Introduction
The treatment with glucocorticosteroids (GCs) was discovered 74 years ago and since then it has played a significant role in the management of many immune-mediated rheumatic diseases (IRDs) [1]. Despite the development of new treatment modalities with disease-modifying anti-rheumatic drugs (DMARDs), GCs are still the most frequently employed class of anti-inflammatory drugs [2].
Their effectiveness is based on different mechanisms, including classic genomic mechanisms leading to changes in gene expression, non-genomic mechanisms mediated via the cytosolic GC receptor and via non-specific interactions with membranes of cells and organelles [3].
Despite being anti-inflammatory and immunosuppressive drugs, their use is restrained by the fear of the occurrence of adverse effects (AEs). The therapeutic effects of GCs range from pain relief and disease-modifying effects in arthritides, such as rheumatoid arthritis (RA), to strong immunosuppressive actions in systemic autoimmune diseases such as systemic lupus erythematosus (SLE) or vasculitides [2, 4, 5].
Glucocorticosteroids are prescribed in different patterns, and their usage depends on the diagnosis, indications and goal of treatment. They remain the anchor drugs for therapeutic strategies in idiopathic inflammatory myopathies (IIMs), polymyalgia rheumatica (PMR), giant cell arteritis (GCA), systemic vasculitides and SLE.
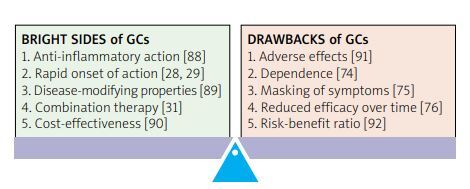
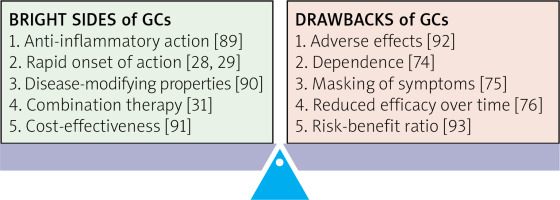
While their benefits are undeniable, their side effects should be taken into account especially considering the chronic prescription in inflammatory rheumatic diseases [6] (Fig. 1).
Fig. 1
The balance between benefits and drawbacks of glucocorticosteroid treatment in immune-inflammatory rheumatic diseases.
This viewpoint analyses the benefits and drawbacks of GC treatment in IRDs by discussing recent randomized controlled trials (RCTs), observational, translational studies and systematic reviews, also providing an in-depth perspective of the experience in the current clinical practice of our center.
The bright side of glucocorticosteroid treatment in immune-inflammatory rheumatic diseases
Glucocorticosteroids have become a cornerstone in many different rheumatological diseases because of their swift onset of action and a quick relief of symptoms in acute flares, being able to prevent irreversible organ damage [7, 8]. Indeed, they remain essential in managing life-threatening autoimmune diseases, such as antineutrophil cytoplasmic antibody (ANCA)-associated vasculitides, systemic autoimmune connective tissue diseases such as SLE, or IIMs, where they are used to control organ-threatening disease manifestations [9 , 10].
For instance, in SLE, high-dose or “pulsed” GCs are essential in cases of nephritis, vasculitis, neuropsychiatric involvement, myocarditis, or alveolitis, among others. In these cases, intravenous corticosteroids should be preferred to oral GCs whenever possible [10]. A recent meta-analysis also showed that SLE patients with specific baseline predictors such as younger age and serologically active although clinically quiescent disease were at risk of relapsing after discontinuing GC treatment [11].
In polymyalgia rheumatic (PMR), GC therapy with a slow taper is considered the core of treatment for the first 1–2 years of diagnosis [12]. The 2015 EULAR/ACR recommendations highlight that there is no ideal GC regimen suitable for all PMR patients, so the GC dosing and tapering schedule should be individualized based on patient characteristics such as disease severity, comorbidities, other prescribed medications, risk of GC-related AEs, and patient preference [12]. Previous translational studies conducted in our center also suggest that phenomena of immune and endocrine senescence occur in PMR patients; in particular, a dysfunctional hypothalamic–pituitary–adrenal (HPA) axis has been detected with impaired production of cortisol and dehydroepiandrosterone sulfate (DHEAS) [13–15].
