Introduction
Osteoarthritis (OA) is the most common joint disease in the world, becoming more prevalent with increasing age, and causes a significant burden on individuals and society [1]. Osteoarthritis affects 60% of men and 70% of women in the seventh decade of life. After ischemic heart disease, OA is the most common cause of disability.
The knee joint, one of the most critical joints in the body, is affected by various inflammatory and degenerative diseases that eventually lead to the destruction of articular cartilage and loss of proper joint function. The patient presents with pain, joint instability, limited range of motion, and deformity [2].
The main pathological findings in OA include abnormalities in the repair stages of intra-articular tissue, involvement of large joints, extensive destructive changes with articular cartilage loss, and capsular hypertrophy. Etiologically, this disease may have biological, mechanical, and biomechanical causes [3].
In the final stages of the disease or when severe pain interferes with a person’s life, surgical intervention such as joint replacement becomes necessary [4].
So far, several factors have been identified in association with OA of the knee joint. Age is the most crucial uncontrollable risk factor for OA. The prevalence of OA increases with age [5].
The type of joint involvement before 55 years old is the same in both genders. Although hand joints are the most frequently involved joints in women with increasing age, the hip joints are more commonly affected in men [6, 7]. Race, genetics, and sex hormones are other factors associated with knee OA [8].
Due to the high prevalence of polyarticular OA in women over 50 years old, a link between OA and estrogen deficiency has been suspected. Studies has shown that estrogen replacement therapy reduces the risk of OA in the hip and knee [9, 10].
Obesity is another risk factor for developing OA, especially in the knees [11]. Severe joint trauma, excessive pressure on the joint from physical activity, congenital anomalies or defects, inflammatory or septic joint disease, and endocrine or metabolic disorders, such as diabetes, hyperparathyroidism, and acromegaly, are also associated with OA [12].
The knee is the most common joint affected by OA, with a prevalence of 13.9% in adults [13]. The knee is divided into three parts: the internal tibiofemoral, the external tibiofemoral, and the patellofemoral regions. The internal and the patellofemoral parts are more often affected individually or together [13].
Numerous pathologies are involved in developing this condition, including meniscal damage, focal loss and proliferation of articular cartilage, and changes in the subchondral bone. Pain is the most important and debilitating manifestation of this disease. To date, the exact cause of this symptom in the peripheral joints has not been determined.
Advanced cases of OA are easily detected on radiographs, but the early stages of degenerative changes, including meniscal defects, joint defects, and soft tissue abnormalities, as well as OA-prone bone changes, need to be evaluated by MRI [14].
Studies have shown that the patella is significantly less likely to develop OA when placed in the trochlear cleft without malalignment. Malalignment of the patella increases the stress on the articular surface and can lead to degenerative changes in the knee [15, 16].
To date, most studies have examined the alignment of the patella on the radiograph. Factors measured on the graph for this purpose include the relationship between the length of the patella and the length of the patellar ligament on the lateral graph and examination of the trochlear angle of the sulcus, the lateral patellofemoral angle, and the lateral tilt of the patella on the skyline radiograph [17].
Few studies have examined patellofemoral alignment in MRI images. Patellofemoral misalignment on MRI may indicate the risk of OA in the knee joint and is of diagnostic value when associated with other clinical findings [18].
Therefore, we aimed to conduct a study to evaluate the association between patellofemoral alignment and OA findings of the knee on MRI, considering age segregation. This cross-sectional study investigates the prevalence of patellofemoral joint malalignment in the study population.
On the other hand, by examining the incidence of patellofemoral joint OA whose early symptoms can be detected by MRI, the relationship between the incidence of OA and the degree of joint alignment is investigated.
Material and methods
Study population
This cross-sectional study was conducted from March to August 2017 at Imam Reza Hospital, affiliated to Mashhad University of Medical Sciences (MUMS). We evaluated 418 MRI scans of the knee joint performed at the MRI center of Imam Reza Hospital. Checklists of medical history, underlying disease, history of surgery or trauma, age, gender, weight, height, and history of osteoporosis were completed for all patients.
Images showing knee trauma or tumor lesions, patients under 15 years old, and joint effusions greater than one centimeter in the midsagittal section were excluded. The remaining patients (n = 277) were divided into two groups based on age, under 50 years old and over 50 years old.
