Introduction
Systemic sclerosis (SSc) is a heterogeneous autoimmune disease, the etiology of which is still unknown [1]. There are two main types of SSc: limited (lSSc) and diffuse (dSSc) [2, 3]. Skin involvement (mainly on hands, forearms and face) is characteristic for lSSc, whereas rapid skin and internal organ fibrosis is specific for dSSc [4].
The modified Rodnan skin score (mRSS) is a measure of skin thickness and is used in clinical settings and in clinical trials of SSc [5]. This is a palpation-based semi-quantitative score established in 1979 used for quantitative estimation of skin hardening [6]. Skin thickness is used as a marker of disease activity and mortality in patients with dSSc [6].
Moreover, increase of mRSS among patients with SSc is associated with negative renal and cardiac outcomes [6]. The modified Rodnan skin score is assessed by palpation of skin in 17 areas of the body (fingers, hands, forearms, arms, feet, legs and thighs, face, chest and abdomen) using a scale from 0 to 3, where 0 stands for normal, 1 for mild thickness, 2 for moderate thickness and 3 for severe thickness. Total skin score can range from 0 (normal skin without thickening) to 51 (hard skin with very severe thickening in all examined areas) [7].
Currently, ultrasound (US)-based techniques of skin imaging are being introduced as a potential tool to replace mRSS [8]. The following methods have been evaluated over the course of the last ten years and considered as tools for skin assessment in SSc: ultrasound elastography, shear-wave elastography (SWE), high-frequency ultrasonography (HFU), acoustic radiation force impulse (ARFI) imaging and magnetic resonance imaging (MRI) [9–12].
Material and methods
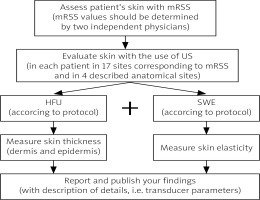
In the present article the authors propose a potential protocol to examine skin involvement among patients with SSc in order to obtain certain repeatability of results and findings (Figure 1). The authors suggest that in order to compare the results with each other researchers should apply the same protocol of examination; therefore, in this article the authors propose a unified protocol based on a literature review and personal experience.
Fig. 1
Proposed protocol of skin examination in systemic sclerosis patients.
HFU – high-frequency ultrasonography, SWE – shear-wave elastography.
Proposed protocol:
Assess patient’s skin with mRSS, then evaluate skin by US applying HFU modality and SWE.
Measure skin thickness (including dermis and epidermis layers – describe each layer) when applying HFU and skin elasticity when applying SWE.
Perform two measurements using the US machine in each patient at 17 sites corresponding to mRSS and at 4 anatomical sites only (right and left middle fingers, right and left dorsal skin of forearms, the area between metacarpophalangeal joints II and III of the right hand, the dorsal skin of the proximal phalanx of the right and left second finger).
During the examination, cover skin at places of US examination with a 10-mm hydrogel pad and a thick layer of gel. Place the transducer perpendicularly to the skin and obtain transverse images. Then, when the area of interest is clearly visualized, perform SWE (the elastography image should be stabilized). The region of interest (ROI) should be placed in the center of the screen and cover approximately 80% of the examined structure. Record three measurements for each ROI and record the average result.
If possible, verify the reproducibility of the results; RSS values should be determined by two independent physicians.
Report and publish your findings. Please record transducer parameters.
For patient comfort, carry out all examinations in a room with an ambient temperature of 20–25°C, with the patient lying in a supine or prone position.
Discussion
Studies suggest that skin thickness (ST) measured with a US-based modality can replace mRSS examination [1, 9–12]. This is mainly because of the positive correlation between skin stiffness and the mRSS in these studies [1, 11, 13–19].
Skin involvement assessed with the mRSS correlates with skin stiffness and thickness. According to personal experience and analyzed studies the authors suggest the use of ultrasound-based techniques, in particular high-frequency ultrasound and shear-wave elastography [9, 10, 13, 14, 17–20].
As many authors have already suggested, HFU allows one to measure dermal thickness and obtain comprehensive imaging of skin layers [9, 10, 13, 14, 17–20]. According to Sobolewski et al. [10] and Flower et al. [19] the HFU technique can distinguish skin layers through examination of ST, SWE and echogenicity. Some studies suggest that whole-body mRSS tended to correlate more closely to the finger or hand skin SE than ST among patients with SSc [20].
According to several authors, the mRSS correlated more positively with skin stiffness than with its thickness [1, 8, 9, 13, 15, 17]; therefore, it is important to test both modalities among a larger group of patients. Interestingly, some authors reported a significant correlation between mRSS and US measurements in the phalanx area [14].
The results suggested that only one measurement at the above-mentioned location could potentially replace the mRSS. Such shortening of US-based examination to only one or two locations could possibly provide a cheap and easy method for clinicians. In order to reach an international consensus, the authors argue for the necessity of use of the same protocol among all physicians treating patients with SSc.



