Introduction
Radiosynovectomy (RSV) is a minimally invasive method of treating and controlling joint inflammation refractory to conventional pharmacotherapy [1]. The most common indications for RSV are rheumatoid arthritis (RA), ankylosing spondylitis (AS), and psoriatic arthritis (PsA). All peripheral joints can potentially be treated with RSV, however, hip joint is one of the least common joints on which RSV is performed.
The aim of the study was to assess the efficacy and safety of the hip joint RSV, based on a case series of 14 patients.
Material and methods
This retrospective study included a total of 14 patients who underwent a hip joint RSV between the years 2016 and 2021 (10 female, 4 male; aged 8 to 79; mean age 48 years; in all the female patients of childbearing age pregnancy was excluded before the procedure).
Overall, 21 hip RSVs were performed: 8 patients had a single RSV, 2 patients had an RSV of both hips, 3 patients had 2 RSVs of the same hip and 1 patient had 2 RSVs of the right hip and 1 RSV of the left hip.
The patients were diagnosed as follows: RA (5 patients), AS (2 patients), PsA (1 patient), unspecified arthritis (UA, 1 patient), pigmented villonodular synovitis (PVNS, 1 patient), osteoarthritis (OA, 3 patients), joint effusion in course of the femoroacetabular impingement syndrome (FAI, 1 patient).
All the patients had a follow-up history of at least 6 months. The effects of the treatment were assessed clinically and ultrasonographically.
Selection
Before the RSV, all the patients underwent clinical and ultrasound (US) examination (Aloka Prosound Alpha 6, 3–5 MHz Convex Probe UST-9123). Clinical criteria for selection included pain, tenderness and restriction of the hip joint motion; ultrasound criteria included effusion, synovial hypertrophy and increased vascularity in power Doppler, visible in the anterior longitudinal projection parallel to the femoral neck (Fig. 1).
Fig. 1
Ultrasound of the hip joints, anterior longitudinal projection along the femoral neck: effusion at the junction of the femoral neck and head (A), spinal needle approaching the femoral neck (B) (H – femoral head, N – femoral neck).

All patients with inflammatory arthropathies had been treated for at least 6 months with disease-modifying antirheumatic drugs (synthetic or biological) prior to RSV. Patients with OA and FAI had at least one prior intraarticular glucocorticosteroid injection, which failed to relieve the symptoms. The patient with PVNS underwent diagnostic arthroscopy, and the RSV was the first line of treatment.
Injection procedure
All the RSVs were performed under direct US guidance using an aseptic technique. The course of the femoral vessels was ultrasonographically identified to determine the safest site for injection. Following disinfection, the skin and subcutaneous tissue at the injection site were anesthetized with 1% lidocaine.
The injection was performed with the 22-G spinal needle using the anterolateral approach, under real-time US guidance. The tip of the needle was directed at the junction of the femoral neck and head, where the biggest fluid collection was usually present (Fig. 1).
After aspiration of any excess fluid, a radiopharmaceutical was injected, followed by 40 mg of methylprednisolone to avoid exacerbation of symptoms due to radiation-induced synovitis. The needle was flushed with 1–5 ml saline during withdrawal to prevent needle-tract burns.
Radiopharmaceutical
As for any other medium-sized joint, rhenium-186 sulfide (186Re, CIS Bio International, France) was the radiopharmaceutical of choice. The administered activities of 186Re ranged from 74 to 148 megabecquerels (MBq), depending on body mass, age and severity of the joint inflammation; 111 MBq was injected in 13 cases, 74 MBq in 6 cases, and 148 MBq in 2 cases.
Post-therapeutic scintigraphy
Directly after the RSV, each patient underwent a post-therapeutic planar scintigraphy with a single-head gamma camera (Nucline TH, Mediso) using 186Re gamma emission (137 keV photopeak, 10% energy window). Two patients also aunderwent a single photon emission computed tomography/computed tomography (SPECT/CT) with a hybrid gamma camera (Symbia, Siemens) (Figs. 2 and 3).
