Introduction
Complementary and alternative medicine (CAM) encompasses a wide range of health practices that fall outside the mainstream healthcare system. Individuals with rheumatic conditions often seek out these treatments for several reasons, such as limited access to conventional therapies due to high costs and strict regulations, concerns about potential side effects of medications, and persistent symptoms despite using pharmaceuticals. Additionally, many view complementary and alternative medicine as natural, which leads to a perception that these methods are generally well tolerated with minimal adverse effects [1].
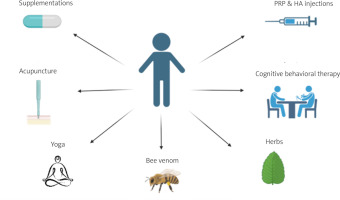
The most popular among these techniques include massage, herbalism, aromatherapy, acupuncture, homeopathy, and reflexology and yoga, which have proved to be an effective type of exercise in the treatment of many rheumatic diseases (Fig. 1) [2]. Several motivating factors have led to the increasing use of CAM by patients, including their dissatisfaction with and perceived ineffectiveness of conventional medicine, lack of trust in the healthcare system, the empowerment felt by patients when placed at the center of their health, the congruence between CAM and spirituality, and the ever-increasing costs of conventional medicine and health insurance premiums [3]. Autoimmune diseases are perceived as uncommon, yet they affect approximately 3–5% of the general population [4]. Despite advancements in research, certain domains remain ambiguous and lack data about autoimmune pathophysiology. Around 100 different autoimmune diseases exist, among which some affect a specific organ such as primary biliary cirrhosis, and some affect various organ systems such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) [5–7]. Despite the presence of established treatment regimens for autoimmune diseases, some regimens still lack effectiveness in controlling the disease; hence the efficacy of complementary and alternative medicine is being investigated thoroughly. The aim of this review is not to disregard conventional medicine or downplay its efficiency, but to demonstrate valuable insights from the literature regarding the utility of CAM in autoimmune disorders. That showcases the effect on patients’ satisfaction, pain modulation and overall adaptation with autoimmune diseases.
Material and methods
We searched through Medline/PubMed, Scopus and DOAJ for relevant papers in regards to CAM and autoimmunity, utilizing Boolean operators. The key words utilized included the Mesh terms “autoimmune diseases” [Mesh], “complementary therapies” [Mesh], “therapeutics” [Mesh].
Systemic lupus erythematosus and complementary and alternative medicine
Systemic lupus erythematosus is a chronic autoimmune disease characterized by multisystem involvement and complications with recurrent relapses [8]. Despite advancements in health care and research, there is currently no cure for SLE, with significant morbidity and premature mortality [9]. Mainstream treatments are based on glucocorticosteroids and immunosuppressants, which are known to have considerable adverse effects. Hence, it is imperative to assess the efficacy of complementary and alternative medicine as a safe adjunct treatment that may reduce inflammation and alleviate symptoms. Among the CAM modalities implicated in the treatment of SLE, we will shed light on acupuncture, mind-body treatments, and biologically based therapies.
Acupuncture
Evidence on the effect of acupuncture on pain in rheumatic conditions is growing; however, few studies have been conducted to date to show its effect in SLE patients. Several theories have been proposed to explain the modality whereby acupuncture has its effect on SLE patients. One of them involves modulation of the immune response, possibly by synchronizing the function of immune cells and cytokines [10]. Another theory is that SLE patients frequently suffer from musculoskeletal pain and inflammation in the joints; hence acupuncture triggers the release of endorphins and other neurotransmitters, potentially offering relief from pain and enhancing the general sense of well-being [11]. A study was conducted to test the effect of acupuncture in reducing pain and fatigue in 24 SLE patients. During the study, patients continued to receive their medical care and were assigned randomly to 10 acupuncture sessions and 10 minimal needling sessions (needles are inserted just under the skin in non-active acupuncture points), and safety measures were taken during each session. The results showed that there was a greater than 30% pain decrease in 40% of the minimal needling and acupuncture patients. In addition, more than a 30% reduction in fatigue was noted in 13% of acupuncture and 25% of minimal needling patients. Hence, this study proposes that SLE patients can undergo acupuncture safely and may experience a reduction in fatigue and pain; however, non-needling control groups and larger samples are required to further study these effects [12]. Furthermore, a recent meta-analysis published in 2023 showed that the synergistic use of acupuncture combined with conventional treatment resulted in improvement in symptoms as well as autoimmune markers and safety profiles [13].