The images were examined for OA findings in groups. Patients without abnormalities in articular cartilage morphology were included in the control group, and patients with symptoms of OA were included in the patient group. The study design followed the Declaration of Helsinki and was approved by the Ethics Committee of Mashhad University of Medical Sciences (ethics code: IR.MUMS.fn.REC.1396.121.).
Magnetic resonance imaging evaluations
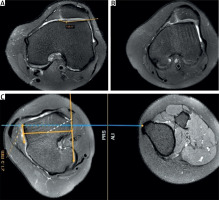
The extent of joint damage is classified into five grades (0 to 4) according to the International Cartilage Repair Society (ICRS) classification system (grade 0: normal, grade 1: increased cartilage signal with normal articular surface, grade 2: 50% > partial-thickness defect, grade 3: 99–50% partial-thickness defect, grade 4: full-thickness defect with exposure of subchondral bone and bone marrow edema).
All MRI images in all five groups were evaluated for patellofemoral joint alignment and degree of joint damage. First, the images were downloaded from PACS of Imam Reza Hospital and then examined using the Radiant program. The following indices were measured for evaluation of joint alignment: femoral sulcus angle – SA, femoral sulcus depth – SD, lateral patellar displacement – LPD, lateral patellofemoral angle – LPFA, Insall-Salvati index, tibial tubercle-trochlear groove – TTTG.
Among the axial MRI images, three images were selected as references: the first image at the level of the largest anterior-posterior diameter of the femoral condyle, the second image on the surface of the largest transverse diameter of the patella, the third image on the surface of the patellar tendon’s origin on the tibial tubercle.
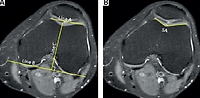
Lines A, B, C were drawn on the image. Line A is parallel to the anterior surface of the femoral condyles between the innermost and outermost points of the trochanter. Line B runs along the posterior surface of the femoral condyles, and line C is drawn perpendicular to line A from the outermost point of the trochanter (apex of trochanter).
Femoral sulcus depth and SA parameters were measured in image I. Lateral patellofemoral angle and LPD parameters were measured on image II (Fig. 1A–C). Lateral patellofemoral angle and LPD parameters were measured on image II (Fig. 1D, E). Lateral patellar displacement is the distance between two lines, one perpendicular to line A (line D) from the innermost point of the patella and the other perpendicular to line A (line E) from the innermost point of the trochlea.
Fig. 1
Reference images for measuring the values of femoral sulcus angle, femoral sulcus depth, lateral patellofemoral angle, lateral patellar displacement, tibial tubercle-trochlear groove and Insall-Salvati index. Line A (A), parallel to the anterior surface of the femoral condyles between the innermost and outermost points of the trochanter. Line B runs along the posterior surface of the femoral condyles. Line C, drawn perpendicular to line A from the outermost point of the trochanter (apex of trochanter); femoral sulcus angle was measured (B), femoral sulcus depth was measured (C), lateral patellar displacement was measured (D). Line D, one perpendicular to line A from the innermost point of the patella. Line E, perpendicular to line A from the innermost point of the trochlea; lateral patellofemoral angle was measured (E), tibial tubercle-trochlear groove was measured (F). Line F, parallel to line C from the innermost point of the origin of the patellar tendon on the tibial tubercle. Patellar length and patellar tendon length were measured.
Line A is copied from image I to image II. The results are positive if line D is lateral to line E. The line measuring the LPFA is drawn between the apex and the outer subchondral border of the patellar cortex and its angle with line A was measured. The results are considered positive if the angle opens to the lateral side.
The tibial tubercle-trochlear groove is measured on image III. In Figure 1G line F is drawn from the innermost point of the origin of the patellar tendon on the tibial tubercle parallel to line C. The distance between lines F and C is recorded as TTTG.
The Insall-Salvati index is evaluated using the midsagittal image. The maximum patella length (PL) and patellar tendon length (PTL) are measured, and the PTL/PL ratio is calculated (Fig. 1G).
Statistical analysis
Data were analyzed using SPSS version 23. The independent sample t-test or Mann-Whitney test was used to compare the groups according to the distribution of the variables. The qualitative variables in the groups were compared using the χ2 test. P-value > 0.05 was considered significant.
Results
Of the 438 patients enrolled in the study, among them 150 were excluded due to severe trauma, bone tumor, evidence of knee surgery, or significant joint effusion and 11 were excluded due to age less than 15 years old. Finally, 277 patients were evaluated. The mean age of patients was 36.8 ±13.3 years, and 110 (36.7%) were female. Articular cartilage morphology data have been reported in the form of joint injury grading. Table I shows the characteristics of patients.
