Introduction
Rheumatoid arthritis (RA) is a chronic, systemic, autoimmune, inflammatory disorder of unknown etiology that primarily involves synovial joints. The arthritis is typically symmetrical, and if uncontrolled leads to destruction of joints due to erosion of cartilage and bone, causing joint deformities. The disease usually progresses from the periphery to more proximal joints and results in significant locomotor disability within 10 to 20 years in patients whose disease does not respond to treatment. It is a painful and disabling condition that is associated with higher mortality rates than the general population [1–3]. When left untreated, long-term RA can result in significant disability. Additionally, many patients suffering with this condition may face multiple social and psychological stressors. Depressive disorders have long been regarded as a comorbidity of RA which increases mortality and morbidity [4]. Depression is frequently seen in patients with RA, and individuals with RA with depression have increased pain, fatigue, and disability compared to those without depression [5]. The pooled prevalence of major depression in patients with RA is 17%; however, Patient Health Questionnaire-9 based prevalence of major depression is 39% in patients with RA [6]. In India depression associated with RA is a serious public health concern and the prevalence ranges between 14.8% and 66.2% [6, 7].
The disease activity in individuals with RA directly correlates with their mental health and standard of living [8]. Psychological distress plays an important role in the disease progression as well as affecting the treatment response in people suffering from RA. Patients who perceived RA as an illness with serious negative consequences were found to experience high levels of anxiety, whereas those who experienced more primary symptoms of the disease were more likely to suffer from depressive symptoms [9, 10]. The high prevalence of major depressive disorders (MDD), social phobia, panic disorder, and anxiety in patients with RA has been reported in the literature [11]. In addition, the number of comorbidities in RA may interfere with treatment and complicate it further. Therefore, it is important to recognize such comorbidities and set achievable therapeutic goals, which may require additional medications and a multiprong approach [12]. The majority of studies on neuropsychiatric health are from Western countries, and there is a lack of research on the prevalence of psychiatric morbidities among Indian patients with RA. Understanding the prevalence of psychiatric comorbidities in RA patients can aid healthcare professionals in developing more effective interventions to manage both the physical and mental health of these patients. Therefore, there is a need for more evidence-based research on psychiatric morbidities associated with RA among the Indian population. Hence, the present prospective study was conducted to find the pattern of psychological disorders associated with RA.
The aim of the study was to systematically investigate and analyze the patterns and prevalence of psychiatric morbidity among individuals diagnosed with RA, with the aim of identifying common mental health conditions, understanding the interplay between RA and psychiatric disorders, and providing valuable insights for improved holistic patient care.
Material and methods
Study population
This was a cross-sectional observational study conducted at Shifa hospital and V Care super specialty clinic in Srinagar, India over the course of three years (January 2019 to January 2022).
Patients
Inclusion criteria
The study included patients of either sex, aged 17 years or older, diagnosed with RA, who were on treatment for RA.
Diagnostic evaluation
Confirmation of the diagnosis of RA was based on specific constitutional symptoms and signs, radiological examination (bone radiograph), and blood investigations. The diagnosis of RA was confirmed using 2010 American College of Rheumatology/European Alliance of Associations for Rheumatology (ACR/EULAR) diagnostic criteria for RA [13]. The socio-economic status was established by the Kuppuswamy scale [14]. The RA Disease Activity Score with 28-joint count with erythrocyte sedimentation rate (DAS28 [ESR]) was used to calculate disease activity with help of the application RheumaHelper [15]. The patients were interviewed for socio-demographics related to age, sex, marital status, religion, education, and occupation and all of this information was entered into a database and maintained for the registry. Prior to screening for any psychiatric diagnosis, a detailed history, physical examination, and relevant investigations were conducted by a dedicated psychiatrist. For the diagnosis of psychiatric morbidity, Mini-International Neuropsychiatric Interview Schedule PLUS (MINI PLUS) was used [16]. The standard of care treatment was followed for management of RA. Synthetic disease-modifying anti-rheumatic drugs (DMARDs) were given to 650 patients (65%); they included methotrexate (MTX; mean dose of 15 mg weekly), hydroxychloroquine (HCQ) 400 mg in 2 divided doses daily, leflunomide 20 mg single dose daily was added to patients who did not respond to MTX and HCQ and low dose glucocorticosteroids were used as bridge therapy. Biological DMARDs (bDMARDs) were prescribed to 190 (19%) patients, Janus kinase inhibitor tofacitinib 5 mg or 11 mg was added to 97 patients (9.7%) and 63 patients (6.3%) were given rituximab in addition to MTX as these patients had refractory disease.
