Current issue
Archive
Online first
About the Journal
Editorial Office
Editorial Board
Publisher
Editorial Policies
Ethical standards and procedures
Abstracting and indexing
Reviewers
Honorary Reviewers
Subscription
Contact
Most read articles
Instructions for authors
Article processing charge (APC)
Books and Events
Books
Events
CASE-BASED REVIEW
Posterior ischemic optic neuropathy as the main manifestation of giant cell arteritis: a case-based literature review
1
Department of Clinical Neuroimmunology, Institute of Neurological Disorders, Poznan University of Medical Sciences, Poland
2
Department of Neurosurgery and Neurotraumatology, Institute of Neurological Disorders, Poznan University of Medical Sciences, Poland
3
Department of Clinical Pathomorphology, Poznan University of Medical Sciences, Poland
Submission date: 2025-04-06
Final revision date: 2025-06-11
Acceptance date: 2025-07-01
Online publication date: 2026-01-08
Corresponding author
Nina Barankiewicz-Tyc
Institute of Neurological Disorders, Department of Neurology, Poznan University of Medical Sciences, Poznan, Poland
Institute of Neurological Disorders, Department of Neurology, Poznan University of Medical Sciences, Poznan, Poland
KEYWORDS
TOPICS
ABSTRACT
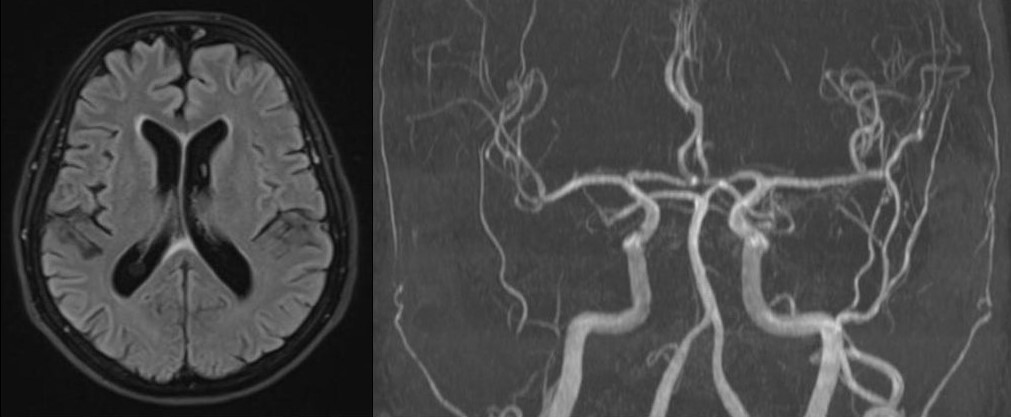
This case-based literature review aims to challenge a common misconception that elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels, halo sign on temporal artery ultrasound, and arteritic anterior ischemic optic neuropathy are essential to make a diagnosis of giant cell arteritis (GCA). Here, we present a case of a 70-year-old woman with a biopsy-proven GCA who met the 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology Classification Criteria for Giant Cell Arteritis. On admission she complained of left temporal headache, left scalp tenderness, constitutional symptoms and visual disturbances in her left eye that was diagnosed as posterior ischemic optic neuropathy. Erythrocyte sedimentation rate and CRP levels were within normal limits, and the patient had no halo sign on the temporal artery ultrasound. It is crucial to carefully evaluate visual disturbances in elderly patients, since missing a diagnosis of GCA can have catastrophic consequences, such as bilateral blindness, aortic dissection, stroke, or myocardial infarction.
REFERENCES (33)
1.
Laskou F, Coath F, Mackie SL, et al. A probability score to aid the diagnosis of suspected giant cell arteritis. Clin Exp Rheumatol 2019; 37 Suppl 117: 104–108.
2.
Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol 2021; 73: 1349–1365, DOI: 10.1002/art.41774.
3.
Ponte C, Grayson PC, Robson JC, et al. 2022 American College of Rheumatology/EULAR Classification Criteria for Giant Cell Arteritis. Arthritis Rheumatol 2022; 74: 1881–1889, DOI: 10.1002/art.42325.