Fig. 2
Post-therapeutic single photon emission computed tomography/computed tomography of the hip joints after radiosynovectomy (patient 1) – radiopharmaceutical activity visible around the femoral neck and in the joint space with no extraarticular leakage: coronal cross-section (A), 3D volume rendering reconstruction (B).
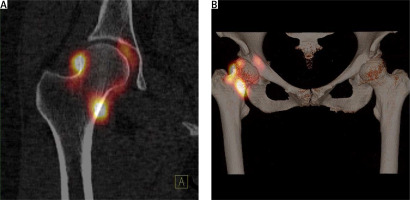
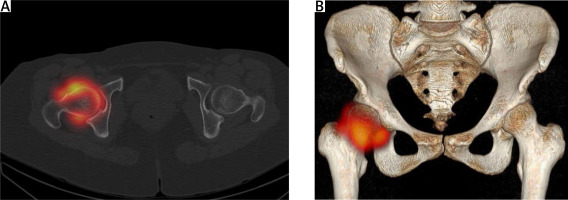
Fig. 3
Post-therapeutic single photon emission computed tomography/computed tomography of the hip joints after radiosynovectomy (patient 2) – radiopharmaceutical activity visible around the femoral neck and in the joint space with no extraarticular leakage: transverse cross-section (A), 3D volume rendering reconstruction (B).
Patient management after radiosynovectomy
In order to minimize the risk of radiopharmaceutical leakage and radiation burns, hip joints were immobilized for 48 hours after the RSV. To prevent deep vein thrombosis in the immobilized limbs, 11 patients were prescribed low molecular weight heparin for 5 days.
Two patients had already been treated with an oral anticoagulant (rivaroxaban) for unrelated conditions. The 8-year-old boy with PVNS did not receive any anticoagulant prophylaxis, since the consulting pediatrician deemed it unnecessary.
Effects evaluation
All patients had at least 2 follow-up visits 3 and 6 months after the RSV. As in initial selection, clinical and US examinations were performed.
Bioethical standards
This is a retrospective analysis. All patients underwent the procedure in connection with planned management in the course of treatment. Adult patients gave informed consent to the procedure, in the case of children under 16, the consent of their parents/legal guardians was obtained, after the age of 16, the consent for the procedure was signed by the parents/legal guardians and the patient. All activities were in line with the ethical principles according to Helsinki’s Declaration.
Results
In 9 cases, complete resolution of symptoms was seen 3 and 6 months after the RSV. The patients experienced no pain, there was no restriction in the range of motion of the hip joint, and US examination revealed no fluid or an increased power Doppler signal in the synovial tissue.
In 4 cases, the RSV initially had a satisfactory effect, but after 6 months, inflammation symptoms recurred. In all these patients, lasting improvement was achieved after the second RSV. In 4 cases, the treatment effects were negligible or absent altogether after 3 and 6 months, and no repeated treatment attempt was made.
In total, the percentage of successfully treated hip joints was 62% (13 cases). In 19% of the hip joints (4 cases), the treatment effects were transient, while in 19% (4 cases) the procedure had no effect. All the responders had a diagnosis of systemic joint disease or PVNS. Conversely, the non-responders had either OA or FAI.
Three patients who required second RSV responded to higher 186Re activities. In two cases, the initial activity was 74 MBq, increasing to 111 MBq for the repeated treatment. In the third case, the initial activity was 111 MBq, increasing to 148 MBq for the second RSV. One patient responded well to the second injection without dose escalation (111 MBq for both injections).
All the patients tolerated the procedure well. No major complications or adverse events occurred; in particular there were no cases of radiation necrosis or needle-tract burns. One patient experienced mild pain in the general area of the injection, which lasted for 4 weeks after the RSV, and resolved without intervention.
Two patients who were concomitantly treated with biological agents (one with etanercept, and the other with golimumab) manifested no signs of infection, either local or systemic, during the whole observation period.
The 8-year-old patient with PVNS is particularly noteworthy. He did not require general anesthesia and tolerated the procedure very well, with only local anesthesia with lidocaine. For over 12 months after the RSV, he has been symptom-free.