Mind-body treatments
Various mind-body practices such as cognitive behavioral therapy (CBT) along with interpersonal and behavioral treatments have shown encouraging results in improving quality of life, anxiety, pain, and fatigue in SLE patients, which are common in these individuals. Hence these approaches tend to identify and modify distorted and non-functional thought processes [12]. A randomized clinical trial was conducted to decrease stress and pain levels in 92 SLE patients. Participants were divided into 3 groups: randomly assigned to 6 sessions of CBT along with biofeedback (practice to enhance physiological relaxation and self-awareness), supportive counseling (used as a control for non-specific treatment effects such as attention from the therapist), or to a group receiving medical care alone. The results showed that at the end of the treatment period, all three groups had an improvement in their disease status; however, those in the CBT and biofeedback group had a significantly larger reduction in pain and overall better psychological function than the other two groups [14].
Supplements and diet
Vitamin D is often considered an anti-inflammatory agent due to its ability to regulate both adaptive and innate immune systems and to reduce inflammatory cytokines [15]. In comparison with the general population, SLE patients have a higher frequency of vitamin D deficiency due to their avoidance of sunlight to prevent flares [16]. Hence, a relationship between increased lupus activity and vitamin D deficiency suggests that reduced vitamin D plays a role in lupus progression. A systematic review showed that vitamin D supplementation can raise its levels in the serum, decrease inflammation, and may reduce disease activity and preserve bone health [17]. Omega-3 fatty acids possess anti-inflammatory effects via regulating C-reactive protein and anti-inflammatory mediator levels [18]. Systemic lupus erythematosus patients have altered lipid profiles and low omega-3 polyunsaturated fatty acids, which may be related to an increased incidence of cardiovascular complications [19]. Hence, dietary supplements of omega-3 can help regulate lupus activity. Based on available evidence, omega-3 supplements reduce disease activity and may decrease oxidative stress and inflammation, enhance endothelial function and lipid profile, and improve the quality of life [4]. Vitamin E (antioxidant function) can regulate the immune system by inducing protective mechanisms. A study conducted on a mouse model of SLE revealed that vitamin E supplements reduce the production of proinflammatory cytokines, and decrease oxidative stress and the expression of major histocompatibility complex class 2 [20]. Furthermore, a low glycemic index diet as well as a low-calorie diet can reduce weight and fatigue, and improve their quality of life.
Rheumatoid arthritis and complementary and alternative medicine
Rheumatoid arthritis is a chronic autoimmune inflammatory disease characterized by cartilage and bone destruction [21]. Intrinsic as well as extrinsic factors influence RA. Based on statistical data, RA affects 1% of the world’s population [22]. Over the past twenty years, there have been major improvements in the pharmacological treatment of RA. However, despite this improvement, CAM plays an important role in delaying the use of disease-modifying anti-rheumatic agent therapy. Complementary and alternative medicine modalities include acupuncture, traditional Chinese medicine, diet-based therapies, mind-body treatments, and others. Many CAM modalities used in RA will be further discussed in this review. Some commonly used CAM modalities are listed as follows.