4.
Bilton EJ, Mollan SP. Giant cell arteritis: reviewing the advancing diagnostics and management. Eye (Lond) 2023; 37: 2365–2373, DOI: 10.1038/s41433-023-02433-y.
5.
Khalique MI, Arjunan M, Wood S, Mackie SL. The spectrum of giant cell arteritis through a rheumatology lens. Eye (Lond) 2024; 38: 2437–2447, DOI: 10.1038/s41433-024-03153-7.
6.
Castillejo Becerra CM, Crowson CS, Langenfeld HE, et al. Population-Based Performance of Inflammatory Markers in Giant Cell Arteritis. Am J Ophthalmol 2025; 275: 47–51, DOI: 10.1016/ j.ajo.2025.03.022.
7.
Monti S, Schäfer VS, Muratore F, et al. Updates on the diagnosis and monitoring of giant cell arteritis. Front Med (Lausanne) 2023; 10: 1125141, DOI: 10.3389/fmed.2023.1125141.
8.
vvan der Geest KSM, Sandovici M, Bley TA, et al. Large vessel giant cell arteritis. Lancet Rheumatol 2024; 6: e397–e408, DOI: 10.1016/S2665-9913(23)00300-4.
9.
Sebastian A, Coath F, Innes S, et al. Role of the halo sign in the assessment of giant cell arteritis: a systematic review and meta-analysis. Rheumatol Adv Pract 2021; 5: rkab059, DOI: 10.1093/rap/rkab059.
10.
Chu R, Foster C, Ali M, et al. Optimal length and usefulness of temporal artery biopsies in the diagnosis of giant cell arteritis: a 10-year retrospective review of medical records. Lancet Rheumatol 2020; 2: e774–e778, DOI: 10.1016/S2665-9913(20)30222-8.
11.
Parreau S, Liozon E, Chen JJ, et al. Temporal artery biopsy: A technical guide and review of its importance and indications. Surv Ophthalmol 2023; 68: 104–112, DOI: 10.1016/j.survophthal. 2022.08.008.
12.
Agostino A, Farmer J, Blanco P, et al. Efficacy of bilateral temporal artery biopsies and sectioning of the entire block of tissue for the diagnosis of temporal arteritis. Cardiovasc Pathol 2022; 59: 107425, DOI: 10.1016/j.carpath.2022.107425.
13.
Hayreh SS. Posterior ischaemic optic neuropathy: clinical features, pathogenesis, and management. Eye (Lond) 2004; 18: 1188–1206, DOI: 10.1038/sj.eye.6701562.
14.
Maramattom BV, Sundar S, Thomas D, Panikar D. Postoperative posterior ischemic optic neuropathy (PION) following right pterional meningioma surgery. Ann Indian Acad Neurol 2016; 19: 374–376, DOI: 10.4103/0972-2327.186826.
15.
Srinivasan S, Moorthy S, Sreekumar K, Kulkarni C. Diffusion- weighted MRI in acute posterior ischemic optic neuropathy. Indian J Radiol Imaging 2012; 22: 106–107, DOI: 10.4103/0971-3026.101082.
16.
Albarrak AM, Mohammad Y, Hussain S, et al. Simultaneous bilateral posterior ischemic optic neuropathy secondary to giant cell arteritis: a case presentation and review of the literature. BMC Ophthalmol 2018; 18: 317, DOI: 10.1186/s12886-018-0994-9.
17.
Héron E, Sedira N, Dahia O, Jamart C. Ocular Complications of Giant Cell Arteritis: An Acute Therapeutic Emergency. J Clin Med 2022; 11: 1997, DOI: 10.3390/jcm11071997.
18.
Chazal T, Clavel G, Leturcq T, et al. Characteristics and Prognosis of Binocular Diplopia in Patients With Giant Cell Arteritis. J Neuroophthalmol 2024; 44: 87–91, DOI: 10.1097/WNO. 0000000000001912.
19.
