Introduction
Diabetes mellitus (DM), a chronic metabolic disorder associated with abnormal glucose homeostasis resulting in high blood glucose (hyperglycemia), is a growing public health problem causing a significant amount of disability and mortality [1]. The global prevalence of DM among adults aged 20–79 years was estimated at 10.5% (536.6 million people) in 2021.
This figure is projected to rise to 12.2% (783.2 million people) by 2045 [2]. The burden of DM is particularly worrying in low- and middle-income countries as most people (over 3 in 4) with the disease live in these regions [1].
The prevalence of DM in Nigeria was found to be 5.8% (11.2 million people) [3] with an estimated mortality rate of 30.2 per 100,000 population [4]. Currently, the International Diabetes Federation, based on extrapolated data, ranked Nigeria as the second top African country with the highest number of people with DM (3.6 million) [1] suggesting that Nigerians are likely to suffer the greatest burdens of DM [5].
Diabetes mellitus is a serious disease that adversely affects a person’s daily life, emotional well-being, productivity, and quality of life due to its chronic nature. It is associated with debilitating and life-threatening complications, among which include musculoskeletal disorders (MSDs).
Diabetic individuals are more likely to develop MSDs than those without DM, but these complications have been often unrecognized, underappreciated, and poorly treated in contrast to other complications like retinopathy, neuropathy, and nephropathy causing various disabilities [6–8].
According to a previous systematic review and meta-analysis, the prevalence of all types of MSDs among diabetic individuals was 58.2%, with the hand (33.1%) being the most commonly affected body part followed by the shoulder (32%) [9]. The most commonly reported MSDs in DM are limited joint mobility, flexor tenosynovitis, carpel tunnel syndrome, Dupuytren’s contracture, frozen shoulder, and osteoarthritis [10, 11].
Musculoskeletal disorders among DM patients have been linked with the duration of the disease, age of the patient, lack of formal education, impaired metabolic control, and the existence of microvascular complications [7, 12, 13]. Although the exact pathogenesis of MSDs in DM is not fully understood as they may also be due to some personal, occupational, or psychological factors [12], metabolic disturbances such as increased protein glycosylation, decreased collagen degradation, microangiopathy, and neuropathy are believed to be important attributing factors [14].
More specifically, higher glycosylation of collagen in the skin and periarticular tissue may alter extracellular matrix structure and function, causing inflammation and subsequently leading to progressive joint pain and stiffness [12, 15]. Additionally, factors such as obesity and advanced aging in individuals with type 2 DM may lead to excess joint loading causing MSDs [15].
Studies on the prevalence of MSDs among diabetics are mostly conducted in developed countries. There are variations in culture and environment in Africa in terms of the environment and food consumed.
Considering the high prevalence of DM in Nigeria, local studies will provide healthcare professionals and policymakers with insight into the appropriate measures to put in place to reduce the burden associated with DM-related MSDs and improve the health outcomes of people with this condition. It is worth noting that a few studies on the prevalence of MSDs and their associated factors were conducted in Nigeria [7, 16–18].
However, these studies were largely conducted in southern Nigeria and there is a dearth of studies in northern Nigeria. Due to the cultural diversity between southern and northern Nigeria, it would be important to conduct a similar study in northern Nigeria to have data that can be extrapolated.
Thus, this study determined the prevalence of MSDs and their associated factors among individuals with DM attending a diabetic clinic of Ahmadu Bello University Teaching Hospital (ABUTH), northwest, Nigeria.
Material and methods
Study population
A retrospective cross-sectional survey of medical case records of all consecutive diabetic patients attending the diabetic clinic, Department of Internal Medicine, ABUTH between February 2015 and September 2021 was conducted.
Ahmadu Bello University Teaching Hospital, located in Shika, Zaria town, Giwa Local Government Authority, is the largest public hospital with a 1,000-bed capacity. The hospital provides tertiary-level healthcare services to millions of patients in northwest Nigeria. The hospital has general clinics and different specialties for follow-up of chronic diseases such as DM.
