Introduction
Clinical interest in low back pain (LBP), accompanied or not with pain radiating down the sciatic nerve, is due to the fact that these are among the most common symptoms or peripheral nervous system diseases [1–3]. More than 4% of patients who seek medical advice for any reasons have LBP. Half of the admissions in neurological departments are for lumbar-sciatic syndrome [1, 3].
The condition has social significance since 80% of working people have faced it at least once in their working lifetime. Most of the acute and subacute (> 6 weeks) episodes resolve within 3 months while in 10–15% of patients their condition does not resolve and they develop chronic (> 3 months) lumbosacral syndrome (LSS) [1, 4].
Analysis of the literature reveals multiple approaches to conservative treatment of discogenic lumbosacral radiculopathy (DLSR). At the same time, there is a lack of data on their short- and long-term effectiveness.
Usually, diagnosis is easy to determine. Functional tests showing characteristic vertebral and radicular syndromes are additional to anamnestic data [2, 3, 5]. In cases of non-typical course of the disease, which is very common when lesions have higher localization, data from the clinical study are not sufficient. Additional imaging studies are needed (computed tomography, nuclear magnetic resonance, electromyography). Imaging of specific anatomic changes solves the issue of differential diagnosis.
Regarding the therapeutic approach in patients with DLSR, in our everyday clinical practice we face the question what is the best approach for that particular case. Several key factors determine the choice of methods to use and the mechanism of impact: stage of disease, process localization, and patient’s general condition [6].
The therapy aims to fight against the pain syndrome, to decrease compression and inflammatory phenomena, to normalize trophicity and metabolism, to improve circulation and vitamin balance [2, 7]. Methods of physical medicine are preferred not only as a single therapeutic strategy, but also as a part of complex treatment of these patients.
Physiotherapeutic complexes used here [8] are capable of causing physical analgesia by several mechanisms: by affecting the cause of nociceptors’ stimulation; by blocking nociception; by interrupting neurotransmission (along A-δ and C-fibers) towards the body of the first neuron of general sensitivity; by turning the gate control on.
Recently, the interest of community and health care specialists in using alternative non-pharmaceutical methods for affecting pain in DLSR has been growing [9, 10]. Acupuncture is one of these alternatives.
There are two leading theories that attempt to explain the mechanisms of action [11]. Release of endogenous opioids is one of the leading theories explaining the mechanism of action of acupuncture and is called “neurohormonal theory”.
The second theory that became popular in the scientific community is based on the continuous inhibitory action of acupuncture. In cases of continuous inhibition of the central nervous system through long-lasting low frequency stimulation, a decrease in the number of nerve impulses (decrease of synaptic transmission) is achieved for a long period of time [10, 12].
The aim of the present research is to optimize the therapeutic approach in patients with chronic pain due to discogenic lumbosacral radiculitis by comparing the therapeutic effect of combination application of different physical and alternative factors of treatment.
The subject of this research is to compare the effect of acupuncture implementation in the low back area and the affected limb versus ultrasound (US) and low frequency impulse magnetic field (LFIMF) implementation in the low back area and the affected limb in chronic pain caused by discogenic lumbosacral radiculitis.
Material and methods
Background data were obtained for the two compared groups consisting of patients of predominantly working age, with continuous, chronic intermittent disease course, who had received inpatient or outpatient conservative treatment through different methods but without significant improvement of clinical complaints.
The research enrolled 30 patients with chronic pain due to discogenic LS radiculitis who received a combination of: LFIMF in the low back area and the affected leg; paravertebral US in the lumbosacral spine segment with Oxypain Oil (the main active ingredient is oxidized glycerol triesters of natural essential oils. The product is a medical device.) mediator with power of 0.4–0.6 W/cm2, 10 min. The treatment course comprised 10 LFIMF procedures and 10 US procedures with follow-up of the effect before and during the treatment and a month later.
The second group included 30 patients who received within 2 weeks (without the weekends): classic acupuncture in the low back area and the affected leg including biologically active points (BAP), predominantly on the meridian of the urinary bladder (UB), the gallbladder (GB) and governing vessel meridian (GV), 12 points per session using the sedating method (deep placement of needles with several rotations during the 20-minute procedure).
