surgery and an increased mortality rate. They require prolonged hospitalization and achieve worse functional outcomes [6]. The identification of patients with frailty syndrome subjected to THA could lead to more accurate qualification for the procedure and provide high-risk patients with special perioperative care [7].
Nowadays, clinicians place particular emphasis on a holistic view of the patient, and there are useful tools available for the assessment of the clinical status of patients undergoing surgical procedures. Among them, the most common is the American Society of Anesthesiologists grades (ASA), Charlson Comorbidity Index (CCI), American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator (ACS NSQIP), and Elixhauser Comorbidity Method (ECM) [8]. Recently, based on ACS NSQIP data, the modified frailty index-11 (mFI-11) and modified frailty index-5 (mFI-5), were developed [9].
The authors demonstrated the high efficacy of this clinical tool in predicting mortality, postoperative complications, and prolonged hospitalization in patients subjected to THA [10]. In the study by Shin et al. [11], carried out on 14 583 patients undergoing THA, mFI-11 showed better predictive properties than ASA score in complications and 30-day mortality. However, the previous research conducted on mFI-5 and mFI-11 has not included the aspect of the long-term physical functioning of patients, pain severity, and satisfaction rate after the THA [7].
Objectives
Thestudyaimstoinvestigate the influence of frailty measured with mFI-5 and mFI-11 on the outcomes of primary THA in OA patients. The clinical outcomes were long-term functional results (WOMAC, HHS), pain complaints (VAS), complication rate, hospitalization time (LOS), and patient’s satisfaction (HKASS). Understanding the importance of frailty burden in the elderly population undergoing THA could have a substantial impact on the safety and effectiveness of this procedure.
Material and methods
Trial design
This is a single-center cohort observational study. The study received approval from the ethics committee of the Medical University of Warsaw as part of the project “Evaluation of the influence of coexisting diseases and other selected factors on the results of primary hip arthroplasty” (AKBE/196/2018).
The study followed (Strengthening the Reporting of Observational studies in Epidemiology – STROBE) guidelines for observational studies, and it was conducted according to the Guidelines of Good Clinical Practice and the principles expressed in the Declaration of Helsinki. All patients were recruited after providing written informed consent.
Setting and study population
The study was based on a retrospective analysis of clinical material from the Department of Orthopedics and Traumatology, Infant Jesus Teaching Hospital, Medical University of Warsaw. Five hundred ninety-seven patients undergoing unilateral primary THA in the five years from 2009 to 2014 were identified among the operated patients.
The exclusion criteria were: revision THA procedures, incomplete medical record, age under 18 years old, pregnancy, previous surgery of the operated joint, a diagnosis other than idiopathic OA (rheumatoid arthritis, post-traumatic osteoarthritis, developmental dysplasia of the hip, avascular necrosis, Legg-Calve-Perthes disease) or uncertain diagnosis of idiopathic OA. All patients received equivalent perioperative care.
Variables and data sources
The baseline data, including the information about comorbidities, were collected based on medical documentation in the form of medical history and operating room documentation obtained from the hospital archives and an electronic data register.
The preoperative evaluation focused on coexisting diseases and predictive factors belonging to the mFI-5 and mFI-11. Demographic and perioperative parameters such as age, gender, BMI, and hospitalization time were collected. Long-term results were evaluated during follow-up visits at the clinic.
During the follow-up visit, the research team collected data on the occurrence of complications after surgery, questionnaires evaluating the function of the operated limb, and the severity of pain. Long-term results of THA were evaluated with patient and physician reported outcome measures: Harris Hip Score (HHS) [12], the Western Ontario and McMaster Universities Index of Osteoarthritis (WOMAC) [13], the Visual Analogue Scale (VAS) [14], and Hip and Knee Arthroplasty Satisfaction Scale (HKASS) [15].
The WOMAC score was calculated from the Hip Osteoarthritis Outcome Score (HOOS) questionnaire according to the authors’ recommendation [16]. During the follow-up visits, an orthopedic examination was performed. Also, information on distant postoperative complications was collected.
The modified frailty index
The Canadian Study of Health and Aging (CSHA) on the epidemiology of dementia developed the 70-item CSHA-FI based on many deficits that may be associated with frailty. The simplified version consisting of eleven health deficits was created (mFI-11) because of the difficulties in measurement of each of the multiple factors and the fact that all CSHA-FI data was not uniformly collected. The mFI-11 was proven to reflect frailty as well as CSHA-FI. Later on, mFI-11 was simplified to the five-factor index mFI-5 [9]. The modified frailty index mFI-5 and mFI-11 can be calculated based on retrospective data from medical records. Table I explains the components of mFI-5 and mFI-11.
