Introduction
Since 1982, isotretinoin (13-cis-retinoic acid) has been proposed as a first-line therapy in patients with moderate to severe acne vulgaris (AV) [1]. Sacroiliitis is an uncommon adverse event following therapy with isotretinoin [2–4]. Patients with AV can suffer from sacroiliitis even though they do not use isotretinoin, particularly in the severe form named ‘acne fulminans’ [5].
We report the case of a male patient complaining of inflammatory back pain due to sacroiliitis following treatment with isotretinoin, who had a complete disappearance of pain following drug withdrawal. We carried out a literature search in order to assess the relevance of the relationship between oral isotretinoin and sacroiliitis in everyday clinical practice.
Material and methods
We performed a search through PubMed Medline (OVID interface), EMBASE, Scopus and Web of Science, for articles published in any language up to 10th July 2022. We used the following search terms: isotretinoin, sacroiliitis, isotretinoin-induced sacroiliitis, drug-induced sacroiliitis, acne vulgaris, acne fulminans. Reviews, conference abstracts and comments were excluded.
We scanned each review’s reference list for additional articles meeting the aim of this study. When manuscripts reported data partially presented in previous articles, we considered only the most recent data.
Case description
Written informed consent for publication was obtained from the patient.
A 30-year-old male patient was admitted to our clinic complaining of pain in his right hip. This pain had appeared about two months earlier. There was no history of fever, weight loss, inflammatory bowel disease or psoriasis, and the patient did not smoke or drink alcohol. The patient weighed 60 kg.
When the patient’s history was reviewed, we learned that the low back pain had an inflammatory character, and that he had been using isotretinoin at a dose of 30 mg/day for 4 months for AV. Acne was not present at the time of the visit.
On physical examination, lumbar movements were painful and unrestricted at the end of flexion and extension. The clinic tests used to diagnose pathologies of the sacroiliac region, i.e. FABER, FADIR, sacroiliac compression, Gaenslen and Mennel tests, were all positive. Neurological examination was normal.
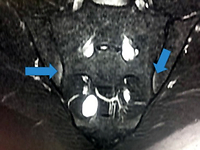
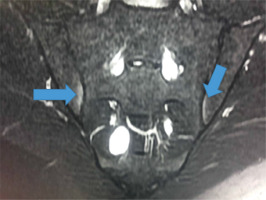
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level were normal. Brucella agglutination tests and histocompatibility leucocyte antigens B27 (HLA-B27) were negative. In the sacroiliac magnetic resonance imaging (MRI), prominent subcortical mild bone marrow edema was detected on the iliac face inferior to both sacroiliac joints (Fig. 1).
Fig. 1
Magnetic resonance imaging of the sacroiliac joint shows subcortical mild bone marrow edema on the iliac face inferior to both sacroiliac joints (see arrows).
Discontinuation of treatment with isotretinoin resulted in complete disappearance of pain. After a 7-months follow-up, we found no additional musculo-skeletal manifestations. Sacroiliac MRI was not repeated.
Results
Fifteen case reports and case-series met our inclusion and exclusion criteria [3, 4, 6–18], shown in Table I.
Table I
Isotretinoin-induced sacroiliitis: case reports and case series according to our literature search
| Author | Year | Patients [number] |
|---|---|---|
| Bachmeyer et al. [6] | 2003 | 1 |
| Eksioglu et al. [7] | 2008 | 1 |
| Dinçer et al. [8] | 2008 | 3 |
| Rozin et al. [9] | 2010 | 1 |
| Levison et al. [10] | 2012 | 1 |
| Kocak et al. [3] | 2017 | 11 |
| Baykal Selçuk et al. [4] | 2017 | 6 |
| Dawoud et al. [11] | 2018 | 1 |
| Coskun et al. [12] | 2019 | 2 |
| Taheri et al. [13] | 2020 | 5 |
| Mulkoglu et al. [14] | 2020 | 1 |
| Cheng et al. [15] | 2020 | 1 |
| Karadağ et al. [16] | 2020 | 4 |
| Ozdel et al. [17] | 2020 | 2 |
| Seyman Civelek et al. [18] | 2022 | 11 |
We found only one large study performed on 513 AV patients receiving isotretinoin [19]. The first report of an association between isotretinoin and sacroiliitis dates back to 2003: an 18-year-old man with acne fulminans suffered from bilateral sacroiliitis following treatment with isotretinoin. When isotretinoin was withdrawn, pain in the hips improved; however, pain reappeared 48 hours after reintroduction of the drug [6].