Supplements and antioxidant vitamins
Omega-3 fatty acids are polyunsaturated fatty acids mainly derived from marine resources [23]; they are also available as dietary supplements. Clinical trials showed that omega-3 fatty acids are beneficial in reducing blood pressure, inflammatory markers, and triglycerides, and hence important in rheumatic diseases and other obesity-related disorders. A review of clinical trials was conducted in 2017 on the effect of omega-3 fatty acids in SLE, lupus nephritis, RA, and osteoarthritis (OA) [24]. The studies showed that these supplementations improved at least two of the following clinical measures: hand grip strength, duration of early morning stiffness, physician’s global assessment and pain index, the patient’s global assessment, swollen joint account, tender joint account, Ritchie’s articular index, and joint pain intensity. In addition, a 70% improvement in tender joints in 77% of patients receiving these supplements was noted in one of these recent studies. Through the process of lipid peroxidation, oxygen-free radicals are inflammatory mediators responsible for tissue damage in RA patients. In healthy individuals (low levels of reactive oxygen species), plasma antioxidants inhibit lipid peroxidation; in contrast, RA patients are more prone to oxidative damage due to higher lipid peroxidation. Hence, the failure of the antioxidant barrier in RA is responsible for lipid peroxidation and tissue damage.
A study was performed on 40 RA patients to investigate the role of antioxidant therapy in the management of RA patients. These patients were randomly distributed into two subgroups of 20 patients each [25]. One group received the conventional treatment for 12 weeks while the other group received the same treatment along with vitamins A, C, and E as antioxidants for the same period. After 12 weeks of management, blood samples were collected and analyzed for glutathione, total thiols, vitamin C (markers of antioxidant parameters), and malondialdehyde (MDA; marker of oxidative stress). In addition, using the Rheumatoid Arthritis Disease Activity Index (RADAI), the disease activity of the patients was measured at the time of presentation and the end of the period. The results showed that the antioxidant parameters were significantly lower in RA patients in comparison with healthy controls, and a statistically significant post-treatment increase in these parameters was found. Furthermore, significant reductions in the RADAI score and MDA levels were noted post-treatment. According to the previous observations, antioxidants may play a role in reducing oxidative stress and hence inflammatory damage in RA patients.
Yoga
Yoga originates in India and includes physical exercise as well as relaxation techniques [26]. It has been shown to play a role in ameliorating function and reducing pain in many chronic non-malignant diseases including RA, low back pain, fibromyalgia, and OA [27]. A randomized clinical trial performed in 2015 aimed to investigate the role of Hatha yoga in sedentary people with RA compared to wait-list controls. The results showed a notable improvement in physical activity, pain, mental and general health, as well as flexibility and overall quality of life (p < 0.05) [28]. Another review was performed in 2018 investigating the role of yoga and tai chi in RA and spondyloarthropathy patients [29]. The results showed an overall decrease in pain and inflammation levels as well reduction in some inflammatory markers such as interleukin-6 levels and an improvement in the quality of life.
Relaxation techniques
The term “relaxation response” was coined by Dr. Herbert Benson and is aimed at counteracting the effects of the fight or flight response via muscle relaxation, slow breathing, and reduced blood pressure [30]. A randomized controlled trial conducted in 2010 evaluated the effect of CBT and relaxation response training on RA patients [31]. The relaxation regimen includes progressive muscle relaxation, diaphragmatic breathing, and other relaxation skills. The results showed significant amelioration in pain throughout 12 months, but anxiety and depression did not improve. However, no major studies have been performed in this field, and there is insufficient literature; hence no formal conclusions can be made.
Psoriatic arthritis and complementary and alternative medicine
Psoriasis is a multisystemic, inflammatory skin disease affecting most commonly the extensor surfaces of the elbows and knees [32]. Many organs are affected, including peripheral and axial joints, entheses, skin, and nails.
Many studies have been done to explore the effects of alternative clinical medicine on psoriatic arthritis (PsA), though they remain insufficient. Most studies have focused on dietary changes; however, many small studies showed a possible effect of other types of CAM on PsA.