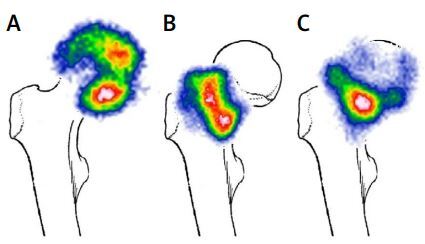
In the post-therapeutic scintigraphy, three distribution patterns were identified (Fig. 4).
Fig. 4
Post-therapeutic planar scintigraphy images in anteroposterior projection superimposed on an anatomical drawing. Patterns of distribution – acetabular (A), around the femoral neck (B), mixed (C).
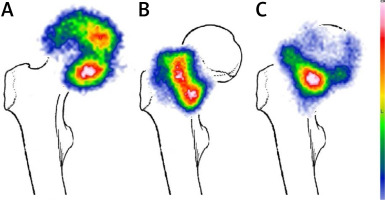
The most prevalent pattern seen in 9 cases was a mixed one, with radioactivity visible in the acetabulum around the femoral head and at the injection site, around the femoral neck. In 6 cases, radioactivity was seen only in the acetabulum, and in 6 cases only around the femoral neck. No foci of radioactivity suggestive of extraarticular injection were observed in any of the scintigrams.
The distribution pattern of the radiopharmaceutical did not seem to correlate with the treatment effects.
Discussion
Hip joint involvement is common in most systemic arthropathies, with prevalence of 15–26% in RA, 24–36% in AS, and 15% in PVNS [2–6]. In psoriatic arthritis, hip arthritis occurs in less than 7% of patients, but is often associated with quick joint degeneration [7–10]. Hip arthritis can be present even in the early stages of the inflammatory disease, however, the clinical symptoms may be scarce or absent altogether for prolonged periods [2, 7].
When the disease manifests clinically, the destructive changes are usually severe, and the only viable treatment option is joint replacement. In rheumatoid arthritis, over one-third of patients requires arthroplasty, most commonly total hip replacement [9].
Early, aggressive treatment of active inflammation can improve patient’s life quality and functional performance of the hip joint, and possibly delay or even prevent the need of joint replacement. It has already been suggested that RSV performed at early stages can slow down or stop altogether radiographic progression of the hip joint degeneration [11].
As such, RSV seems a viable treatment option in the management of hip joint inflammation over arthroscopic synovectomy in terms of invasiveness, safety and cost-effectiveness [12].
The results of our study support these hypotheses. Most of our patients responded very well to RSV treatment without any major complications during the observation period. The radiosynovectomy was effective in all the patients with systemic joint diseases and PVNS. Lack of efficacy in the osteoarthritis subgroup can be most likely attributed to advanced joint degeneration.
Moreover, positive outcomes of our study emphasize the importance of ultrasonography in the entire RSV process. Contrary to Szerb et al. [11], rather than fluoroscopy with iodine injection, we used only ultrasound guidance to puncture the hip joint. As proven by post-therapeutic scintigrams, all the injections were intraarticular, with no traces of extraarticular radioactivity.
This is of great importance, since the radioisotope leakage can lead to the most serious complication of RSV: radiation-induced soft tissue necrosis. None of the patients exhibited symptoms of paraarticular soft tissue damage such as skin necrosis, or milder reactions such as beta burns [13].
We conclude that the ultrasound-guided injection is safe, accurate and preferable to fluoroscopy, since it eliminates additional exposure to X-rays and potential adverse effects of iodine contrast media.
As in our previous research [14], we did not observe any septic complications following RSV in patients concomitantly treated with biological disease-modifying antirheumatic drugs. Unlike open surgical or arthroscopic synovectomy, RSV does not require discontinuation of the biological therapy, which is yet another advantage to the patient.
Study limitations
The major limitations of our study are its retrospective nature, small patient group and lack of information regarding biochemical indicators of the inflammation, disease activity indices (e.g. DAS28, VAS) and imaging studies assessing the degree of preexisting structural joint degeneration. Another limitation is a relatively short observation period of 6 to 12 months.
Conclusions
Radiosynovectomy of the hip joint in systemic joint diseases, especially performed using ultrasound-guidance, is an effective treatment modality. With its high safety profile, it is an attractive alternative to open or arthroscopic surgery, even in patients undergoing biological treatment.