Table I
Baseline demographic data
Patients were divided into two groups based on the severity of cartilage injury. Patients with normal articular cartilage (grade 0) were in the healthy group, and other patients with articular cartilage injury were included in the OA group. Based on the results, 81 (28.9%) of the patients showed joint cartilage damage (grade 1–4). Table II shows the comparison of characteristics between the two groups.
Table II
Comparison of demographic data between healthy and osteoarthritis groups
| Variables | Healthy group | Osteoarthritis group | p-value |
|---|---|---|---|
| Gender | |||
| Male | 137 (82) | 30 (18) | < 0.001* |
| Female | 59 (53.6) | 51 (46.4) | |
| Age | |||
| < 50 years | 181 (67.4) | 50 (21.6) | < 0.001* |
| > 50 years | 15 (32.6) | 31 (78.4) | |
| Joint alignment parameters [mean ±SD] | |||
| TTTG | 7.53 ±3.22 | 8.53 ±3.24 | 0.02 |
| SA | 128.24 ±7.92 | 129.63 ±8.77 | 0.2 |
| SD | 7.76 ±1.3 | 7.11 ±1.49 | < 0.001† |
| LPFA | 17.02 ±6.17 | 17.32 ±6.75 | 0.721 |
| LPD | –3.25 ±2.71 | –2.34 ±3.56 | 0.04 |
| Insall-Salvati index | 1.12 ±0.16 | 1.38 ±1.54 | 0.13 |
Participants were divided into two groups based on age, under 50 years old and over 50 years old, and their cartilage damage grade was assessed. Table III shows a comparison of patellofemoral joint alignment parameters between healthy individuals and OA patients.
Table III
Patellofemoral joint alignment parameters comparison in two age groups between healthy individuals and osteoarthritis
| Age group | Variables | Healthy group | Osteoarthritis group | p-value† | |
|---|---|---|---|---|---|
| > 50 years | Joint alignment parameters [mean ±SD] | TTTG | 7.6 ±3.27 | 8.42 ±2.83 | 0.10 |
| SA | 128.19 ±8.02 | 131.28 ±8.74 | 0.019 | ||
| SD | 7.75 ±1.31 | 6.93 ±1.61 | > 0.001 | ||
| LPFA | 17.03 ±5.91 | 16.64 ±7.33 | 0.69 | ||
| LPD | –3.26 ±2.75 | –2.13 ±3.87 | 0.02 | ||
| Insall-Salvati index | 1.12 ±0.17 | 1.23 ±0.22 | > 0.001 | ||
| < 50 years | Joint alignment parameters [mean ±SD] | TTTG | 6.78 ±2.63 | 8.72 ±3.85 | 0.08 |
| SA | 128.93 ±6.81 | 126.98 ±8.28 | 0.43 | ||
| SD | 7.87 ±1.20 | 7.39 ±1.25 | 0.23 | ||
| LPFA | 16.93 ±8.94 | 18.41 ±5.62 | 0.49 | ||
| LPD | –3.2 ±2.21 | –2.67 ±3.10 | 0.56 | ||
| Insall-Salvati index | 1.14 ±0.11 | 1.62 ±2.48 | 0.46 |
The results showed that the values of Insall-Salvati index, LPD, SD and SA in the under-50 group have a significant relationship with OA (p-value < 0.05). No significant association was observed between the values of joint measurements despite OA in the over-50 group.
Spearman’s rank correlation coefficient (rho) test was performed to investigate the relationship between increased cartilage damage grade and joint alignment parameters, bone marrow edema, and osteophyte. In Table IV the results show a negative correlation between SD values and the grade of articular cartilage damage (rho = –0.21) and a positive correlation with Insall-Salvati index values (rho = 0.21) among patients under 50 years old.
Table IV
Correlation between patellofemoral joint alignment parameters, bone marrow edema, and osteophyte with increasing grade of joint injury in both age groups
This means that the degree of joint cartilage damage has increased with decreasing SD values and increasing Insall-Salvati index values. No such association was observed in patients over 50 years old. This test also showed that higher osteophyte and bone marrow edema rates are associated with higher grade of articular cartilage in both age groups (rho = 0.4, rho = 0.56 in the under-50 group, rho = 0.62, rho = 0.64 in the over-50 group, respectively).