Alternative medicine treatment for spondyloarthritis: psoriatic arthritis and ankylosing spondylitis
In a case study of a 56-year-old male patient with PsA, it was reported that changing the person’s diet led to an 80% decrease in pain, increased mobility, less stiffness and swelling, and some weight loss. The dietary change included a 100% gluten and dairy-free diet, avoiding yeast and eggs, no alcohol, caffeine, or sugar, and some vitamins and supplements such as omega-3 fatty acids EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), folic acid, and vitamin B6 [33]. Other studies have also demonstrated the importance of dietary changes in treating PsA. In a review published in 2020, the authors reported that a cohort of systemic rheumatic disease patients had been surveyed and that the diet change had a “great influence” on their symptoms, with especially gluten-free, low-carbohydrate, high-protein diet, and paleolithic diets being the most popular [34]. The importance of fasting has also been shown: studies have revealed that Ramadan fasting for a month improved C-reactive protein levels, the Disease Activity Index for Psoriatic Arthritis (DAPSA), the Leeds Enthesitis Index (LEI), the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Dactylitis Severity Score (DSS), and the Psoriasis Area Severity Index (PASI) [35]. The Medical Board of the National Psoriasis Foundation stated that dietary weight reduction, using a hypocaloric diet, seems helpful in overweight and obese patients with PsA [36]. It also stated that dietary supplements, especially vitamin D, may help patients with PsA. Some studies suggest that the vitamin D3 analog alphacalcidol leads to significant improvements in the severity of PsA [34].
Concerning ankylosing spondylitis (AS), an extensive review by Kocyigit et al. [1] demonstrated that balneotherapy, which involves soaking in baths filled with thermal or mineral-rich water from natural sources, as well as the application of mud and other natural peloids, was effective in improving disease activity, functionality, quality of life, and mobility in patients with AS. No significant effect was found for pilates, massage therapy or hypnotherapy [1]. Yoga, which includes a variety of poses and postures with specific mechanics, is often emphasized as an exercise that enhances both physical and mental well-being. Practicing the correct techniques in yoga can enhance balance, strength, and flexibility, while also promoting overall health and improving quality of life [2]. Studies with strong evidence assessing the effectiveness of yoga in patients with AS are scarce. Yoga practice incorporates stretching exercises along with proper breathing techniques, which indicates that it may have a beneficial impact on AS [1, 2].
Scleroderma and complementary and alternative medicine
Scleroderma is an uncommon disorder that includes skin thickening or hardening and fibrosis of the involved tissues [37]. Two categories exist: localized scleroderma and systemic scleroderma [38]. There are many alternative therapies implicated in the treatment of scleroderma that have shown a great capacity to treat, and if not, relieve symptoms affecting the functionality of the individual.
Herbal medicinal plants
Salvia miltiorrhiza, a Chinese herbal medicine known for its anti-inflammatory and antioxidant effects, inhibits transforming growth factor β and fibroblast proliferation [39]. Centella asiatica, and especially asiaticoside extraction, has anti-inflammatory characteristics and accelerates wound and ulcer healing [40]. These 2 Chinese medicines, combined, may represent an alternative treatment for scleroderma, as shown in a clinical case study [38]. Other plants are effective in treating scleroderma, for instance, Capparis spinosa L., also with anti-inflammatory and antioxidative effects, can affect systemic sclerosis by reducing oxidative stress and modulating the ROS-ERK1/2-Ha-Ras pathway [41]. Ginkgo biloba L. has, in clinical trials, demonstrated efficacity in improving Raynaud’s phenomenon, a complication of systemic sclerosis [42].
Bee venom
A traditional Chinese medicine, with anti-inflammatory, anti-atherosclerosis activity [43]. Bee venom improved the sleep index in scleroderma patients [42].
Curcumin
Curcumin is helpful in scleroderma treatments. Its protective effects are mainly exerted by modulating the protein kinase C pathway [44]. It also increases apoptosis in damaged cells, thus modulating systemic sclerosis [42].
