Introduction
Rheumatic diseases are often associated with ophthalmic complications. Any part of the eyeball can be affected. The most common conditions include keratoconjunctivitis sicca, uveitis, scleritis and episcleritis, ischaemic retinopathy, optic neuropathy.
Keratoconjunctivitis sicca primarily involves the sense of having a foreign body under the eyelids and a sense of burning; however, photophobia and deterioration of visual acuity can also occur.
The vascular layer of the eye (the uvea) includes the iris, ciliary body and chorioidea. Depending on location, the anterior vascular layer (iridocyclitis), the intermediate portion (intermediate uveitis) and the posterior one (posterior chorioiditis) can be affected. Depending on the course of inflammation, uveitis can be divided into acute, subacute and chronic. Acute uveitis is characterized by a rapid onset and duration of up to 6 weeks. Chronic uveitis usually has an asymptomatic onset and lasts more than 3 months, sometimes many years [1].
Uveitis occurs at a rate of 38 per 100,000 individuals [2]. It is usually found in young people. In the majority of cases it is diagnosed in patients under the age of forty. Inflammation of the anterior segment of the vascular membrane is the most common form of vascular membrane inflammation (iridocyclitis is the most common form uveitis). In patients with the presence of the HLA-B27 acute anterior uveitis is usually found which is characterized by eye pain, redness, photophobia, epiphora and progressive deterioration of visual acuity. The palpebral fissure is narrowed, the eye is congested with intensive perilimbal hyperaemia and the pupil is narrow with a weak light reflex. Effusion appears in the anterior chamber.
The presence of the HLA-A29 is a predisposing factor for multifocal chorioiditis [2]. As many as 50% of cases of recurrent anterior uveitis are considered idiopathic since the underlying disease cannot be determined. However, this condition is considered to be the first sign of spondyloarthropathy preceding it by many years [3]. Other causes of anterior uveitis include herpes infection, sarcoidosis, toxoplasmosis, Behçet’s syndrome, multiple sclerosis or tuberculosis. Chronic uveitis with scarce symptoms occurs in children with juvenile idiopathic arthritis (JIA) [3].
Scleritis is associated with strong eyeball pain with associated conjunctiva and sclera redness, epiphora and photophobia. It is found primarily in young and middle-aged women. Nearly half of the cases of scleritis are associated with autoimmune diseases [4]. It is most often found in patients with rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA, formerly known as Wegener’s granulomatosis), spondyloarthropathies (SpA), polyarteritis nodosa (PAN), systemic lupus erythematosus (SLE). Other underlying causes of scleritis include bacterial, viral and parasitic infections. Scleritis can be anterior or posterior. Anterior scleritis occurs in three forms: diffuse (most common), nodular, necrotizing. Posterior scleritis is the least common form of the disease.
In the case of episcleritis the patient complains of a red eye, usually in the palpebral fissure on the nasal side [1, 4].
Vasculitis leads to the development of microinfarcts and ischaemic foci in the retina, which results in vascular oedema and angiogenesis in the retina, vitreous body haemorrhages and fibrosis as well as retinal detachment [1].
Optic neuropathy manifests itself as progressive deterioration of visual acuity, impaired colour vision and impaired pupillary light reflex [1].
Various visual complications are observed in different connective tissue diseases. However, there is a relationship between certain systemic diseases and a higher rate of some eye diseases.
Ocular involvement in rheumatic diseases
Rheumatoid arthritis is a chronic systemic connective tissue disease that affects the lining of the synovial joints, and also involving other organs; RA is usually associated with secondary dry eye syndrome as well as scleritis and episcleritis. The problem of dry eye occurs in 11% to 50% of patients with RA. Scleritis and episcleritis are the second most common ocular manifestation of RA. They can sometimes be prodromal symptoms, but they usually indicate the presence of active disease. Episcleritis occurs in approximately 5% of patients with RA and scleritis is found in 2% of these patients [5].
Retinal vasculitis has also been reported for RA patients. The optic nerve is less commonly affected in RA.
The second most common rheumatic disease and the one which is most commonly associated with visual involvement is Sjögren syndrome (SS). It is 9 times more common in women. It can occur at any age. The peak incidence is at 40 years of age. The dominant ocular symptoms are those associated with dry eye syndrome. It is the result of desquamation of corneal epithelium and bulbar conjunctiva. It occurs as a result of insufficient lacrimation and abnormal composition of the tears. Hyperosmolarity of tears is found in these patients. It manifests as eye pruritus, foreign body sensation, burning and pain. Patients can also complain of sunlight hypersensitivity, eye fatigue, redness and fluctuating visual acuity. Symptoms exacerbate as a result of low moisture level, tobacco smoke exposure, anticholinergics or antihistamines.
Complaints develop slowly and are variable, which makes diagnosis difficult. Therefore, it is estimated that the disease remains undiagnosed in half of the affected adult population. Data suggest that diagnosis is delayed by approximately 3.9 years [6–8].