Discussion
Asymmetry in the patellofemoral joint has been suggested as a factor in the development and progression of patellofemoral OA in various sources [19, 20]. Limited studies have examined the relationship between multiple parameters related to joint alignment and cartilage damage and have reported conflicting results. This study aimed to investigate the relationship between patellofemoral alignment and OA.
In presented study among 277 studied patients men predominated (67.3% male and 39.7% female). The mean age of all participants was 36.8 ±13.3. This study showed that the prevalence of patellofemoral OA in patients was 28.9%, which was higher than that in similar studies [21–23]. In our study, similar to international reports, the prevalence of patellofemoral OA was significantly higher among women and people over 50 years old. It indicates that age and gender are crucial risk factors for patellofemoral OA.
Examination of SA, SD, LPD, and Insall-Salvati index values in participants under 50 years old showed that LPD, SA, and Insall-Salvati index values in OA patients were higher than in the control group, and the SD value was lower. With these results, patellofemoral joint misalignment can be used as a risk factor for OA in people under 50 years old, while other risk factors are considered in people over 50 years old.
The study by Tsavalas et al. [21] included 655 patients in two age groups (over 50 years and under 50 years). In this study, a significant relationship was observed between LPFA, SA LPD, and SD levels and OA in both age groups. However, unlike the present study, no significant relationship was observed between the Insall-Salvati index and OA in people under 50 years old.
In another study, conducted by Kalichman et al. [22], 213 patients with a mean age of 60 years were evaluated. In this study, a significant relationship was observed between the levels of SA and LPFA, Insall-Salvati index, and OA.
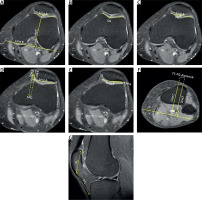
Femoral sulcus depth and SA are two crucial factors in trochlear morphology that are used to evaluate trochlear dysplasia [24]. Increase in SA and decrease in SD indicate a shallow trochlear groove (Fig. 2A, B, respectively).
Fig. 2
Magnetic resonance imaging of patients with tibial tubercle-trochlear groove, and femoral sulcus angle values increased, and femoral sulcus depth value decreased. Flat trochlear groove (sulcus depth: 0 mm) (A), increased sulcus angle (B), increased tibial tubercle-trochlear groove distance (C).
In our study, these parameters showed a significant relationship with OA in people under 50 years old. A study conducted by Ali et al. [23] showed that trochlear parameters in the under-40 group were significantly associated with articular cartilage damage. This study did not find a significant relationship between patellofemoral alignment parameters and articular cartilage damage. This contradiction could be due to differences in sample size in the Ali et al. [23] study and the present study (100 and 277 patients were examined, respectively).
Lateral patellofemoral angle and LPD are two characteristics of congruence between the patellar and the femur. In this study, further LPD, which suggests a more lateral position of the patellar triceps, showed a significant association with joint cartilage damage. No such association was observed with LPFA.
The position of the tibial tubercle is also an important parameter of the patellofemoral joint alignments because it determines the axis of inferolateral pressure applied to the joint that is measured by the TTTG parameter. Values less than 15 mm are normal, and values higher than 20 mm are abnormal. In our study, increase of TTTG showed a significant relationship with increased incidence of OA in all patients. (Fig. 2C).
In addition to examining the relationship between joint alignment parameters despite OA, the correlation between the parameters and the joint damage severity was also investigated. The results showed that in the OA patients under 50 years old, increasing the Insall-Salvati index and decreasing SD increase the severity of joint cartilage damage.
The present study’s findings and similar studies indicate that there are some other risk factors in addition to the morphology and orientation of the patellofemoral joint in older people that predispose them to joint cartilage damage.
Study limitations
This study also had some limitations. The most important limitation of our study was our selection. The population of our study was from patients who underwent MRI due to knee problems, and therefore it cannot be a sample of the normal population, and the results cannot be generalized with certainty to the society.
Also, the relationship between measured parameters and patients’ clinical symptoms were not evaluated due to the inaccessibility to patients to get an accurate history.
Future studies with larger samples and random selection can help investigate the prevalence of cartilage damage in the general population.
Conclusion
Patellofemoral joint asymmetry in the younger people was significantly associated with joint cartilage damage and premature patellofemoral joint OA. Joint misalignment by stressing the articular cartilage causes joint cartilage changes that may be congenital or due to bone injuries such as trauma and surgery.