Cannabis
Many studies have been conducted to explore the effects of cannabidiol (CBD) in treating multiple sclerosis. It has been shown that treatment with CBD was consistently effective, usually resulting in reduced severity of experimental autoimmune encephalomyelitis, including delayed onset of symptoms, attenuation of clinical signs, and reduced disease progression [45]. Also, cannabinol-9-carboxylic acid (also called resunab and lenabasum) was approved by the EMA to treat scleroderma [46].
Musculoskeletal rehabilitation
It has been shown that paraffin wax baths and massage are potentially helpful in the treatment of scleroderma, with several clinical studies demonstrating an increase in joint motion compared to control groups [47].
Hyaluronic acid and platelet-rich plasma
In a prospective open-label study on 10 female patients aged between 18 and 70, each person was given 3 filler injections of hyaluronic acid and platelet-rich plasma and had follow-ups up to 2 years. The results were promising and showed an improvement, though it declined over time. Also, an increase in the skin’s elasticity was noted [48].
Osteoarthritis and complementary and alternative medicine
Osteoarthritis is a disease caused by inflammation of the joints, with inadequate repair [49]. It creates a burden of chronic pain for millions worldwide, including mostly female, elderly, and/or obese patients [50]. This chronic pain can be managed not only by the typical treatment, nonsteroidal anti-inflammatory drugs (NSAIDs), but also by many alternative medicine methods: medical cannabis, Thai massage (TM), Thai herbal compresses (THC), acupuncture, tai chi, botanicals, and other approaches currently under investigation.
Medical cannabis
Using medical cannabis is now recommended for chronic non-cancerous musculoskeletal pain, in North and Latin America, Australia, Europe, and Iran. It can even be used as adjunctive therapy if the first- and second-line therapies are not tolerable or efficient [51]. A study examined whether, and to what extent, cannabis can decrease or even replace the use of opioids for the chronic pain associated with OA [52]. Forty OA patients with chronic pain were certified for the use of medical cannabis and observed 6 months before and after the beginning of treatment. Average morphine milligram equivalents (MME) prescribed decreased to almost half, with 37.5% of patients dropping to 0 MME/day. Visual Analogue Scale (VAS) scores for pain significantly decreased at three and six months of medical cannabis use, while the Global Physical Health score significantly increased. These results prove that medical cannabis reduced the prescription of opioids while improving the patients’ quality of life.
However, since there were only forty patients, and the route and dosage were not tracked, a larger and more generalizable study should be conducted, and future guidelines are needed for the route of administration, dosing, side effects, and long-term efficacy profiles. On another note, a study examined the articular cartilage of patients with symptomatic OA, histologically assessing the expression and localization of cannabinoid receptors [53]. Chondrocytes displayed a large range of cannabinoid receptors, including degenerate tissue, demonstrating the potential efficacy of cannabinoids in these cells. Furthermore, CBD, the non-psychoactive component of cannabis, has been found to primarily affect peroxisome proliferator activated receptor γ (PPARγ) to mediate its therapeutic potential for OA. On the other hand, when CBD activates the TRP (transient receptor potential) channel, usually upregulated in OA, the TRP channel disrupts the analgesic effect of CBD. Knowing the molecular target of CBD, PPARγ, and its site of action, the spinal cord, drugs with CBD can now be more specific [54].
Thai massage and Thai herbal compresses
Another form of alternative medicine that has been found to be equally as efficient as NSAIDs is the use of TM and THC [55]. The TM technique is Suandok massage, directed towards therapy while being low-risk. It targets Chinese acupuncture points specified for the treatment of OA of the knee. THC, on the other hand, applies a herbal ball compress, which is steamed and heated, on the lower extremities.
In a controlled, randomized evaluator-blind trial, 60 OA patients were assigned randomly to receive either oral ibuprofen, TM, or THC. After three weeks, all treatments seemed to cause a comparable improvement and clinical efficacy. The THC group even showed the greatest improvement. Hence, TM and THC could be considered as alternative and complementary treatments for OA of the knee. The massage sessions are efficient in relieving pain up to several weeks after their discontinuation [56].