Spondyloarthropathies are often complicated by uveitis. In ankylosing spondylitis (AS) the anterior part of the uvea is most often affected; in psoriatic arthritis (PsA) anterior or posterior uveitis occurs, while in reactive arthritis (ReA) iritis is found.
It is estimated on the basis of the available literature that from 20 to 40% of patients with ankylosing spondylitis have a history of acute anterior uveitis. The posterior part of the uvea is less frequently affected. In patients with psoriatic arthritis uveitis occurred at a rate of approximately 25%. In over 80% of cases uveitis has an acute course and in over 90% the anterior portion of the eye is affected. Bilateral inflammation has been reported in as many as 80% of patients with spondyloarthropathies and recurrent inflammation in approximately 50% [9–11].
In chronic uveitis the following complications can occur, particularly in patients with the HLA-B27: pupillary block with secondary filtration angle closure, visual acuity deterioration, cataract, secondary glaucoma, macular oedema. Prolonged and uncontrolled anterior uveitis is a risk factor for the transfer of inflammation to the posterior portion of the eye [9–11].
Reactive arthritis occurs 1–6 weeks after an infection, usually a genitourinary or gastrointestinal tract infection. The main pathogens include Chlamydia trachomatis, Yersinia, Salmonella, Shigella and Campylobacter. Following the onset of urinary or gastrointestinal tract infection symptoms articular and ocular complaints occur. Conjunctivitis occurs most frequently and iritis is less common. Conjunctivitis is particularly frequently induced by Chlamydia and occurs within the first few days from the infection. It is often painless and non-specific, but can cause burning and irritation of the eyes. It occurs in 2% of patients with acute ReA and in approximately 96% of patients with chronic disease. It is estimated that ReA can become chronic in 30–50% of patients. Iritis is less common. It affects 10–20% of patients with ReA who have the HLA-B27 [12, 13].
Ocular problems affect approximately 20–30% of patients with SLE. Keratoconjunctivitis sicca is the most common one. Various data indicate that they occur at a rate of 9 to 25% of patients.
In patients with active SLE the retina is often involved (29%) and lesions similar to diabetic or hypertensive microangiopathy frequently occur. The presence of antiphospholipid antibodies is found in the majority of these patients. Scleritis and episcleritis occur in approximately 2.4% of adult patients with SLE [14–17].
Optic nerve involvement is less common. It usually occurs in the form of inflammation or anterior ischemic optic neuropathy. It is associated with serious visual impairment and only early glucocorticosteroids treatment gives a chance for improvement. Ocular vascular thrombosis is a rarely diagnosed but serious eye condition associated with SLE. The consequences of vascular occlusion and the development of collateral circulation include vitreous body hemorrhages, retinal detachment and post-thrombotic glaucoma [14–17].
As a result of the procoagulatory activity of antiphospholipid antibodies associated with antiphospholipid syndrome (APS) thrombosis can be observed in the vessels of various organs, including the eyes. The most common ocular manifestations of APS are those of retinal vascular thrombosis, particularly in young individuals. It is estimated that ocular complications occur in 14–18% of patients.
Abnormalities which may occur in the anterior portion of the eye include telangiectasias, microaneurysms, episcleritis, scleritis and keratitis. The most common ocular manifestation of APS located in the anterior portion of the eye is superficial punctate keratitis. Scleritis occurs in over 45% of patients. Anterior scleritis is most commonly observed. The posterior portion of the eye is involved in as many as 76% of APS patients. Retinal vasculitis, vitreous body inflammation and, less commonly, retinal detachment or posterior keratitis are usually diagnosed.
Antiphospholipid syndrome can also be associated with optic neuropathy, usually unilateral, which can occur in the form of anterior ischaemic optic neuropathy or retrobulbar optic neuritis [18, 19].
To date a few reports of ocular abnormalities in patients with systemic sclerosis (SSc) and a number of studies on small groups of patients have been presented. Dry eye syndrome is the most common ocular complication in SSc. It is the consequence of lacrimal gland fibrosis as well as chronic blepharitis and Meibomian gland dysfunction. Retinopathy and maculopathy are less common. In 29–65% of patients with SSc eyelid skin sclerosis occurs, which leads to the inability to close the eyelids completely (lagophthalmos) or to the narrowing of the eyelid fissure (blepharophimosis). Cases of blepharitis or degenerative proliferation of bulbar conjunctiva (pterygium) have also been reported. Single cases of recurrent uveitis have been reported. Literature data show that over 30% of patients with SSc develop chorioidal perfusion disorders [16, 20–22].
Multiple muscular and cutaneo-muscular inflammation can be complicated with keratoconjunctivitis sicca, less commonly with retinopathy. Cases of iritis, episcleritis and chorioiditis have also been reported [16, 23, 24].