Discussion
Sacroiliitis is a hallmark of seronegative spondyloarthropathies. However, it also may be associated with inflammatory bowel diseases or infections such as brucellosis and tuberculosis [20]. In addition, positive sacroiliac screening tests may account for as many as 20% of asymptomatic persons in the general population [21].
Our literature search highlighted that sacroiliitis had been reported as an adverse event following isotretinoin treatment, but it had never been reported in association with other drugs. The mechanism of retinoid-related sacroiliitis is still unclear.
It has been suggested that isotretinoin causes some changes in the lysosomal membrane structure of cells, making synovial cells prone to degenerative processes and more susceptible to mild trauma. Reports of sacroiliitis in AV athletes treated with isotretinoin may be in favour of this hypothesis [8]; however, microtrauma can cause sacroiliitis itself [20].
Sacroiliitis following treatment with isotretinoin usually resolves with discontinuation of therapy. In the Bachmeyer et al. [6] case report, hip pain recurred 48 hours after the reintroduction of the drug. In our patient, as well as in all the other case reports we found in literature, isotretinoin was never reintroduced.
Is the link between isotretinoin and sacroiliitis causal or coincidental? How was sacroiliitis following isotretinoin therapy evaluated as an adverse drug reaction (ADR)? Only clinical judgment was used in all the listed case reports and case-series, without the use of scales or algorithms.
The ADR Probability Scale developed by Naranjo et al. [22] in 1981 is commonly used in clinical practice to standardize causality assessments. This scale assesses the probability that an adverse event is related to drug therapy using a list of 10 weighted questions that examines some variables, such as temporal association with the drug administration and event occurrence; alternative causes if any; drug levels; and previous patient experience with the same drug. The significance of the sum of the scores is listed in Table II.
Table II
Naranjo et al.’s adverse drug reaction probability scale: sum of the scores and their significance [modified 22]
| Adverse drug reaction probability scale |
|---|
To date, Naranjo’s scale has repeatedly documented a significant increase in inter- and intra-rater agreement compared with standard clinical examination alone [23]. When, using reported data, we were able to apply Naranjo’s scale to the listed case reports and case-series, total scores were almost never > 4.
In a prospective longitudinal cohort study performed on 513 acne patients, MRI-proven sacroiliitis was detected in about 50 symptomatic patients and MRI findings completely resolved within a mean period of 6.27 ±1.7 months after isotretinoin discontinuation [19].
In another cross-sectional study, 11.7% of 94 acne patients under isotretinoin treatment had MRI sacroiliitis. All the patients with sacroiliitis were completely symptom free at the sixth month after discontinuation of the drug [24].
These studies suggested that isotretinoin-induced sacroiliitis may be underdiagnosed in a real-world setting, and they proposed that in patients using isotretinoin a first diagnosis of primitive axial spondyloarthropathy should be revised afterstopping isotretinoin.
Study limitations
Our case-based review has some limitations. We decided not to follow the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) protocol and it is possible that we missed some data during our literature search. At the same time, we scanned all the articles we found regardless of their scientific quality. The evaluation of the latter was not our aim. Finally, the non-repetition of sacroiliac MRI did not allow us to report the radiological disappearance of the sacroiliitis.
Conclusions
According to our literature search, isotretinoin-induced sacroiliitis may be much more frequent than commonly assumed. Our clinical observation also highlights this problem.
It is recommendable to consider in patients taking isotretinoin and having hip or low back pain or even sacroiliitis whether the drug might have been not responsible for these symptoms.
In acne patients using isotretinoin, the first diagnosis of axial spondyloarthropathy should be revised after the discontinuation of isotretinoin, as the related clinical and MRI findings may be reversible.