Table I
Prevalence of clinical conditions belonging to the modified frailty index-5 (mFI-5) and modified frailty index-11 (mFI-11)
The group of patients with arterial hypertension was identified based on the diagnosis in the medical record. The use of pharmacological treatment, for this reason, was necessary for qualification. Information about the partial or total inability to function independently was obtained based on the medical history (changes in everyday activities such as problems with getting dressed, bathing, personal grooming, cooking, going out alone).
Myocardial infarction was defined as the presence of diagnosis in medical history regardless of the onset time. Peripheral vascular disease was defined as lower limb varicose veins, resting pain, presence of necrotic lesions, state after revascularization, or amputation. Impaired sensorium was defined as cognitive disorders or disturbances of consciousness. The modified frailty index-5 (mFI-5) and modified frailty index-11 (mFI-11) values are calculated by dividing the number of health deficits present by the number of health deficits measured [9, 17].
Statistical methods
The probability distributions of individual variables were estimated for continuous parameters. To determine the normality of the distribution of the variables, the Shapiro-Wilk test and graphical analysis were used. The analysis of relationships between continuous parameters was performed using correlation analysis with Spearman’s R coefficient. The Mann-Whitney test was used to investigate the possible influence of other factors on the outcomes. The cutoff values for mFI-5 and mFI-11 were proposed by Dayama et al. [18]. The missing data were addressed with a complete case analysis method [19].
The results were found to be statistically significant at p < 0.05. The statistical analysis of the collected data was performed using Statistica version 13.
Results
Group characteristics
Three hundred sixty-five patients from the initial cohort met the eligibility criteria, including 57.26% women (n = 209) and 42.74% men (n = 156). The mean age at the time of surgery was 65.11 ±12.12 years (median 67; LQ 57; UQ 75). The mean BMI before surgery was 27.97 ±5.26 kg/m<sup>2</sup> (median 27.06; LQ 24.06; UQ 30.86).
One hundred nineteen arthroplasty procedures were performed with the use of bone cement (32.60%). The average hospitalization time among the examined patients was 16.39 ±5.91 days (median 15; LQ 12; UQ 19). One hundred fifty-three patients (41.92%) came to the follow-up visit after 1164.00 days. Clinical scales and postoperative complications were assessed in patients who completed the follow-up visit.
Frailty burden
The conditions predisposing to frailty were identified in 78.08% of patients for mFI-5 and 80.27% for mFI-11. The most common conditions were arterial hypertension, reported in 74.25% of patients (271), diabetes mellitus type II 19.45% (n = 71), and congestive heart failure 16.44% (n = 60). The prevalence of other clinical conditions belonging to mFI-5 and mFI-11 is presented in Table I.
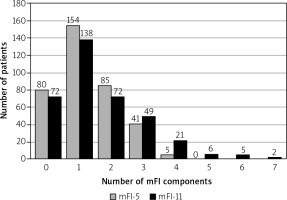
The values of mFI-5 (mean 0.26 ±0.19; median 0.20; LQ 0.2; UQ 0.4) and mFI-11 (mean 0.15 ±0.12; median 0.09; LQ 0.09; UQ 0.18) were characterized by very strong positive correlation (r = 0.93; p < 0.001). The distribution of mFI-5 and mFI-11 components in the investigated group of patients are presented in Figure 1.
Functional results
Patients with frailty (“mFI-5” and “mFI-11”) had significantly less satisfactory functional results (WOMAC). The correlation index was stronger for mFI-11 (r = 0.22; p < 0.05) than mFI-5 (r = 0.19; p < 0.05). Also, older subjects achieved a worse clinical outcome (HHS, WOMAC).
After the age adjustment the correlation for mFI-5 was r = 0.15, p = 0.07, and for mFI-11 r = 0.17, p < 0.05. The preoperative BMI and gender did not significantly correlate with postoperative function. The results are presented in Table II.
Table II
The clinical results after total hip arthroplasty
| Parameter | mFI-5 | mFI-5# | mFI-11 | mFI-11# | Age | BMI |
|---|---|---|---|---|---|---|
| HHS | –0.12 | –0.05 | –0.15 | –0.09 | –0.31*** | –0.14 |
| VAS | 0.09 | 0.08 | 0.10 | 0.08 | 0.10 | 0.04 |
| WOMAC | 0.19* | 0.15 | 0.22** | 0.17* | 0.20* | 0.12 |
| HKASS | –0.05 | –0.07 | –0.08 | –0.10 | –0.05 | –0.05 |
[i] HHS – Harris Hip Score, HKASS – Hip and Knee Arthroplasty Satisfaction Scale, mFI-5 – modified frailty index-5, mFI-11 – modified frailty index-11, VAS – Visual Analogue Scale, WOMAC – Western Ontario and McMaster Universities Osteoarthritis Index, Spearman’s R coefficient; * p < 0.05, ** p < 0.01, *** p < 0.001, # age-adjusted.