Analogously, initial high dosages of GC treatment (40–60 mg/day prednisone equivalent) are recommended for patients with a high clinical suspicion of GCA, despite an unconfirmed diagnosis with imaging techniques, due to the imminent risk of visual loss [16, 17]. Although much progress has been made in introducing steroid-sparing agents such as tocilizumab (TCZ) [18], recent evidence from the GCA treatment with ultra-short GC and TCZ trial (GUSTO) suggests that GC treatment is still essential and cannot be stopped very early during the disease course due to the high frequency of relapses within the first month, detected in 75% of patients [19].
Glucocorticosteroids have also been shown to improve overall quality of life, including pain, function, and psychological well-being in RA patients, playing a significant role, especially during disease flares [3].
Data from previous studies conducted in our center suggest that the chronic inflammatory stimulus exerted by RA induces a persistent activation of the HPA axis, with a progressive insufficient production of endogenous corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and finally cortisol [20]. In this way, GCs, when externally supplemented, can act as a “replacement therapy” to restore cortisol levels in the serum to an adequate amount [21].
Different RCTs and meta-analyses have demonstrated that GC therapy, particularly when administered on a long-term, low-dose basis, can slow the progression of radiographic damage in patients with early RA by at least 50%, satisfying the conventional definition of a DMARD [22–24].
Additionally, a task force from the European Alliance of Associations for Rheumatology (EULAR) was established with the aim of defining conditions under which long-term GC treatment is safe enough to enable the implementation of existing recommendations for treating RA. The task force recognized the importance of using low doses of GCs and ultimately agreed that, for the majority of patients, the risk of harm is low when taking long-term dosages of ≤ 5 mg/day prednisone (PDN) equivalent. Patient-specific characteristics, such as protective and risk factors, can influence the risk of harm at dosages between > 5 and ≤ 10 mg. However, at dosages of > 10 mg, the risk of harm is elevated [25] (Table I).
Table I
Patient-specific factors influencing the grade of damage induced by chronic GC treatment. In the column labelled in green, there are reported factors, analysed in observational studies, which are protective if GC dosages are ≤ 5 mg/day prednisone equivalent. In the third column, there are listed factors which might increase the level of harm if GC dosages are > 10 mg/day prednisone equivalent. Between dosages ranging from 5 to 10 mg/day, there is a more uncertainty and a careful multidimensional assessment needs to be performed balancing the risk to benefit ratio. Besides the daily dosages, the cumulative exposure and duration of treatment should be taken into account. As per consensus, long-term GC usage refers to an assumption period > 3–6 months [25]
| Reduced grade of damage | GC-related adverse events | Increased grade of damage |
|---|---|---|
| Male sex, absence of prior fragility fractures, normal baseline BMD, young age at the start of GC treatment*, physical activity, sufficient intake of vitamin D and calcium, prescription as per guidelines of antiresorptive/osteoanabolic treatment [94] | Osteoporosis | Older age at the start of GC therapy, low baseline BMD, previous fragility fractures, female gender, low BMI, smoking, excessive alcohol intake [94] |
| Younger age, absence of comorbidities (i.e. diabetes, chronic kidney failure, chronic obstructive or interstitial lung disease), vaccinations [49, 51] | Infections | Elderly age, chronic comorbidities (see left column), poor overall general conditions evaluated with standardised scales (i.e. Karnofsky score), concurrent treatment with DMARDs [49, 51] |
| Absence of prior history of glucose intolerance or diabetes, younger age, normal BMI, healthy diet and exercise [95] | Diabetes mellitus | Previous history of glucose intolerance or diabetes, older age, overweight or obesity status, familial history of diabetes, physical inactivity, specific ethnic background (African American, Hispanic Latino, Native American, Asian) [95] |
| Healthy diet, exercise, absence of prior history of cardiovascular disease or diabetes, younger age, normal blood pressure and lipid serum concentrations [96] | Cardiovascular events/effects | Smoking, physical inactivity, systemic arterial hypertension, obesity, atherosclerosis, coronary heart disease, previous history of myocardial infarction and/or heart failure [96] |
| Absent history of previous neuropsychiatric disorders, traumatic brain injuries, substance abuse or addiction [97] | Neuropsychiatric involvement | Concurrent medications affecting the central nervous system (opioids, benzodiazepines or antipsychotics), presence of the risk factors mentioned in the left column [97] |
| Absence of prior history of cataracts or glaucoma, younger age [98] | Cataract and glaucoma | Presence of prior history of cataracts or glaucoma, older age, family history of cataract/glaucoma, smoking, systemic arterial hypertension, diabetes [98] |
| Absence of prior history of ulcers, gastrointestinal bleeding, Helicobacter pylori infection, comorbidities (diabetes, heart failure)Prophylaxis with PPI [99] | Ulcers/gastrointestinal bleeding | Concomitant use of NSAIDs, antiaggregant and/or anticoagulant treatment. Previous history of ulcers, Helicobacter pylori infection, comorbidities (diabetes, heart failure) [99] |
Reassuring data related to the efficacy and safety of GC also emerged from the recently published Glucocorticoid LOw-dose in RheumatoId Arthritis (GLORIA) trial, which suggested that the add-on low-dose prednisolone might display beneficial long-term effects in elderly patients with established RA [26]. A low rate of non-severe AEs was observed, potentially indicating a favorable balance of benefit and harm.
