Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease of the joints that shows slow progression. Inadequate treatment of RA may lead to uncontrolled disease activity and complications such as deformity, disability and organ damage. Thus, regular outpatient visits to physicians are necessary to ensure that patients take their medicine regularly and monitor disease activity status, drug side effects and drug dose adjustment [1]. According to the literature, if disease activity failed to improve by at least 50% within 3 months, the probability of reaching the treatment goal of remission would be low [2, 3]. Unfortunately, there were patients who did not attend every scheduled outpatient visit and got lost to follow-up (LTFU), which would potentially lead to a deterioration in their disease.
A few studies have reported the frequency and factors associated with LTFU in RA patients. Fear of or experience of drug side effects, perceived lack of efficacious therapies, economic costs, and difficulties with the health care environment were major barriers to treatment compliance at Ben Taub General Hospital, Houston, Texas [4]. Moving to another medical institution due to convenience and stopping medication due to medical symptoms were the main identified reasons for LTFU in Central Taiwan [5]. However, no previous studies have analysed factors associated with LTFU of RA patients in Indonesia. This study aimed to determine the frequency of loss to follow-up and the possible associated factors in newly diagnosed RA patients in the rheumatology outpatient clinic Cipto Mangunkusumo General Hospital, Indonesia. The majority of the patients in our clinic are covered by Indonesia’s government insurance. While there are several hospitals nearby, our hospital is a teaching facility of the Faculty of Medicine, Universitas Indonesia, and serves as a national referral centre. We receive patients from other centres for further diagnostic evaluation and appropriate treatment.
Material and methods
Study population
This is a retrospective cohort study of newly diagnosed RA patients who came to our rheumatology outpatient clinic between May 2021 and November 2022. The inclusion criteria were RA patients with disease onset at least 18 years old. The exclusion criteria were: 1) having a change of diagnosis from RA to another rheumatic autoimmune disease during follow-up visits, 2) having other rheumatic autoimmune diseases, 3) the medical number was no longer registered. Data of their active job status, parental status, comorbidity, disease activity scores, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were recorded for analysis.
Definition of lost to follow-up and routine follow-up
In our rheumatology outpatient clinic, the frequency of regular RA outpatient visits was every 1 to 3 months. Patients who did not attend their scheduled appointment for more than 3 months were defined as LTFU. In this study, we included patients whose first visit to our clinic was from May 2021 onwards. Patients who attended our clinic before May 2021 were excluded from this study. The patients were classified into different groups. First, those who regularly returned for their scheduled appointments were defined as the routine follow-up (RFU) group. Second, those who returned for their late appointment before December 2022, even after 3 months of being late for their initial appointment date, were still classified as the RFU group. Third, those who did not attend their scheduled appointment for more than 3 months and still did not return before December 2022 were defined as the LTFU group. The LTFU group was divided into 3 subgroups: those who could not be contacted after 3 phone calls or had no functional phone number or refused to participate; those with documented reasons for not returning to our outpatient clinic; and those who were confirmed to be deceased. Then, we took age-matched routinely followed-up patients as a control group. We calculated the total number of patients in this cohort as the denominator.
Data collection
Demographic data, including age, sex, employment status, the presence of symptoms at the last visit, and comorbidities were obtained from medical records. Prior to initiating the questionnaire retrieval process, we engaged in proactive communication with individuals classified as LTFU via text messages. The objective was to confirm their last visit, and to serve as a reminder for them to return to our rheumatology outpatient clinic. A crucial element of this interaction included an open-ended question: “Why didn’t you return for your appointment?” This question provided valuable insights, outlining the potential factors contributing to LTFU. Subsequently, through extensive discussions involving rheumatology staff in our department and members of the patient support group community, we identified and consolidated 8 possible reasons for LTFU: distance constraints, transportation constraints, time constraints due to busy schedules, challenges in comprehending the hospital registration flow system, dissatisfaction with outpatient services, discontinuation of medication due to minimal symptoms, the presence of comorbidities, and a lack of information about their disease. We then developed these into a questionnaire that comprises several questions for a more detailed exploration. To gather comprehensive data, we employed telephone communication to reach out to both LTFU and RFU patients. We ensured that respondents provided honest answers by clearly explaining the consent process at the outset. Patients were informed that their responses would not impact their care or treatment at the clinic. This was emphasized to minimize any potential biases or socially desirable responses.
Statistical analysis
We used a Likert scale questionnaire to explore the perception and the possible reasons for LTFU. We took age-matched RFU patients from the same population as the control group. The chi square test was used to evaluate the difference of perception between LTFU patients and controls. To find the most significant variable associated with LTFU, bivariate and multivariate logistic regression analyses were performed. A p-value < 0.025 was considered significant in the preliminary analysis, while a p-value < 0.05 was considered significant in the multivariate analysis. Statistical analysis was analysed using SPSS Statistics 26 for Windows.