Ross M, Bursztyn L, Superstein R, Gans M. Multiple Cranial Nerve Palsies in Giant Cell Arteritis. J Neuroophthalmol 2017; 37: 398–400, DOI: 10.1097/WNO.0000000000000529.
20.
Pellegrini F, Mairot K, Cuna A, Lee AG. Paracentral acute middle maculopathy in giant cell arteritis. Retin Cases Brief Rep 2024; 18: 285–289, DOI: 10.1097/ICB.0000000000001381.
21.
Kasimov M, Popovic MM, Micieli JA. Paracentral Acute Middle Maculopathy Associated With Anterior Ischemic Optic Neuropathy and Cilioretinal Artery Occlusion in Giant Cell Arteritis. J Neuroophthalmol 2022; 42: e437–e439, DOI: 10.1097/WNO. 0000000000001306.
22.
Sverdlichenko I, Lam C, Donaldson L, Margolin E. Horner Syndrome in Giant Cell Arteritis: Case Series and Review of the Literature. J Neuroophthalmol 2022; 42: 340–345, DOI: 10.1097/WNO.0000000000001593.
23.
Wong CW, Alryalat SA, Al Deyabat O, Lee AG. Ophthalmic Manifestations of Giant Cell Arteritis. Exp Rev Ophthalmol 2024; 19: 133–140, DOI: 10.1080/17469899.2024.2306583.
24.
Hayreh SS. Giant cell arteritis: Its ophthalmic manifestations. Indian J Ophthalmol 2021; 69: 227–235, DOI: 10.4103/ijo.IJO_1681_20.
25.
Casella AMB, Mansour AM, Ec S, et al. Choroidal ischemia as one cardinal sign in giant cell arteritis. Int J Retina Vitreous 2022; 8: 69, DOI: 10.1186/s40942-022-00422-z.
26.
Dzhus M, Mostbauer H. Cardiovascular lesions in giant cell arteritis. Reumatologia 2022; 60: 399–407, DOI: 10.5114/reum.2022.123670.
27.
Conticini E, Falsetti P, Bardelli M, et al. Giant cell arteritis presenting as a stroke in the internal carotid artery territory: a case-based review. Reumatologia 2021; 59: 121–125, DOI: 10.5114/reum.2021.105414.
28.
Dejaco C, Ramiro S, Bond M, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice: 2023 update. Ann Rheum Dis 2024; 83: 741–751, DOI: 10.1136/ard-2023-224543.
29.
Ponte C, Rodrigues AF, O’Neill L, Luqmani RA. Giant cell arteritis: Current treatment and management. World J Clin Cases 2015; 3: 484–494, DOI: 10.12998/wjcc.v3.i6.484.
30.
Albarrak AM, Mohammad Y, Hussain S, et al. Simultaneous bilateral posterior ischemic optic neuropathy secondary to giant cell arteritis: a case presentation and review of the literature. BMC Ophthalmol 2018; 18: 317, DOI: 10.1186/s12886-018-0994-9.
31.
Nichani P, Biousse V, Newman NJ, Micieli JA. Vision Loss From Giant Cell Arteritis in Patients With Other Ocular Diagnoses. J Neuroophthalmol 2021; 41: e254–e258, DOI: 10.1097/WNO.0000000000001064.
32.
Arai T, Sawamura H, Shoda H, et al. A case of posterior ischemic optic neuropathy due to giant cell arteritis with advanced glaucoma. Neuro-Ophthalmology Japan 2017; 34: 54–60.
33.
Yan Y, Li Z, Luo Y, et al. Biopsy-Proven Giant Cell Arteritis Associated Vision Loss in Chinese Subjects: A Case Series and Review of the Literature. Neuroophthalmology 2022; 47: 79–87, DOI: 10.1080/01658107.2022.2099427.
Copyright: © Narodowy Instytut Geriatrii, Reumatologii i Rehabilitacji w Warszawie. This is an Open Access journal, all articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0) License (https://creativecommons.org/licenses/by-nc-sa/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, provided the original work is properly cited and states its license.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.