Also the Steroid EliMination In RA (SEMIRA) trial discovered that continuing to use 5 mg of daily PDN in patients who were receiving TCZ and csDMARD and had achieved remission or low disease activity resulted in better disease control than tapering the GCs [29]. The continuation group had a treatment success rate of 77%, compared to 65% in the taper group (p = 0.02). Furthermore, although the overall safety profile was comparable and there were no reported cases of clinically evident adrenal insufficiency or fatalities, the tapered GC group encountered a greater number of treatment-emergent adverse events compared to the group continuing GCs [27].
To summarize the beneficial aspects of GC treatment, we can conclude that these molecules have a rapid onset of action, providing relief of pain, stiffness, and swelling within hours to days of administration [28, 29]. They are used as first-line therapy in many IRDs to rapidly control local or systemic inflammation and are relatively inexpensive compared to biologic DMARDs, making them a cost-effective treatment option for many conditions [3, 30].
Low-dose GCs have been shown to have disease-modifying properties in RA, reducing joint damage and reducing radiographic progression [22, 23]. They can be used in combination with other DMARDs to improve the therapeutic response and prevent disease flares. They can also be used as a bridge therapy while waiting for other steroid-sparing agents to take effect [31, 32].
Despite the advances in biological and targeted treatments available for other IRDs, evidence from RCTs and from meta-analyses of observational studies suggest that the early discontinuation of GC is not yet feasible for most of the patients.
Chronobiology of glucocorticosteroids in rheumatoid arthritis
Recent significant advances in the optimization and long-term management of RA with GCs have also emerged from the validation of their administration in accordance with the physiological circadian rhythm, as initially proposed by Cutolo et al. [33]. Serum cortisol, a key GC hormone, follows a circadian rhythm, with peak levels in the morning and trough levels at midnight. This diurnal variation in cortisol levels appears to be influenced by the nocturnal rise of pro-inflammatory cytokines such as tumor necrosis factor (TNF) and interleukin-6 (IL-6), which stimulate cortisol production around 3 am. However, in chronic inflammatory conditions such as RA, the nocturnal cortisol production is often insufficient, leading to a diminished anti-inflammatory effect during the night and subsequent morning symptoms [21].
In light of these findings, it has been optimized to administer exogenous replacement doses of GCs around 3–4 am, rather than at breakfast as traditionally done around 7–9 am, to better align with the circadian rhythms of the nocturnal inflammatory response and the physiological anti-inflammatory actions of endogenous GCs [34]. This has been made possible by the availability of a modified-release PDN formulation, which is designed to release PDN in the stomach/gut at 3 am, mimicking the natural cortisol production rhythm and its anti-inflammatory effects against pro-inflammatory cytokines [34].
Two RCTs have demonstrated the efficacy of this modified-release (MR) PDN formulation in managing the signs and symptoms of RA, particularly morning stiffness (MS), achieving superior rates of MS improvement after 3 months compared to immediate-release (IR) PDN taken in the morning (33% reduction in the MR group vs. 0% in the IR arm) [35, 36]. This formulation has also shown promising results in managing PMR and may be a potential option for better controlling the inflammatory process also in newly diagnosed patients with GCA [37, 38]. Although specific recommendations on the use of MR cortisone have not been formulated, it has been suggested that their utilization might be considered in patients experiencing prolonged fatigue and joint stiffness in the morning [20, 39]. Notably, in recognition of recent discoveries on the molecular mechanisms governing cellular circadian rhythms, the 2017 Nobel Prize in Physiology or Medicine was jointly awarded to three scientists [40].