We used original Chinese stainless steel needles, individual for each patient with the following parameters: ϕ 30, longitude 40 mm. We made an objective evaluation of the results at the beginning and during the treatment, and also a month later.
Statistical analysis
Data were analyzed using SPSS v.20 (IBM SPSS, Armonk, NY). Categorical data were compared with the χ² test or Fisher’s exact test (as appropriate). Continuous variables were compared with the independent samples t-test in normal distribution or the Mann-Whitney U test for distribution different from the normal, and with the paired samples t-test or Wilcoxon signed ranks Z test, respectively. All statistical analyses were performed at α = 0.05.
Bioethical standards
The study protocol of this single-center retrospective observational study was reviewed and approved by the Ethics Committee at the University Hospital Tsaritsa Yoanna-ISUL, Sofia (21.01.2022). Owing to the retro-spective nature of this study and the anonymization of data, the need for informed consent was waived. All studied patients gave signed informed consent in order to begin in-hospital treatment. The study was performed according to the Declaration of Helsinki principles and the EU General Data Protection Regulation.
Objective evaluation
For objective evaluation of the patient’s condition, we used a Visual Analogue Scale (VAS) for assessment of pain (VAS from 0 to 100 mm), volume of movement in the lumbar spine segment with centimeter measurement (test of Tom Meyer, left and right lateral flexion, extension and test of Schober) and we studied muscular weakness of flexors and extensors of the torso with the manual muscle test (MMT) [13].
Results
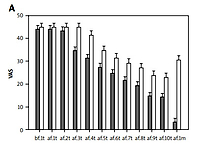
Comparing results in group I (LFIMF and US) and group II (acupuncture in BAP), Figure 1 shows that pain strength in group I started to decrease statistically significantly after the third procedure while in group II it did so after the sixth one. This positive tendency was maintained until the end of the treatment course and also a month later. A statistically significant difference between the two groups (p < 0.001) was observed in favor of group I.
Results from Tom Meyer’s test show that flexion in the thoracic-lumbar spine segment in group I started to increase statistically significantly after the fifth procedure while in group II it did so after the eighth one (Fig. 1).
This positive tendency in both groups was maintained until the end of the treatment course. In group I this tendency was also maintained 1 month after the end of the therapy while in group II values do not show a statistically significant difference from the background data. Improvement in group I is statistically significant when compared to group II (p = 0.0424)
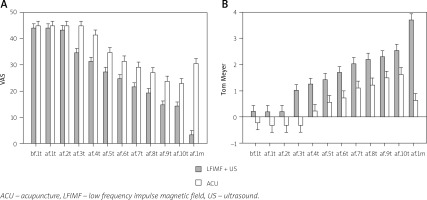
In right lateral flexion we observed a statistically significant difference in group I from the fifth procedure until the end of treatment and also a month after its end. In group II this happened from the eighth procedure until the end of treatment but a month after the end of therapy the values were close to the background data. A statistically significant difference in improvement between the two groups (p < 0.001) was observed.
The graph in Figure 2 shows that left lateral flexion improved statistically significantly in group I after the fifth procedure, unlike group II in which this happened after the ninth one. This positive tendency was maintained until the end of therapy but 1 month after its end in group II a negative tendency was observed when compared to group I. A statistically significant difference in improvement between the two groups (p = 0.00582) was observed.
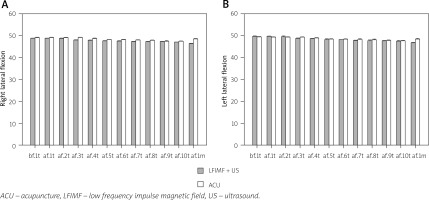
Regarding the extension in the lumbar spine segment, the graph in Figure 3 shows that in group I extension increased statistically significantly after the sixth procedure while in group II it did so after the seventh one.
This positive result was maintained until the end of the treatment course in both groups but 1 month after the end of therapy, again, there was no statistical significance in the results of group II, unlike group I. A statistically significant difference in improvement between the two groups (p < 0.001) was observed.