Statistical analysis
Data were analyzed using SPSS Statistics software, version 23.0. Quantitative data were presented as number and percentages.
Bioethical standards
The study was conducted in accordance with ethical principles consistent with the Declaration of Helsinki, International Conference on Harmonization Good Clinical Practices, and the applicable legislation on non-interventional studies. The study protocol was approved by the Ethical Committee reference No: 109/GMC/IEC/ICMR (Dated: 15/12/2018) prior to commencement of the study. Written informed consent was obtained from all study participants.
Results
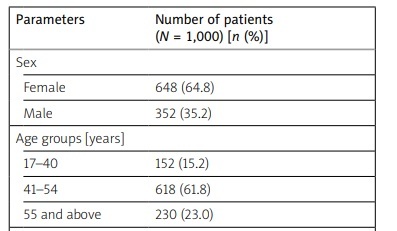
During the study period of three years 1,000 patients diagnosed with RA were examined for disease activity and psychiatric comorbidities. The majority of patients were female: 648 (64.8%). The mean duration of disease was 9.4 years, the minimum 6 weeks and the maximum 29 years. Among 1,000 studied patients, 618 (61.8%) were in the age group of 41 to 54 years, followed by 230 (23%) in the age group 55 years and above and 152 (15%) in the age group 17 to 40 years; 62.0% were married, 35.0% were unmarried, and the remaining 3.0% were divorced. In terms of occupation, 47.5% of patients were unemployed, 27.0% were salaried, 19.0% were businessman, while 6.5% were students (Table I).
Table I
Demographic details of patients with rheumatoid arthritis
According to DAS28, 258 patients (25.8%) had mild disease activity (DAS28 < 3.2), 532 patients (53.2%) had moderate disease activity (DAS28 = 3.3–5.1), and 210 patients (21.0%) had severe disease activity (DAS28 ≥ 5.1).
The prevalence of psychiatric comorbidities that were evaluated is depicted in Table II. Major depressive disorder was the most commonly observed comorbidity (n = 410; 41.0%), followed by somatoform disorder (n = 285; 28.5%), and generalized anxiety disorder (n = 135; 13.5%). One hundred and seventy patients (17.0%) were free of any psychiatric disorder.
Table II
Disease activity and observed psychiatric comorbidities among patients with rheumatoid arthritis
The prevalence of MDD in patients aged under 55 years was 47% compared to 21.3% in patients aged over 55 years.
The prevalence of depression among patient with low disease activity was 31.7% (82 patients out of 258), 36.8% (196 patients out of 532) in patients with moderate disease activity and 62.8% (132 patients out of 210) in patients with high disease activity. The results of χ2 analysis revealed a significant association between disease activity and prevalence of depression Table III.
Table III
Results of χ2 analysis
The prevalence of GAD in the age group less than 41 years was 21% compared to 12% in individuals aged over 40 years of age.