Patients with DM presenting with any musculoskeletal complaints such as joint pain during activity or at rest, tenderness, swollen joints and stiffness, and reduced activity were included.
However, those with a history of trauma-related MSD, history of previous surgery, known endocrine disorders such as thyroid disorder, neurological conditions such as stroke, chronic kidney disease, mental and visual disorders, and pregnancy were excluded.
Because this study is a retrospective analysis of medical records of patients, no formal sample size calculation was performed. Patients’ detailed information was obtained from their hospital folders at the diabetic clinic of ABUTH, Zaria, Kaduna State. A researcher-designed questionnaire was used to collect data and it consists of two sections.
The first section was used to record participants’ sociodemographic variables such as age, sex, occupational status, height, weight, and body mass index (BMI) and clinical variables such as type of DM, duration of DM, two-hour postprandial, glycated hemoglobin (HbA1c), and presence of comorbidity.
The second part of the questionnaire was used to record the presence and pattern of MSDs. All patients with complaints of MSD were examined by either a rheumatologist or an orthopedic surgeon.
Clinical diagnoses were made through standardized physical examination and the use of radiological (plain radiographs) and laboratory investigations where necessary. Physical examination included general inspection, palpations, assessment of active and passive joint range of motion, and specific provocative maneuvers.
Radiological assessments such as plain radiographs for degenerative conditions, such as osteoarthritis or spondylosis, were performed. Laboratory investigations for two-hour postprandial and HbA1c in the participants’ case notes were carried out by collecting venous blood samples using standard techniques.
The following operational definitions were used for the diagnosis of some MSDs:
Cervical spondylosis was considered if pain experienced in the cervical region was reported for at least 12 weeks duration, including seasonal or recurrent episodes, with evidence of radiological features such as osteophytes, intervertebral disc space narrowing, and vertebral sclerosis on X-ray.
Frozen shoulder or adhesive capsulitis: this was identified by painful restriction of the shoulder joint on passive and active in at least three planes of less than 50%, having unilateral shoulder pain > 4 weeks, and inability to lie on the affected shoulder [6, 19].
Flexor tenosynovitis or trigger finger: this was identified by palpating a nodule or thickened flexor tendon with a locking phenomenon during finger flexion or extension [6, 20].
Depuytren’s contracture: this was identified by the presence of thickening of the palmar of the hand with firm, painless nodules, and flexion contracture of the ring and little finger [19, 21].
Carpal tunnel syndrome: this was identified by the presence of pain, paraesthesia, or weakness in the hand, evidence of thenar atrophy, and or a positive Tinel’s or Phalen’s sign [19, 21].
Lumbosacral spondylosis: this was considered if pain, stiffness, or discomfort in the lumbar spine, buttock, and thigh area were reported for at least 12 weeks duration including seasonal or recurrent episodes, with evidence of radiological features such as osteophytes, intervertebral disc space narrowing and vertebral sclerosis on X-ray [11].
Knee osteoarthritis: this was identified by the presence of pain or stiffness around the knee on waking up from sleep or after activity, swelling, or crepitation; evidence of radiological features such as osteophytes, reduced joint space, subchondral sclerosis, and cysts on X-ray [11, 22].
Multisite MSDs: if there is the presence of more than one type of MSD.
Overall MSDs: if one or more of the aforementioned MSDs are present (Yes) [21].
Statistical analysis
Descriptive statistical analysis in the form of mean (standard deviation – SD) was carried out for continuous variables, and frequency (percentages) for categorical variables. A Bar chart was used to present the prevalence and pattern of MSDs. Univariable logistic regression was applied to identify association between overall MSDs (dependent or outcome variable) with each independent or predictor variable (sociodemographic and clinical characteristics).
Variables with p ≤ 0.25 [23] in the univariable analysis were entered into a multivariable logistic regression model to examine the contribution of each of the predictor variables to the outcome variable while handling the effect of possible confounders.