Results
Frequency of loss to follow-up
A total of 260 newly diagnosed RA patients were documented from May 2021 to November 2022. Among them, 65 patients (25%) were LTFU patients who met the study inclusion and exclusion criteria. We successfully contacted 34 of these patients; 3 patients had passed away, 28 patients either had non-functional phone numbers or did not respond to our calls, and 1 patient declined to participate, stating that they felt it was unnecessary to answer. Figure 1 illustrates the frequency of LTFU in newly diagnosed RA patients and the 3 subgroups of LTFU.
Demographic characteristics
The majority of participants were female (94%). The mean age was 44 years. Figure 2 shows the age range distribution of LTFU patients who could be contacted. Most of the participants were busy with their work, still had symptoms, and had no comorbidity. The characteristics of subjects are summarized in Table I.
Table I
Demographic characteristics of total LTFU patients, LTFU patients evaluated, and RFU patients as control group
Identified reasons for loss to follow-up from our rheumatology outpatient clinic
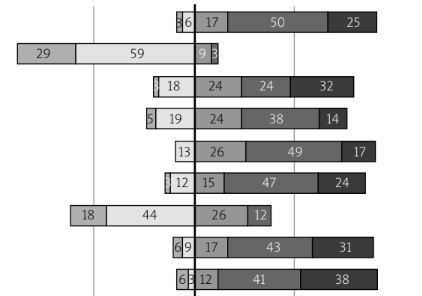
By using a questionnaire consisting of several Likert scale questions, this study could identify the perceptions of patients regarding factors associated with LTFU. Each constraint was represented by several questions (Fig. 3). Accordingly, 76% of LTFU patients had a distance problem from their house to the hospital, 56% were busy with their work or childcare and thus were not able to visit our clinic, 38% had transportation constraints, 21% felt dissatisfied with the outpatient clinic service, 18% patients had lack of information about their disease, 15% had other comorbidities that compelled them to go to another department’s clinic, 9% had difficulties understanding the clinic registration flow system, and 6% only had minimal symptoms that led them to stop their treatment.
Fig. 3
Factors associated with loss to follow-up as assessed by Likert scale ratings.
An average Likert scale rating below 3 is considered indicative of constraints.

Distance constraints
The distance between the patients’ homes and our hospital emerged as a hindrance to adherence for regular hospital visits. Seventy-six percent of patients reported facing limitations due to the distance between their homes and our hospital. Furthermore, 24% of patients underwent home relocations within the last 3 months, resulting in additional expenses and time commitments to attend our clinic. Therefore, they chose to visit rheumatology clinics closer to their new homes.
Transportation constraints
The observation that 76% of patients encountered challenges with distance implies a possible intersection with transportation constraints, involving concerns about accessibility and associated costs. Specifically, 24% of patients reported difficulty in accessing transportation, while 47% perceived the transportation cost from their home to our hospital as prohibitively high.
Busyness
Our patients mostly were in the productive age range; thus they might be busy at work during their scheduled hospital visit. Scheduling difficulties due to work commitments affected 36% of patients when arranging appointments. Furthermore, an equivalent percentage of patients (36%) found themselves engrossed in childcare responsibilities, rendering them too preoccupied to attend appointments at our rheumatology outpatient clinic.
Unclear information and instructions
Only 9% LTFU patients think that the instructions and information provided in the hospital were not easily understandable. Therefore, it seems that unclear information and instructions were not the primary factors associated with loss to follow-up.
Poor services
Among LTFU patients, 21% expressed that our hospital provided poor services. Our questionnaire revealed that 15% were dissatisfied with the hospital services, 6% felt that the services were not hospitable, 62% felt that the waiting time in the queue was long, and 15% perceived that the consultation duration was insufficient.
Stopping medication due to absence of or minimal symptoms
Our investigation found that 6% of patients became LTFU from our outpatient clinic due to the absence or minimal manifestation of symptoms. Additionally, 12% expressed that their symptoms did not significantly impede their daily activities. Two patients (6%) articulated the perception that minimal symptoms were deemed acceptable, justifying their deviation from regular outpatient visits.
Comorbidities
Apparently, 15% of patients had other comorbidities that compelled them to go to other departmental clinics, and thus were absent from the rheumatology clinic. The prioritization of other departmental clinics over the rheumatology outpatient clinic was notably observed in this subset of patients.
Lack of information about their disease
Twenty-one percent of patients often forget to attend their appointment, owing to the underestimation of disease, which could have contributed to the adherence barrier. The contrast between the perceived beneficial effects of therapy and the potential toxicities of drug treatment could adversely impact treatment adherence among patients. From our findings, 88% of patients feared or experienced drug side effects. Additionally, 9% of patients reported perceiving ineffective treatment, with a subset expressing the belief that re-evaluation was unnecessary. Recognizing the impact of inadequate disease awareness on decision-making, formulating strategies aimed at enhancing patient adherence was needed.
Statistical analysis
As shown in Table II, χ2 analysis indicated that transportation constraints and busyness were significantly associated with loss to follow-up (p-value 0.008 and 0.2, respectively). For further analysis, we performed multivariate logistic regression. As seen in Table III, the final multivariate analysis showed a strong association between transportation constraints and loss to follow-up (OR = 6.397; 95% CI: 1.622–25.228).