Discussion
Psychiatric disorders such as depression, anxiety, and somatic symptoms exert a strong influence on the quality of life [17]. In this study, we aimed to estimate the pattern and prevalence of psychiatric comorbidities in patients with RA. The DAS28 scores used for disease activity revealed 25.8% had mild disease activity, 53.2% had moderate disease activity, and 21.0% had severe disease activity (DAS28 ≥ 5.1). The presence of comorbid psychiatric disorders poses an additional burden of illness. It was surprising that almost 80% of participants reported some degree of psychological distress in the form of major depression, somatoform disorders, and generalized anxiety disorder, which is one and half times more than reported in the literature [18]. This analysis also revealed a 41% prevalence of major depression among patients with RA and the majority of them belonged to the age group of 41–54 years with predominant female sex. Several studies have demonstrated that RA is more prevalent in women [19]. In the present study, the proportion of female sex was 64.8%, which is consistent with previous studies [20, 21], where the proportion of women was 64.0% and 75.5% respectively [18]. In fact, globally the pattern is the same, with women predominantly affected by RA [22]. In addition a population- and patient-based observational study in the past also revealed higher prevalence of RA in women as compared to men [23]. These sex-based differences in incidence and prevalence of RA have been postulated to be likely related to sex hormones. The serum androgen level has been inversely correlated with the severity of RA; therefore the severity of RA is lower in men [18]. Moreover, another possible explanation could be delayed treatment in women with early arthritis compared to men [24].
In the present study although the overall prevalence of depression was 41%, the prevalence was much higher (47%) in the young age group with age less than 55 years compared to the age group of more than 55 years, which was only 21%, which reflects the need for intervention to prevent the loss of productivity in this productive age. The low prevalence of major depression in aged patients may not necessarily be a good thing; it is possible that those patients with depression and RA have high mortality and may not reach this advanced age, which will decrease the prevalence of depression in this age group as depression has been linked to increased mortality in RA, with the proportion of mortality attributable to depression 6.9% [25], or it could simply be that patients stop worrying about the illness and get adapted to the illness. Similar results have been reported in a previous cross-sectional study conducted at a multi-center level in India, which reported high prevalence of depression in a young adult age group of 40–59 years, patients with RA [26]. Among previous studies from India that evaluated RA prevalence, the National Mental Health Survey (NMHS) study revealed high prevalence of RA with depression among patients aged 40–59 years compared to older adults [27]. Age-stratified analysis also suggests that the depressive disorders are more prevalent among patients with RA in young age (40–55 years) in Indian adults [28].
The present study found that 53.2% of the patients had moderate disease activity, while 25.8% and 21.0% of patients had mild and severe disease activity respectively, based on their DAS28 (ESR) scores. This is in contrast to the previous noteworthy study in the Indian literature, which reported that 69.4% of patients had moderate to severe disease activity scores [29].
Major depressive disorders are known to be associated with detrimental health behavior with physical inactivity and patients with RA experience an increased risk of MDD [30]. A meta-analysis of past studies showed that the prevalence estimates for depressive disorders in patients with RA range between 14 and 48% while MDD occur in 16.8% of RA patients [31]. In the present study MDD were more prevalent than other psychiatric disorders such as somatoform disorder, panic disorder, and generalized anxiety disorder in patients with RA. A recently published cross-sectional study revealed that patients with RA were more prone to develop depressive disorder than other psychiatric disorders [32]. Only one study has demonstrated a higher prevalence rate of an anxiety disorder (52.0%) among people with RA; in addition this study revealed that there was no significant correlation between anxiety symptoms and disease activity [33]. In one study, the prevalence of anxiety disorder was 13.5% [34], which is consistent with our study with the prevalence of anxiety disorder being 13.5% in patients with RA who meet the criteria for generalized anxiety disorder. The results from our study reveal that the disease activity is directly proportional to the prevalence of depression. The prevalence of depression in mild, moderate and severe disease activity respectively was 31.7%, 36.8% and 62.85. The result from a previous prospective study reveal that both depression and anxiety symptoms are associated with an increased DAS28 score in patients with RA [21, 35].
Limitations
The present study has three significant limitations. Firstly, due to its clinic-based nature, the findings cannot be extrapolated to the wider Indian population. Secondly, the study did not record management of these depressive morbidities, which could have added valuable data while inferring the observations. Thirdly, recall bias cannot be ruled out in the duration of disease parameter.
Conclusions
In view of high psychiatric morbidity associated with RA, there is enough scope for psychiatric services to be made available to these patients. In addition, personnel involved in the treatment of these patients should be trained for early detection of psychiatric symptoms for better treatment outcomes. Remission in RA leading to improved function will keep reducing the burden of depression in RA.