To reflect the strength of each relationship, data for the univariable logistic regression analyses were presented as crude odds ratio (OR) and corresponding 95% confidence intervals (CI) while adjusted odds ratio (AOR) and corresponding 95% CI were presented for the multivariable logistic regression analyses.
Separate regression models were also computed for each of the most prevalent MSDs. The model fit was checked using the likelihood ratio test and the Hosmer-Lemeshow test. All data analyses were performed with the use of SPSS version 23.0 (IBM Co., Armonk, NY, USA).
Results
Four hundred eighty cases of patients with DM were analysed. The mean age of the participants was 51.4 ±12.3 years, with 72% of them within the range of 40 to 64 years of age. Two-thirds of the participants were females (65.2%) and had normal BMI (67.3%) (Table I).
Table I
Sociodemographic characteristics of the patients
The majority of the participants had type 2 DM (96.7%) with a mean DM duration of 7.02 ±5.05 years. The available recent HbA1c levels were within the normal target (3.77%) but based on the data of 39 participants. Additionally two participants had no data on two-hour postprandial. Details of the participants’ socio-demographic and clinical characteristics are shown in Tables I and II, respectively.
Table II
Clinical characteristics of the patients
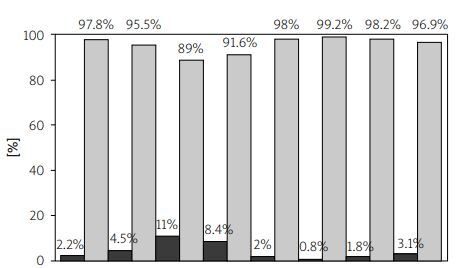
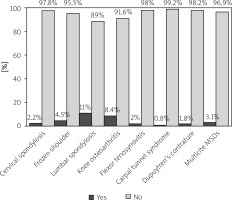
Overall, the prevalence of MSDs among the participants was 32.7% (n = 160). As shown in Figure 1, the highest prevalence was found for lumbosacral spondylosis (11%), followed by knee osteoarthritis (8.4%). The prevalence rates of cervical spondylosis, frozen shoulder, flexor tenosynovitis, carpal tunnel syndrome, and Dupuytren’s contracture were 2.2%, 4.5%, 2%, 0.8%, and 1.8%, respectively. About 3.1% of the participants had multisite MSDs.
Results of the univariable logistic regression showed a significant association between overall prevalence of MSDs and age, sex, BMI, and duration of DM (Table III). A one-year increase in age was associated with a 23% prevalence of MSDs (OR: 1.023, 95% CI: 1.00–1.04), and participants aged 65 years or above were more likely to be affected (OR: 2.39, 95% CI: 1.11–5.12) compared to those aged ≤ 39 years. Similarly, females were more likely to have one or more MSDs (OR: 1.57, 95% CI: 1.04–2.36) compared to males.
Table III
Association of overall musculoskeletal disorders with selected sociodemographic and clinical variables using univariable logistic regression
| MSDs | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Mean (SD) | No (%) | Yes | No | p-value | OR | Lower | Upper |
| Sociodemographic variables | ||||||||
| Age | 51.4 (12.3) | 0.005** | 1.023 | 1.00 | 1.04 | |||
| ≤ 39 years | 66 (13.6) | 13 | 53 | Reference | ||||
| 40–64 years | 352 (72.3) | 132 | 220 | 0.056 | 1.85 | 0.98 | 3.47 | |