The drawbacks of glucocorticosteroids in treating inflammatory rheumatic diseases
Despite their benefits, GCs have many AEs that can limit their use, particularly when used in high dosages and for prolonged periods. The results of a recent survey identified that patients receiving GC therapy for rheumatic diseases experience a large number of AEs, strongly impairing the quality of life, and what is perceived by patients is often difficult for the physicians to measure [41]. An unmet need is, therefore, the development of patient-reported outcome measures to capture the effects of GCs from the patient’s perspective.
Among the main long-term GC-related AEs, it is worth analyzing recent published data related to metabolic disturbances (diabetes, dyslipidemia, hypertension and weight gain), infectious risk, ocular-related AEs (cataract and glaucoma) and bone loss, which can lead to osteoporosis and fragility fractures [42].
Large observational registries collecting data of patients with IRDs suggest that greater cumulative GC dosages (estimated cut-off > 1,800 mg of PDN equivalent), achieved by the exposure from low to medium dosages of GC, are associated with higher AE-related healthcare expenditures [43]. The incremental costs were observed for osteoporotic fractures, type 2 diabetes mellitus, gastrointestinal bleeding and hospitalizations related to opportunistic infections and myocardial infarctions/strokes [43].
In a national German registry where long-term GC usage was assessed in patients with PMR and GCA, only osteoporosis prevalence increased within 3 years whereas the prevalence of cardiovascular comorbidities and diabetes did not significantly rise [44].
Some identified risk factors for GC-induced osteoporosis (GIOP) and fragility fractures include age > 55 years, female sex, Caucasian ethnicity, and long-term use of PDN at a dose ≥ 7.5 mg per day [42]. Since GIOP shows increased morbidity and mortality, clinicians should assess bone health for every patient receiving GC treatment for more than 3 months since one can rely on several effective medications for treating and preventing this condition. These include antiresorptive drugs such as bisphosphonates or denosumab, bone anabolic drugs (i.e. teriparatide) or agents with a mixed dual action, anti-resorptive and anabolic, such as romosozumab, data for which in relation to GIOP were recently presented at the American College of Rheumatology (ACR) 2022 annual meeting [45, 46].
Due to the immunosuppressive side effects, GCs can logically increase the risk of infections, impair wound healing and induce the development of ocular-related disorders such as cataracts and glaucoma [47]. Different studies have reported an increased risk of infection in patients with IRDs compared to the general population. The most frequently reported sites of infections are the skin, the musculoskeletal system, and the respiratory and urinary tracts [48]. In a large multicenter study including a wide spectrum of IRD patients, the incidence of serious infections was 114.8 per 1,000 person-years [49]. Interestingly, the independent risk factors for these outcomes were elderly age, the presence of interstitial lung disease, a high dose of GC (≥ 29.9 mg/daily) and poor overall health quantified with the Karnofsky score [49].
The risk of infections has been reported to be increased even with dosages < 5 mg of PDN equivalent daily in another large observational study of approximately 40,000 patients with PMR and GCA. The estimated cumulative probability of all types of infection was 18% in the first year of treatment [50]. However, the association between low-dose GCs and increased risk of infections still remains unclear in terms of strength of evidence, since data from RCTs of short-term and lower doses of steroids have generally shown little or no increased risk. Additionally, real-world data have shown, an increased risk which is dose-dependent for serious opportunistic infections (e.g. herpes zoster, tuberculosis and Pneumocystis jiroveci) [51].
The use of GCs has also been associated with an increased risk of cardiovascular disease and mortality, particularly in RA patients with pre-existing cardiovascular risk factors [52]. Another population-based cohort study assessing 6 different IRDs (PMR, GCA, inflammatory bowel diseases, RA, SLE and vasculitides) detected an increased risk of cardiovascular events even with GC dosages < 5 mg daily. This highlights how prompt and regular the monitoring of the cardiovascular risk should be with a necessary primary prevention treatment at all GC doses through accurate patient risk stratification [53].
Although neuropsychiatric complications have been reported in up to 6% of patients receiving GC treatment, the evidence that these phenomena occur with low dosages is scarce, and they are mostly associated with high or pulse dosages [54]. Analogous considerations can be made for GC-induced diabetes mellitus, whose development has been more closely associated with high dosages and specific personal risk factors (BMI > 25, HbA1c > 6%, smoking, familiar history of diabetes mellitus and other co-existing cardiovascular risk factors) [55]. Conversely, a recent systematic review highlighted the difficulty in quantifying the risk of cataract and glaucoma in a population of RA patients since these safety outcomes have not been well captured and reported in RCTs and well-designed observational studies [56].