Patients subjected to cementless THA achieved a better clinical outcome (HHS) (p < 0.01). Patients who experienced complications in the follow-up period had a less satisfactory clinical outcome (HHS) (p < 0.05) (Table III).
Table III
Patient- and physician-reported outcome measures after total hip arthroplasty
Length of stay
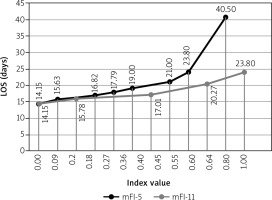
There was a positive correlation between mFI-5 and the length of stay in the hospital (LOS) (r = 0.25; p < 0.001). A stronger positive correlation was confirmed for mFI-11 (r = 0.29; p < 0.001) (Fig. 2). The patients’ age also correlated positively with the LOS (r = 0.12; p < 0.05). The correlations were also confirmed for the age-adjusted mFI-5 (r = 0.22; p < 0.001) and mFI-11 (r = 0.27; p < 0.001). There was no significant correlation between BMI value and the LOS. The LOS did not differ significantly by gender.
Postoperative complications
The overall incidence of complications was 18.30% (n = 28). The most common complication was paresthesia within the operated limb in 8.50% (n = 13) of patients. Surgical site infections (SSI) rate was 4.58% (n = 7), while the prosthetic joint infection (PJI) incidence was 3.27% (n = 5). Aseptic loosening occurred in 3.92% (n = 6). The incidence of dislocation of the head of the endoprosthesis was 3.27% (n = 5). There were no cases of THA periprosthetic fracture in the cohort during the observation period. Patients with mFI-5 above the median (0.2) experienced complications more often (15.96% <i>vs</i> 20.69%; p > 0.05). Similarly, patients with mFI-11 over the median (0.09) had a higher complication rate (16.67% <i>vs</i> 19.12%; p > 0.05). In both cases, the difference was not statistically significant. The analysis did not prove the influence of other factors on the satisfaction (HKASS) and the severity of pain (VAS) after the procedure (Table III).
Discussion
Total hip arthroplasty not only relieves pain and improves function and quality of life but may also increase the life expectancy [20]. Although it is one of the most successful surgical procedures worldwide, multiple variables may contribute to THA results. Traditional outcomes of the surgical procedures are mortality, readmission, complications, surgical recovery time, and return to work.
Nowadays, researchers highlight the importance of patient-centered outcomes such as functional status, degree of disability, emotional and mental health, and social interaction. Total hip arthroplasty results can be influenced by both patient-independent (e.g., prosthesis type, surgeon experience, hospital type) and patient-related factors (e.g., age, comorbidities, BMI, OA severity, patients’ expectations, preoperative function and health-related quality of life) [21].
Although total hip arthroplasty is one of the most common orthopedic procedures in older adults, studies of the frailty and THA results are limited to the traditional outcomes [7]. In this study, we analyzed the complex impact of frailty on the outcomes of THA focusing on patient-centered outcome measures such as long-term function (WOMAC, HHS), pain sensations (VAS), and satisfaction (HKAAS). We also analyzed traditional outcomes such as surgical recovery time (LOS) and complication rate.
The systematic review of possible factors affecting short-term and long-term functional outcomes of THA indicated the negative association of high BMI, presence of comorbidities, and older age with function after the surgery. There is a positive association between factors such as physical function, mental health, and the functional outcome after THA. The relationships of gender, alcohol consumption, socioeconomic status, allergy, and vitamin D insufficiency and functional outcome after THA are unclear [22].
Meessen et al. [23] studied the impact of frailty (Groningen Frailty Indicator, GFI) on the functional outcomes after THA and total knee arthroplasty (TKA). In the regression analysis, the GFI had limited ability to affect the functional outcome change (HOOS) in THA patients. However, higher rates of reoperation complications and reoperation were observed in frail patients.
Schmucker et al. [7] performed a systematic review of the impact of frailty on outcomes after THA and TKA.
Only one study, by Oosting et al. [24], has assessed the functional outcome after THA (HOOS) and frailty. Although the study was mainly focused on the assessment of preoperative training on the functional in the preselected group of frail patients [7, 24]. The modified frailty index accesses mainly the patient’s multimorbidity and the literature supports the influence of coexisting diseases on THA results.
In the study by Judge et al. [25] subjects with coexisting diseases achieved a less satisfactory clinical outcome during a five-year follow-up (Oxford Hip Score).
Wang et al. [26], in a multivariate regression analysis of 12 factors, confirmed the independent influence of comorbidities on the functional outcome (WOMAC). Also, Smith et al. [27] reported the negative effect of ASA status on HHS.