The antineutrophil cytoplasmic antibody (ANCA)- associated vasculitides (AAV) are a necrotising inflammation of small vessels including primarily interstitial arteries, arterioles, capillaries and venules associated with the presence of antibodies against neutrophil cytoplasm. ANCA-associated vasculitis covers three syndromes: GPA, eosinophilic granulomatosis with polyangiitis (EGPA, formerly known as Churg-Strauss syndrome) and microscopic polyangiitis (MPA). Ocular complications occur in 50–60% of patients in AAV, usually in GPA. It is estimated that 29–52% of GPA patients have ocular complications. The anterior portion of the eye is usually affected, usually by scleritis and less commonly by ulceration or orbital pseudotumour. Lesions in the posterior part of the eye, such as retinal vasculitis or optic neuropathy were less frequently reported [25, 26].
Giant cell arteritis (GCA) is characterised by the presence of inflammatory infiltration and T CD4 cell granulomas, macrophages and multinucleated cells in the walls of large and medium-sized arteries leading to their segmental stenosis and, consequently, tissue ischaemia [27, 28]. Visual impairment occurs in 25–50% of giant cell arteritis patients. The most commonly reported complication is vision loss as a result of optic nerve ischaemia. Uveitis as a manifestation of posterior ciliary artery ischaemia is less common [29, 30].
Takayasu arteritis (TAK) is a chronic inflammation of large vessels particularly of the aorta and its branches, less commonly of other arteries. Ophthalmic symptoms are relatively rare in TAK. As a result of aortic arch branches being affected by the disease, an individual develops ischaemia-related visual impairment. If the disease affects renal arteries, severe, uncontrolled arterial hypertension develops, which leads to visual complications. Takayasu arteritis is usually reported to be associated with retinopathy. Other manifestations such anterior ischaemic optic neuropathy or central retinal artery occlusion are less commonly reported [29, 30].
Behçet’s disease is a chronic disease characterised by periods of exacerbations and remissions. It occurs at a similar rate in women and in men. First symptoms occur between 20 and 35 years of age. Behçet’s disease is an inflammatory disease of blood vessels. Ophthalmic symptoms occur in as many as 70% of these patients. The conjunctivas, sclera, vitreous body and retina can be involved. Bilateral acute non-granulomatous iritis, often with purulent effusion in the anterior chamber, is usually observed. The disease is chronic and can lead to multiple complications [31, 32].
Juvenile idiopathic arthritis is the most common rheumatic disease of the young age. It is diagnosed up to 16 years of age. In oligoarticular JIA approximately 20% of patients develop uveitis. Even higher rates (up to 85%) are observed in the female population with single-joint disease and the presence of antinuclear antibodies (ANA). The risk factors for uveitis in JIA include female sex, early age of onset, the presence of plasma antinuclear antibodies and rheumatoid factor (RF) – negative disease. Children with chronic anterior uveitis usually display no symptoms. For this reason, it is imperative to actively search for the symptoms of the disease and perform preventative eye examinations.
Uveitis associated with JIA is usually bilateral, without signs of granulation, chronic and recurrent. It may lead to complications such as band keratopathy, cataract, posterior adhesions, glaucoma or maculopathy [33, 34].
Special attention should be given to eye symptoms, which are an indication for urgent ophthalmological consultation, authors analyzed available literature in this subject and ocular disorders considered as associated with rheumatic diseases are summarized in Table I [1–34].
Table I
Some eye conditions can result from the use of medications in the treatment of rheumatic diseases. Chronic glucocorticosteroid therapy leads to cataracts, while maculopathy is associated with the use of antimalarial drugs. Long-term use of non-steroidal anti-inflammatory drugs can lead to keratopathy, methotrexate can cause punctate keratopathy, and D-penicillamine can lead to optic neuropathy [35].
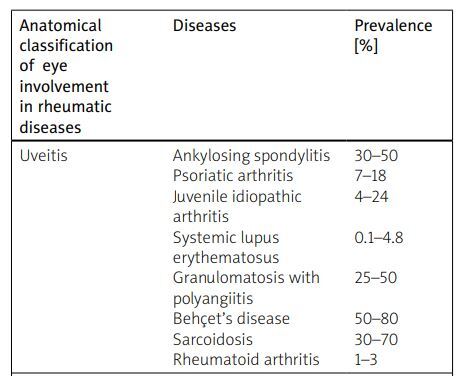
The anatomical classification of eye involvement with prevalence of specific changes in rheumatic diseases according to data from analyzed literature is summarized in Table II [36–57].
Table II
Conclusion
Rheumatic diseases are often associated with ophthalmic complications; however, ophthalmic symptoms often precede rheumatic symptoms. Special attention should be given to symptoms related to the visual system, such as pain, sensitivity to light, tearing, redness of the eye, sudden deterioration of visual acuity, which require urgent ophthalmological consultation. For this reason, cooperation between rheumatologists and ophthalmologists as well as vigilance and active search for rheumatic diseases in patients with ocular abnormalities is so important.