Bearing in mind these multiple potential side effects, it is understandable that rheumatological patients with higher disease activity are more likely to experience overall organ damage, not only due to the disease itself but also due to the GC treatment, since they are exposed to higher dosages for a prolonged time.
A classic but well-designed observational study reported that chronic GC treatment was also associated with irreversible organ damage in a substantial proportion of SLE patients measured through the increase of the Systemic Lupus International Collaborating Clinics (SLICC)/ACR damage index [57]. In up to 80% of cases, organ damage after diagnosis is directly or indirectly attributable to PDN. More specifically, medium dosages (10 to 20 mg daily) have been shown to increase the risk of cardiovascular events in SLE patients and any dose above 6 mg increases later organ damage by 50% [58, 59].
Systemic lupus erythematosus can also cause a spectrum of complications during pregnancy, not only for the mother but also for the fetus. It can affect fertility and cause certain complications during pregnancy such as preterm labor and delivery, high blood pressure (pre-eclampsia), placental insufficiency, miscarriage or stillbirth. Furthermore, it can cause mortality, preterm birth, and neonatal lupus (a temporary condition in the baby caused by SLE-related antibodies) and structural abnormalities in the fetus [60].
On the same note, elevated disease activity in RA during pregnancy increases the risk of adverse pregnancy outcomes such as gestational hypertension, premature rupture of membranes, antepartum hemorrhage, preterm delivery, intrauterine growth restriction, and Caesarean section [61].
Glucocorticosteroids are one of the medications commonly used in pregnancy to control IRD disease activity, given that a large number of classical and biologic DMARDs cannot be used due to their teratogenicity and ability to cross the placenta. It was demonstrated in some studies that long-term GC use during pregnancy can be associated with an increased risk of gestational hypertension, pre-eclampsia, and gestational diabetes [61, 62]. The use of PDN during pregnancy has been found to increase the risk of premature delivery and, consequently, lower birth weight in pregnant women with RA. However, disease activity can negatively influence birth weight independently, likely through immune-mediated mechanisms [63].
Additionally, in conditions such as congenital heart block (CHB), associated with SSA/Ro autoantibodies, the use of fluorinated steroids (FS) was proved to have a mostly positive effect on fetal survival even with possible CHB regression [64].
Therefore, control of disease activity with appropriate medications such as GCs is important during pregnancy, especially when the benefits largely outweigh the possible risks [65].
The same can be said about renal disease in IRDs. Renal disease develops early in SLE, with up to two-thirds of patients with SLE developing lupus nephritis (LN) within 5 years of SLE onset. The use of GCs is one of the most important contributing factors to organ damage in SLE [66].
As mentioned above, prolonged GC use is associated with myriad AEs; thus the achievement of a daily prednisone dose of ≤ 5 mg/day is in fact a criterion for SLE remission [67]. Moreover, recent RCTs in LN as well as international guidelines have proposed a lower dose of glucocorticoids as induction therapy and in particular, a regimen of intravenous pulse methylprednisolone followed by oral prednisone with rapid tapering in the case of disease activity flare or even rapidly progressive LN, as the most effective way of achieving once again the remission stage [68–70]. The same GC therapy principle applies for other IRDs with acute or chronic kidney injury such as ANCA-associated vasculitides [71].
In this perspective, EULAR guidelines for the treatment of chronic IRDs such as SLE, RA and GCA recommend the tapering and the withdrawal of GC treatment when sustained remission is achieved [16, 72, 73].
In brief, while GCs have many positive effects in the treatment of IRDs, the negative consequences associated with their use must not be overlooked. The long-term use of GCs is associated with numerous side effects, including dependence, masking of symptoms, reduced efficacy over time, and a higher risk of AEs [74–76]. The risk-benefit ratio of GCs must be carefully considered in the treatment of IRDs, and the problem of the proper use of GCs remains a significant challenge in clinical practice.