Similarly, the microwave diathermy used for deep heating therapy can improve pain, physical function, and muscle strength for over 12 months [57].
Acupuncture
Acupuncture, both traditional Chinese and sham, was also demonstrated to clinically improve the chronic pain of OA patients of both the knee and hip through a randomized, multicenter, controlled trial in Germany [58]. Additionally, according to another large trial in Germany, sham acupuncture and traditional Chinese acupuncture improve functionality and pain in OA patients of the knee even more than standard therapy, with no difference observed in the results of sham and traditional Chinese acupuncture [59]. The most recent Cochrane review, including 16 randomized trials, demonstrated statistically and clinically significant short-term improvements in function and pain in the acupuncture group in comparison to the control group of OA patients [60].
Tai chi
Tai chi, another traditional Chinese medicine practice, is a mind-body exercise [61]. “Mind” refers to the positive effects this exercise can impose on life satisfaction, psychological well-being, and perceptions of health, which can in turn address the chronic pain of OA patients. “Body” refers to the positive effects of exercise on balance, muscle strength, aerobic cardiovascular exercises, and flexibility. Tai chi greatly improved physical function and sustained it for up to 24 weeks, according to a randomized trial with 152 OA patients with symptoms in their hips and knees [62]. Another randomized, single-blind trial with 40 patients demonstrated great improvement in depression, self-efficacy, physical function, health status, and pain in comparison with the controls. If the patients sustained their exercise schedule for 12 weeks, the benefits in function and pain were durable [63]. Furthermore, a more recent controlled, randomized trial demonstrated that practicing tai chi for 6 months significantly improved bone mineral density and knee extensor endurance, and even reduced the fear of tripping or falling [64].
Botanicals
While the current approach to arthritis focuses on treating the symptoms, research increasingly involves identifying, isolating, and characterizing the active ingredients from crude extracts of herbs and medicinal plants. Herbs that have been found useful for OA include the following: Camellia sinensis, or green tea, which has a role in the remodeling of the joint; Uncaria tomentosa and Uncaria guianensis, or cat’s claw, which has anti-inflammatory, antioxidant, and immunomodulatory properties; Tripterygium wilfordii Hook F (TwHF), which has immunosuppressive and anti-inflammatory effects; Curcuma longa, or turmeric, which is an antagonist of interleukin-1β signaling that contributes to the pathophysiology of OA, and finally, Zingiber officinale, or ginger, which has been shown to relieve pain and symptoms in OA patients [65].
Side effects of complementary and alternative medicine
Many side effects regarding the use of CAM have been reported, including mechanical injuries, infectious complications, pharmacological interactions, and organ toxicity, which will be discussed further.
Mechanical injuries
A prime example is acupuncture, as needles can harm sensitive and critical body parts, leading to various complications such as pneumothorax, cardiac tamponade, spinal cord injuries and bleeding incidents [66]. A large survey conducted in Australia on 3,700 acupuncture practitioners showed that among 3,222 adverse events, 64 were pneumothorax injuries [67]. Although most cases of incidental pneumothorax cases secondary to acupuncture practice are unilateral, bilateral pneumothorax has been reported in the literature [68, 69].
Another important injury is cardiac tamponade (compression of cardiac tissue secondary to accumulation of pericardial fluid). An example of such injury is the case of an 83-year-old woman who suffered from a cardiac tamponade event, leading to syncope and cardiogenic shock after acupuncture of the sternum [70]. Another incident was the case of a 52-year-old man who presented to medical care and was found to have cardiac tamponade caused by the breakage of a forgotten acupuncture needle in the sternum several years after the acupuncture session [71].