Table II
Factors associated with loss to follow-up by χ2 test
| Variables | LTFU patients (n = 34) | RFU patients as control (n = 34) | p in χ2 |
|---|---|---|---|
| Distance constraints [n (%)] | 26 (76) | 22 (65) | 0.290 |
| Transportation constraints [n (%)] | 13 (38) | 3 (9) | 0.008* |
| Busyness [n (%)] | 19 (56) | 12 (35) | 0.200* |
| Unclear information and instructions [n (%)] | 3 (9) | 2 (6) | 0.644 |
| Poor services [n (%)] | 7 (21) | 1 (3) | 0.999 |
| Minimal symptoms [n (%)] | 2 (6) | 0 (0) | 0.999 |
| Comorbidities [n (%)] | 5 (15) | 0 (0) | 0.999 |
| Lack of awareness [n (%)] | 6 (18) | 1 (3) | 0.999 |
Table III
Factors associated with lost to follow-up by multivariate logistic regression
| Variables | LTFU patients evaluated (n = 34) | RFU patients as control (n = 34) | p-value in multivariate logistic regression | OR | 95% CI |
|---|---|---|---|---|---|
| Transportation constraints [n (%)] | 13 (38) | 3 (9) | 0.008* | 6.397 | 1.622–25.228 |
Discussion
In this study, we investigated the rate of LTFU among RA patients during outpatient visits, along with its associated factors. We found that a quarter of our newly diagnosed patients were lost to follow-up, a figure comparable to LTFU rates in studies on various rheumatic diseases [5], as well as other chronic conditions requiring regular outpatient care, in the approximate range of 20–30% [6–10]. Variability exists due to differences in study locations, definitions of LTFU or treatment non-adherence, medical specialties, and patient populations [9]. Differences in LTFU frequency were also observed among different rheumatic diseases, ranging from 23.9% in RA to higher rates of approximately 35% in conditions such as ankylosing spondylitis and psoriasis or psoriatic arthritis [5].
Our findings highlight transportation barriers as independently associated with follow-up discontinuation among RA patients, consistent with previous studies [7, 11]. Relocating to a nearby district hospital for convenience was found to be the most common reason for LTFU among RA patients, often without informing their original hospital [5]. Furthermore, RA is a debilitating disease that may result in difficulties with commuting [12, 13].
Transportation constraints in our study were related to costs and ease of access. Among our LTFU patients, 47% perceived transport costs from their residence to the hospital as high, emphasizing the need for an affordable and widely accessible public transport system, especially in lower-middle-income countries. However, this remains a significant issue in Indonesia. In Jakarta, buses and commuter trains are the primary means of public transportation, but commuting with public transport might be challenging for RA patients with functional disabilities, given the city’s high population density and mobility. Ride-sharing applications offer a more comfortable transportation alternative but at higher costs. Additionally, during the COVID-19 pandemic, measures for social and physical distancing limited public transportation capacity, further restricting urban mobility.
Efforts have been made across countries to overcome transportation barriers to medical care, including transportation reimbursement, vouchers, and bus passes [14]. Telemedicine has also gained popularity during the pandemic, with high satisfaction rates [15]. However, many patients with rheumatic autoimmune diseases still require in-person hospital consultations [16]. Barriers to telemedicine, such as access to internet connections and video-call devices, should be considered, especially among patients with lower socioeconomic status [11]. Therefore, interventions to address transportation issues should carefully consider the demographic characteristics of the population.
Another noteworthy factor in our study was competing priorities, significantly associated with LTFU in bivariate analysis, although not in adjusted analysis. This includes work and childcare responsibilities. Work commitments have been cited as reasons for missed clinic appointments in diseases requiring long-term follow-ups, such as tuberculosis and HIV [17, 18], although another study reported no significant association between employment status and LTFU [19]. This is especially pertinent in resource-limited settings lacking social and financial support, where work often takes precedence over maintaining personal health [19]. Additionally, childcare responsibilities also present a barrier to attending clinic appointments, especially among female populations. This is worth noting, considering that a majority of RA patients, including participants in our study, were females. In lower-income households, utilization of childcare facilities may not be a feasible option, forcing them to rely on informal caregivers such as relatives or neighbours, scheduling their appointments during school hours, or bringing their children along to clinic appointments. The COVID-19 pandemic, however, has exacerbated this problem due to the visitor restriction policies imposed in hospitals and schools implementing remote-learning systems [20, 21]. This may result in patients cancelling or missing their appointments rather than leaving their children unattended. Interventions such as paid sick-leave and childcare assistance services may be considered to support these vulnerable populations and improve follow-up adherence.
Study limitations
Several limitations exist in this study. Our retrospective cohort design relied on the review of information not originally collected for research purposes, leading to potential missing data. This design also limits our ability to establish causality. Additionally, some patients could not be contacted, resulting in missing samples that may affect the results.
Conclusions
Transportation constraints and everyday busyness such as work and childcare were factors associated with LTFU. The second factor in particular was associated with the predominance of women in the study.
Further multivariate analysis showed that the transportation constraints were significantly associated with LTFU of RA patients.