In our study, we proved the association between frailty and functional outcomes (WOMAC). After the age adjustment, mFI-11 was a successful predictor of functional outcome. However, the relationship between mFI and functional outcomes is weak, and this indicates the complexity of factors that can affect the THA outcomes.
Okafor et al. [28] performed a systematic review of patient satisfaction and total hip arthroplasty. The studied factors included patient expectations, age, gender, pain, length of stay, and comorbidities before the surgery. Younger age is often associated with a lower satisfaction rate as patients have higher expectations and an active lifestyle. The influence of multimorbidity and comorbidities on satisfaction after THA has been studied. However, the results are inconclusive. The authors hypothesize that patients with multiple comorbidities experience a high rate of complications, and it can contribute to poor satisfaction after THA [28].
In our study, the overall satisfaction (HKASS) after THA was not affected by frailty. Understandably, patients with any THA-related complications were significantly less satisfied. The regression analysis showed that frail and pre-frail older adults in the community setting more often experience chronic pain [29].
Esses et al. [30] performed a secondary analysis of a prospective observational cohort (PRESERVE). The authors investigated frailty and its association with postsurgical pain in older patients. The frail patients were at five times higher risk of intense post-surgical pain compared to non-frail patients, but this cohort did not include THA patients [30]. We found no study on the impact of frailty on pain after the THA.
Schmucker et al. [7] suggest that frailty may impact long-term pain and function after total joint replacement. However, there is a lack of evidence for their hypothesis.
Length of stay (LOS) is one of the factors which would be considered in terms of both patients’ benefits and economic burden. It is one of the most common outcome measures used to assess the patients’ surgical recovery time [31]. Over the years, LOS after THA has decreased due to the dedicated protocols for rapid recovery and early discharge [32]. Patient-related factors such as comorbidities can significantly influence the LOS and hospital costs, but the evidence is limited [33].
Foote et al. [34] performed a multivariate analysis of factors influencing the LOS after THA. Older age, higher ASA, prolonged surgery time, and extensive incisions were significantly associated with delayed discharge. However, patient-independent variables can also be involved in the patients’ discharge.
Husted et al. [35], in a nationwide study in Denmark, identified the logistical and clinical features of the facility to influence LOS rather than demographic factors and comorbidities. The multimodal opioid-sparing analgesia protocols, early mobilization, quick rehabilitation, and clear criteria for discharge can attribute to LOS reduction [35]. Still, emphasis should be placed on modifiable patient-related factors that can affect LOS such as high glucose and creatinine level, hypotensive events, and postoperative anemia [36]. There is evidence that frailty can also be a significant predictor of LOS.
In the study by Bellamy et al. [37], higher mFI-11 was associated with prolonged LOS after THA. Similarly, in our study, increased mFI-5 and mFI-11 were associated with longer LOS regardless of age. In our cohort, mean LOS was relatively long, as it was before reorganization and improvement of admitting and preparing patients for the surgery.
According to Johnson et al. [38], frailty increases the risk of wound complications, hematoma, infection, dislocations, and reoperation in THA patients. The mortality rate is also higher among frail patients [38].
Bellamy et al. [37] suggest that mFI is an effective risk assessment tool in the decision-making in THA patients. Patients with increased mFI-11 had a significantly elevated risk of complication, readmission, reoperation, and mortality after THA. Also, the mFI-5 was a successful predictor for complications, readmission rate, and mortality in a retrospective analysis of patients subjected to THA [39].
However, in our study, we did not prove the increased complication risk in patients with high mFI-5 and mFI-11. The possible cause is that the group of patients in our study was relatively small compared to the two retrospective analyses mentioned above.
A potential bias in the study is that coexisting diseases may be underreported in medical history, especially when surgical specialties coding of diagnoses in the documentation. However, our dedicated team put particular emphasis on the quality and accuracy of the data entered [40]. Also, some inaccuracies may have arisen between the original version of mFI-5 and mFI-11 and the one used, due to different diagnostic criteria for specific diseases in the United States.
Conclusions
The study assessed the hypothesis that patients burdened with frailty (mFI-5; mFI-11) subjected to THA achieve less satisfactory clinical outcomes. Analysis of the collected material confirmed the hypothesis of worse functional results in frail patients (WOMAC). After the age adjustment, the mFI-11 was found to be a better indicator of patients’ health status than mFI-5.
Less satisfactory functional results were also observed in older patients (WOMAC, HHS). Higher frailty burden was associated with longer LOS, regardless of age (mFI-5; mFI-11).
Table IV summarizes the key points of the study. The mFI is a useful clinical tool, and it can be helpful in prospective detection of patients at risk of poor functioning after THA.
Table IV
Summary of lessons learned from the study on frailty and the total hip arthroplasty results