| ≥ 65 years | 69 (14.2) | 27 | 42 | 0.025* | 2.39 | 1.11 | 5.12 | |
| Sex | ||||||||
| Male | 170 (34.8) | 46 | 124 | Reference | ||||
| Female | 319 (65.2) | 127 | 192 | 0.032* | 1.57 | 1.04 | 2.36 | |
| Occupational status | ||||||||
| Housewife | 206 (42.1) | 81 | 125 | Reference | ||||
| Retiree | 30 (6.1) | 9 | 21 | 0.854 | 1.08 | 0.49 | 2.39 | |
| Paid work | 101 (20.7) | 41 | 60 | 0.905 | 1.03 | 0.63 | 1.69 | |
| Self-employed | 127 (26.0) | 37 | 90 | 0.212 | 0.74 | 0.46 | 1.19 | |
| Student | 25 (5.1) | 5 | 20 | 0.140 | 0.47 | 0.17 | 1.29 | |
| Body mass index | 23.3 (4.74) | 0.000*** | 1.09 | 1.05 | 1.14 | |||
| Normal | 329 (67.3) | 100 | 229 | Reference | ||||
| Overweight | 114 (23.3) | 48 | 66 | 0.007** | 1.85 | 1.19 | 2.89 | |
| Obese | 46 (9.4) | 25 | 21 | 0.002** | 3.56 | 1.89 | 6.69 | |
| Clinical variables | ||||||||
| Two-hour post-prandial | 13.8 (9.56) | 0.33 | 1.01 | 0.99 | 1.03 | |||
| Duration of DM | ||||||||
| ≤ 5 years | 223 (45.9) | 67 | 156 | Reference | ||||
| 6–10 years | 169 (34.8) | 55 | 114 | 0.825 | 1.05 | 0.68 | 1.63 | |
| ≥ 11 years | 94 (19.3) | 50 | 44 | 0.003** | 2.14 | 1.30 | 3.52 | |
| Type of DM | ||||||||
| Type 1 | 16 (3.3) | 3 | 13 | Reference | ||||
| Type 2 | 473 (96.7) | 170 | 303 | 0.051 | 7.59 | 0.99 | 58.0 | |
| Comorbid | ||||||||
| Absence | 293 (59.9) | 95 | 198 | Reference | ||||
| Presence | 196 (40.1) | 65 | 131 | 0.864 | 1.04 | 0.70 | 1.52 |
A unit increase in overall BMI leads to a 9% increase in odds of having one or more MSD, and obese participants were more likely to be affected (OR: 3.56, 95% CI: 1.89–6.69) compared to participants with normal body weight. Furthermore, participants who had 11 years or above duration of DM were more likely to experience one or more MSDs (OR: 2.14, 95% CI: 1.30–3.52) compared to patients who had 5 years or less of duration of DM (Table III).
For the association between most prevalent MSD and potential predictors, only lumbosacral spondylosis was found to be significantly associated with BMI and duration of DM. A unit increase in overall BMI leads to an 8.2% increase in the odds of having lumbosacral spondylosis.
Obese participants were more likely to have lumbosacral spondylosis (OR: 4.59, 95% CI: 2.15–9.78) compared to participants with normal body weight. Participants who had 6 to 10 years duration of DM were more likely to have lumbosacral spondylosis (OR: 1.97, 95% CI: 1.03–3.78) compared to those who had 5 years or less of duration of DM.
No significant association (p > 0.05) was observed between other most prevalent MSDs (i.e. knee osteoarthritis and frozen shoulder) and any of the potential predictors.
When all variables were adjusted for, only duration of DM was retained in the multivariable logistic regression model (Table IV). The model explained 81% variance (adjusted R2 = 0.810) in the risk of MSDs and was able to identify 67% cases accurately.