The second graph in Figure 3 shows the difference between the two groups, evaluated objectively by the test of Schober. A statistically significant difference in improvement between the two groups (p < 0.001) was observed. In group II flexibility improved with a statistically significant difference after the eighth procedure while in group I it did so 1 month after the treatment. One month after the end of treatment, group II did not show any statistically significant difference compared to the background data.
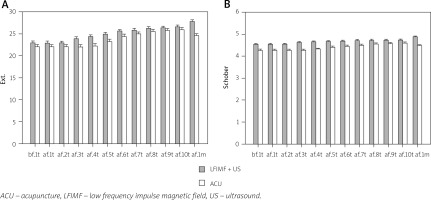
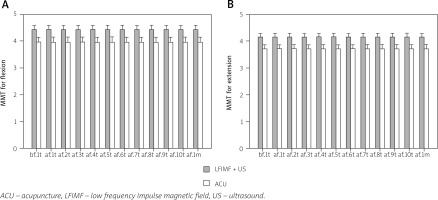
There was a statistically significant difference between the two groups in terms of MMT flexion of torso and MMT extension of torso (p < 0.001 for MMT flexion and p < 0.001 for MMT extension), but this difference could be observed even in the background values of both groups. At the end of the treatment course values showed no statistically significant difference compared to the background level. Data are presented in Figure 4.
In the two studied groups – group I (LFIMF in the low back area and the affected leg in combination with paravertebral US through a labile method with Oxypain Oil mediator) and group II (acupuncture in BAP, predominantly from the GV, UB, GB meridians) – we found faster change in pain magnitude assessed by VAS (100 mm) in group I than in group II, and this tendency was maintained after the end of the treatment course and also a month later. We attributed this tendency to the fact that patients in both groups were selected in a later stage of the disease (after more than 3 months from the first clinical symptoms).
Discussion
In cases of pain chronification, the predetermined factors US and LFIMF affect the damaged structures more due to some of their characteristic features – the thixotropic effect (turning a gel into a sol under the influence of US mechanical waves, which leads to enrichment of the damaged nucleus pulposus of the intervertebral discs with mucopolysaccharides), and also to improvement of blood circulation in the affected tissues, directly and through formation of collateral vessels under the influence of LFIMF [6].
Analgesia with acupuncture is achieved mainly by endogenous opioid release, and also by long-term inhibition of central nervous system via continuous stimulation of descendant inhibition that leads to a decrease in the number of nerve impulses (decrease of synaptic transmission) for pain for a long period of time [10, 11, 14], which makes acupuncture rather effective in fighting against acute and subacute pain.
Regarding the improvement of the functional capability in the lumbosacral spine segment, results are again more in favor of patients in group I than group II as with structural (morphological) recovery comes functional improvement.
Regarding the test of Tom Meyer, the test of Schober, results from follow-up of left and right lateral flexion, extension in the lumbar spine segment, MMT for flexion and extension of the torso, all methods for objective evaluation of flexibility in the lumbosacral spine segment, even in the middle of the treatment course (around the fifth procedure), showed improvement in patients of group I compared to group II, and this tendency was also maintained after the end of the treatment course and also a month later.
Among the factors of alternative medicine, acupuncture could be used in fighting against pain, especially in patients contraindicated for predetermined factors (those with a pacemaker, or an oncological process in the small pelvis area) [12, 15, 16].
Conclusions
According to the aforementioned data we could reach several conclusions. In cases of chronic pain (more than 3 months) in this particular disease, a recommendation should be given to the combination of two physical factors – paravertebral application of US in impulse mode with an appropriate anti-inflammatory medicament as a mediator in the area of the lumbosacral spine segment, by a labile method, combined with LFIMF in the low back area and the affected leg.
Follow-up of the short- and long-term effect of predetermined physical factors remains a challenge for specialists dealing with DLSR treatment. The lack of convincing evidence in the scientific literature confirms this statement.
Usage of a therapeutic scheme comprising predetermined and alternative treatments is completely safe and cost-effective, except for a small patient population, mainly those with pacemakers, pregnant women, patients with severe cardiovascular diseases, and those with malignant diseases.
Due to the positive results we obtained and verified statistically with our patients – in the short term and a month after finishing the treatment – we decided to offer the combination of US and LFIMF, and also acupuncture application for treatment of DLSR regardless of the patient’s age and duration of complaints.