The optimized use of glucocorticosteroids in rheumatology: treat-to-target strategies, outcome measures for assessing glucocorticosteroid toxicity and development of selective glucocorticosteroid receptor ligands
The proper use of GCs in rheumatological practice is essential to balance their benefits and risks. Several strategies have been proposed to optimize their use, such as using the lowest effective dose, limiting the duration of treatment, and using combination therapy or alternative treatments, such as DMARDs, when appropriate. Additionally, patient-specific parameters (healthier lifestyle, early diagnosis, low disease activity, low cumulative GC dosage, monitoring and treatment of additional risk factors and comorbidities) clearly modify the actual risk of AEs when evaluating the current and future benefit–risk balance of long-term GC treatment [77].
However, the proper use of GCs can be challenging in clinical practice. The lack of standardized protocols for the use of GCs in rheumatological practice can lead to variations in the prescribing practices, which can impact patients’ outcomes. The fear of GC-related AEs, particularly in high-risk patients, can also limit their use, leading to undertreatment and disease progression. Moreover, patient preferences and expectations, such as the desire for quick relief of symptoms, can influence the decision to use GCs, sometimes inappropriately.
The appropriate use of GCs in IRDs is a critical component of the treat to target (T2T) strategies, which involve setting specific targets for disease activity and adjusting therapy to achieve those targets. Indeed, one important aspect of the T2T strategy is the reduction or discontinuation of GC therapy once disease activity is under control. This approach has been shown to improve patient outcomes, reduce the risk of AEs, and increase the likelihood of achieving remission or low disease activity. However, the process of GC reduction or discontinuation must be carefully managed to avoid disease relapses or rebound effects.
In potentially life-threating rheumatic diseases such as SLE or ANCA-vasculitides, which can be a severe, disabling and at times even lethal, potential toxicity could be the price to pay to achieve disease remission and to avoid irreversible organ damage. It should be considered that complete withdrawal of GCs, often sped up, can put the patient at risk of a new flare and re-starting of pulse therapy. A different use of GCs, based on pulse therapy and a combination of synthetic or biologic DMARDs in order to start with lower oral doses and taper rapidly to the safety limit (2.5–5 mg/day), can be implemented in IRDs such as SLE with the result of fewer side effects and a similar efficacy to control disease activity [78].
There should be the option to individualize the decision of withdrawal, not forgetting that complete withdrawal might not be the only or the most crucial measure to minimize GC-related AEs. In this respect, new technologies and approaches, such as biomarkers and genetic testing, may help to identify patients who are at increased risk of AEs or who may be more likely to respond to GC therapy [79–81]. For example, recent studies have shown that genetic variants in the GC receptor gene may influence the response to GC therapy in patients with RA [82].
Additionally, the recent development of a comprehensive instrument assessing GC toxicity, i.e. the glucocorticosteroid toxicity index (GTI), represents a valuable improvement not only for assessing GC-related AEs but also for estimating the clinical value of steroid-sparing agents [83]. From a pragmatic point of view, this score has already been integrated in research as an outcome measure in the phase 3, randomized, double-blind trial of the C5a receptor inhibitor avacopan in the treatment of ANCA-associated vasculitides and also in a recent observational study in GCA patients, whose preliminary data were presented in the EULAR 2022 meeting [84, 85].
Lastly, an advocated additional method for optimizing GC therapy suggested time ago, the usage of GC receptor agonists with the rationale of displaying superior benefit-to-risk ratios compared to standard GCs, including innovative GC receptor ligands and liposomal GCs [86, 87]. However, a recent systematic literature review reported that selective GC receptor modu lators do not appear to be superior over conventional GCs and further developments are needed in this respect [86, 88].
Conclusions
The use of GCs in treating IRDs has been a contentious issue in the past, but there is now agreement that these drugs, while valuable, should be used judiciously.
It is likely that conventional GCs will remain a component of many therapeutic regimens, especially at low doses (≤ 5 mg of PDN-equivalent daily).
Current research is focused on minimizing their use, tapering or discontinuing treatment when possible, and improving safety in long-term cases. Low-dose long-term GC administration also exert DMARD effects in RA treatment.
Clinical experience suggests that elderly individuals with difficult-to-treat IRDs benefit from long-term low-dose GC treatment with good safety profiles. Discontinuing GC treatment in patients who have been on it for extended periods is often challenging due to rebound phenomena or disease flares.
Nevertheless, ongoing monitoring for AEs is crucial for appropriate GC use in IRDs, and such use should follow the T2T strategy while carefully weighing risks and benefits for individual patients. Ultimately, a personalized approach to GC therapy, potentially guided by tomorrow’s biomarkers, is vital to achieving optimal long-term health outcomes and addressing current unmet needs in research and clinical practice.