Several cases of direct spinal cord and spinal nerve root injuries as well as indirect injuries due to the migration of needle fragments have been mentioned in the literature [72]. The results of a vast survey on acupuncture and bleeding incidents carried out in Sweden showed that about 14.8% of acupuncture sessions were complicated by bleeding [73].
Hence, given all the previous mechanical incidents, acupuncture should be performed by trained specialists, who are aware of the correct protocols and maneuverability of the procedure as well as the potential complications and their management [66].
Infectious complications
Inadequate sterilization and insufficient hygienic measures regarding acupuncture needles can increase the risk of infections [66]. The most common serious infections include hepatitis and subacute bacterial endocarditis, and other infections have been reported [66]. A survey conducted in Australia showed that 122 out of 3,222 reported adverse events were localized skin infections [67]. In a review article, around 126 cases of acupuncture-associated hepatitis infections were mentioned [74].
Furthermore, a 66-year-old man with a history of long-standing OA suffered from staphylococcal septicemia with disseminated intravascular coagulation caused by acupuncture of the surrounding knee region [75].
Another case report describes the case of 59-year-old woman with a prosthetic heart valve receiving ear acupuncture for headache leading to bacterial endocarditis [76]. In addition, although it is a rare occurrence, acupuncture-associated HIV infection was reported in a 17-year-old boy [77].
Pharmacological interactions
Many herbal medicines can interact and hence alter the pharmacological properties of other drugs, including enzyme kinetics and affinity.
Shankhpushpi, an ayurvedic syrup, was reported to decrease the plasma levels of the anti-epileptic drug phenytoin, hence altering seizure control in epileptic patients [78].
Hypericum perforatum, known as St. John’s wort, has been found to reduce the plasma level of the antihistamine drug fexofenadine by interacting with substrates of a transmembrane transporter [79] and to reduce the plasma concentration of theophylline [80]. In addition, other herbal medicines such as Gingko biloba can alter blood coagulation by interacting with anticoagulants such as warfarin and antiplatelet drugs such as aspirin [81].
Hence, doctors should be careful when prescribing these herbal medicines, as serious side effects can occur.
Organ toxicity
Medical herbal preparations include a mixture of herbs and are widely used to treat various conditions. However, toxicity can result from various causes such as contamination of the preparations, misidentification and naturally occurring unidentified toxins [66].
In an attempt to study contamination of medical herbal medicines with toxic substances, medical herbs used by children, obtained from local markets, were evaluated with gas chromatography and mass spectrometry, and surprisingly high levels of organophosphorus compounds were found [82].
Heavy metals identified in traditional Chinese medicine such as lead, arsenic, thallium, and others have been responsible for several poisoning incidents [66]. Two cases of poisoning from arsenic and mercury have been reported in Indian ethnic medical remedies, leading to significant neurological symptoms [83]. The use of the herbal medicine Syo-saiko-to was reported to cause acute drug-induced liver damage; another case report of Dai-saiko-to-induced autoimmune hepatitis was reported in Japan in a 55-year-old woman [84, 85].
Furthermore, Chines herbs were reported to cause renal damage [66]. A group from Belgium published a case series of 33 patients with Chinese herb-induced nephropathy; severe interstitial fibrosis and parenchymal damage were observed in renal biopsy specimens from these patients [86].
In addition, Ferguson et al. [87] described case of 42-year-old woman with chronic eczema was treated with Chinese herbal medicine, leading to severe dilated cardiomyopathy [87]. Also, severe neurological symptoms were reported in two Chinese patients following the consumption of guijiu (podophyllin containing Chinese herbal broth) [88].
Conclusions
This literature review highlights the increasing interest in alternative medications and remedies for managing autoimmune diseases. While some alternative therapies show promise in symptom relief and improved quality of life, the efficacy and safety of these treatments vary. The demand for alternative approaches in autoimmune care is growing, which emphasizes the need for clinical research to explore the efficacy of these alternative remedies in healing or alleviating the symptoms of autoimmune diseases.