Table IV
Association of overall musculoskeletal disorders with selected sociodemographic and clinical variables using multivariable logistic regression
| MSDs | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Mean (SD) | No (%) | Yes | No | p-value | AOR | Lower | Upper |
| Sociodemographic variables | ||||||||
| Age | 51.4 (12.3) | 0.307 | 1.107 | 0.99 | 2.34 | |||
| ≤ 39 years | 66 (13.6) | 13 | 53 | Reference | ||||
| 40–64 years | 352 (72.3) | 132 | 220 | 0.865 | 1.08 | 0.44 | 2.65 | |
| ≥ 65 years | 69 (14.2) | 27 | 42 | 0.870 | 0.89 | 0.21 | 3.72 | |
| Sex | ||||||||
| Male | 170 (34.8) | 46 | 124 | Reference | ||||
| Female | 319 (65.2) | 127 | 192 | 0.059 | 1.52 | 0.99 | 2.34 | |
| Body mass index | 23.3 (4.74) | 0.152 | 1.07 | 0.98 | 1.16 | |||
| Normal | 329 (67.3) | 100 | 229 | Reference | ||||
| Overweight | 114 (23.3) | 48 | 66 | 0.677 | 1.16 | 0.57 | 2.37 | |
| Obese | 46 (9.4) | 25 | 21 | 0.404 | 1.68 | 0.49 | 5.65 | |
| Clinical variables | ||||||||
| Duration of DM | ||||||||
| ≤ 5 years | 223 (45.9) | 67 | 156 | Reference | ||||
| 6–10 years | 169 (34.8) | 55 | 114 | 0.842 | 0.95 | 0.60 | 1.52 | |
| ≥ 11 years | 94 (19.3) | 50 | 44 | 0.035* | 1.76 | 1.04 | 2.99 | |
| Type of DM | ||||||||
| Type 1 | 16 (3.3) | 3 | 13 | Reference | ||||
| Type 2 | 473 (96.7) | 170 | 303 | 0.173 | 5.06 | 0.49 | 52.3 |
The results showed that for every additional year with DM, the odds of having one or more MSDs is 76% (AOR: 1.76, 95% CI: 1.04–2.99; p = 0.035). However, the association between MSDs and age, sex, BMI, and type of DM disappeared (Table IV).
Similar to the univariable logistic regression model for the association between lumbosacral spondylosis and potential predictors, the multivariable logistic regression model retained BMI and duration of DM as predictors. Obese participants were more likely to have lumbosacral spondylosis (AOR: 7.461, 95% CI: 1.33–43.8; p = 0.023) compared to those with normal body weight.
Participants who had ≥ 11 years duration of DM were more likely to have lumbosacral spondylosis (AOR: 2.64, 95% CI: 1.19–5.89; p = 0.018) compared to those who had 5 years or less of duration of DM.
Discussion
The present study aimed to determine the prevalence of MSDs and their associated factors among individuals with DM in northwest Nigeria. From the demographical point of view, we found that individuals aged 40–64 years are commonly affected by DM, with the majority of them (96.7%) having type 2 DM, which is incongruent with the literature [24].
Additionally, females were more affected by DM compared to males, which is not in harmony with findings of the global estimates indicating that DM prevalence is similar in men and women. Nevertheless, the sex disproportionality in our study could be partly explained by the fact that a plurality of the participants were housewives.
Although physical activity level was not assessed in our study, it is believed that housewives or married women, especially those living in urban Nigerian settings are less physically active [25] as they are often indoors, thus are more at risk of developing obesity and subsequently type 2 DM. On the other hand, being physically active is associated with reduced odds of having MSD [26].
While several studies from different parts of the world have determined the prevalence of MSDs among diabetic individuals, most of these studies, however, focused on individual components, particularly upper extremity disorders [21, 27–31]. Our study, on the other hand, evaluated the prevalence of a wide range of MSDs involving both upper and lower limb extremities akin to the study by Olaosebikan et al. [7] conducted in southwest Nigeria.
We found the overall prevalence of MSDs to be 32.7%, which is higher than the prevalence rates reported in Netherlands (16.3%) [31], Saudi Arabia (17.9%) [6], and Ethiopia (24%) [21], but lower compared to those reported in southwest Nigeria (54%) [7], India (42.6%) [19], Canada (66%) [32], and Iran (83.5%) [33]. Individuals with type 2 DM were more affected than those with type 1 (33.6% vs. 6.3%). It is believed that those with type 2 DM are more prone to develop MSDs due to factors such as obesity, older age, decreased physical activity, and dyslipidemia [7].
Among the different MSDs investigated, we found lumbosacral spondylosis (11%) to be the most prevalent disorder followed by knee osteoarthritis (8.4%). This is in harmony with the results of previous studies suggesting that degenerative joint disorders were more common than inflammatory and other conditions among patients with DM [34, 35].
In contrast, most studies reported upper extremity disorders affecting the hand or shoulder to be the most prevalent disorder among patients with DM [6, 10, 21, 31]. Notwithstanding, the findings that lumbosacral and knee regions were commonly affected in our study could be attributed to the fact that the joints of these regions support most weight of the body (i.e. weight-bearing joints) thus, a higher prevalence of MSDs is expected.
The differences in the pattern of affectation of MSDs across studies could be attributed to the different methods used by researchers to determine the prevalence of MSDs and their distribution besides differences in socioeconomic, lifestyle, and cultural factors among populations [21].
The present study found age, sex, BMI, and duration of DM to be potential predictors of having one or more MSDs. In particular, BMI and duration of DM were associated with lumbosacral spondylosis. However, when all the predictors were included in the adjusted regression model to account for conpounding effect, only duration of DM became a significant predictor of overall MSDs whereas both duration of DM and BMI became significant predictors of lumbosacral spondylosis.
Individuals living with DM for 11 years or more were more at risk of developing lumbosacral spondylosis compared to those living with DM for less than or equal to 5 years. It could be hypothesized that as the duration of living with DM increases, so also musculoskeletal degeneration progresses [21].
Another plausible explanation is that a longer duration of DM may be accompanied by persistent hyperglycemia, which is believed to induce chronic inflammation and consequently joint degeneration and pain [15]. In line with our study, previous studies conducted in Ethiopia [21], India [19], and Turkey [36] found the duration of DM to be a predictor of MSDs among diabetics.
The finding of our study that obese diabetics have increasing odds of having MSDs, particularly lumbosacral spondylosis affirms the relationship between obesity and the development of MSDs in the lower back and knee joints. It is assumed that excess body weight induces abnormal joint loads leading to biomechanical alterations of the intervertebral discs and subsequent inflammation and pain [37].
Moreover, excessive joint loading and hyperglycemia are linked to osteoarthritis, causing excess glucose accumulation producing advanced glycation end products (AGEs), oxidative stress triggering cartilage degradation, osteophyte development, and subchondral bone sclerosis [38].
In contrast to the findings of our study, previous researchers have found factors such as age, sex, education level, and occupational status as significant predictors of MSDs in their final model [19, 21, 32, 36].
The lack of association of MSDs with age in our study may be explained by its association with the outcome variable, hence a potential conpounding variable as verified by the adjusted model. In addition, the majority of our population (72%) were within the age range of 40–64 years, thus their preponderance may have influenced the results. Similarly, the fact that our data was more skewed to the female sex (62.2%) may also explain the lack of association between MSDs and sex.
However, in agreement with our study, other studies [39, 40] did not support the association between sex and MSD, which could be assumed that both males and females are equally afflicted. Instinctively, the lack of association of MSD with education level and occupational status in our study could be partly due to decreased statistical power, as a result of some categories with small sample size.
The cross-sectional study of data of patients from one of the largest tertiary health institutions in northwest Nigeria constitutes the strength of our study. We reported a wide variety of MSDs affecting both the upper and lower limbs, unlike the reports of most epidemiological studies that focus on disorders of the upper limb. Moreover, significant predictors in univariable analyses were adjusted in multivariable analyses to control the effect of compounding variables. However, other authors did not report adjusted models in their studies [7].
Study limitations
Our study is not without certain potential limitations. First, the study lacks a comparative or control group and there were a few missing clinical data. Second, the cross-sectional design of the present study limits the establishment of temporal relationships between the examined predictors and MSDs.
Third, our study sample was recruited from a single health center and not a random sample of the overall population, thus limiting to some extent the extrapolation of the study findings. Lastly, the retrospective design could not allow us to retrieve other vital patient information. For example, data on lifestyle characteristics such as physical activity, smoking status and alcohol use, would have been useful if included in the data analyses.
Conclusions
Approximately one-third of the study participants had MSDs, with lumbosacral spondylosis being the most frequently occurring disorder. Being obese and having a longer duration of DM were significantly associated with MSDs. It is recommended that clinicians should pay attention to MSDs and their influencing factors in DM patients by conducting routine assessments and implementing early treatment.